A Comprehensive 360˚ Philanthropic Support Model: Holistic and Sustainable Approaches to Childhood Cancers (0–19 years) in a Tertiary Cancer Hospital in India
Download
Abstract
Background: In low- and middle-income countries (LMICs), childhood cancer care is often compromised by financial and logistical barriers, with many families unable to afford life-saving treatment. At Rajiv Gandhi Cancer Institute and Research Centre (RGCIRC), New Delhi, we envisioned a solution: a 360˚ philanthropic support model that ensures no child is denied treatment due to lack of funds.
Objective: This study aims to describe the structure and impact of the comprehensive philanthropic care model at RGCIRC and to evaluate financial support provided to pediatric cancer patients between 2021 and 2023.
Methods: Data were retrospectively analyzed from hospital records for all pediatric oncology cases treated from 2021 to 2023. Financial support was tracked across sources government schemes, private insurance, NGO funding, and corporate social responsibility (CSR) contributions. Additional support services such as accommodation, education during treatment, and long-term follow-up were assessed through hospital departments.
Results: Out of 1,098 pediatric patients, 997 (90.84%) received financial aid. Annual financial support rose from INR 4.38 crores in 2021 to INR 7.8 crores in 2023, with philanthropic contributions increasing from 71.6% to 78.7%. Beyond monetary aid, children received emotional and academic support, stay facilities at the hospital’s “Grace” home, and long-term survivorship care through dedicated ACT (After Completion Therapy) clinics forming a robust safety net around each child.
Conclusion: RGCIRC’s 360˚ philanthropic model redefines pediatric cancer care in LMICs by combining financial, emotional, educational, and post-treatment support. Its success underscores the power of multi-sector partnerships and offers a replicable blueprint for other institutions seeking to bridge care gaps and improve survival and quality of life for children battling cancer.
Introduction
All the types of cancers that occur in children and adolescents with individual age range from 0-19 years came under the pediatric cancers. To develop effective health care strategies, we need to understand its types, incidence, and challenges associated with it. The most common sites include Leukemia, Central nervous system tumor and Lymphomas. While other sites also include Neuroblastoma, Wilms tumor (nephroblastoma), Rhabdomyosarcoma, Retinoblastoma, Osteosarcoma and Ewing sarcoma and soft tissue sarcomas. In lower-middle income countries the rates of pediatric cancer under diagnosis and under-registration are significantly higher which results in the delaying of treatment and less data availability for continuous research. Studies has shown that more than 80% of pediatric patients who are treated with modern techniques are cured but unfortunately these treatment options are majorly available to developed countries where pediatric patients count is only 20% of the total in world [1]. When a child is diagnosed with the cancer it is the whole family which has to go through a cycle of psychological stress which in severe cases can turn into post-traumatic stress disorder, the whole family structure is sometimes degraded affecting the mental health of father and mother [2]. According to the report of press information bureau India’s per capita Net National Income is Rs. 98,374 in 2022-23 and average cancer treatment cost in India is INR Rs.5,00,000 This high gap of financial resources cannot be filled overnight in a large diverse country like India, thus helping the needy (core of philanthropy) is what keeps Indian population stable. Considering the report of NCRP, cancer cases are estimated to increase by 12.8 per cent in 2025 as compared to 2020. Hence, it becomes a crucial responsibility to maintain and grow society’s philanthropic needs and the financial power of families to decrease the burden on the nation’s philanthropic pillars.
In 2022, more than 275 000 children and adolescents (aged 0–19 years) were diagnosed with cancer worldwide and more than 105 000 children died from cancer [3]. While in India, total annual cases of pediatric cancer (ages 0-19 years) were 76,805 [4]. The further estimates shows that leukemia and Central nervous system tumors as the most common cancer sites in India with an average burden of 53%, other sites includes lymphomas (10.8%), retinoblastoma (3.2%), renal tumors (5.8%), hepatic tumors (1.6%), bone tumors (4%), Soft tissues sarcomas (6.4%), germ cell tumors(3.5%), epithelial tumors (3.3%) and other types (<1%) [4].
Psychological and financial burden of pediatric cancer
Financial burden major contributors are cost of treatment, loss of parent income, Cost of stay, and unawareness of financial support programs. Studies have shown that the risk of clinical depression, anxiety and inferior quality of life increases in parents after cancer diagnosis in family because of multiple reasons like lack of knowledge about cancer, uncertain financial status and continuous negative thoughts which leaves the family in a feeling of helpless environment without any hope [5]. As a result, development of posttraumatic stress disorder in parents is also seen, siblings may feel lost because of lack of attention by parents pushing them to the same mental health crisis with their parents.
Government hospital status in India
Indian government hospitals are operating with their primary focus on the affordability and accessibility of cancer treatment and care. While the existence of a government health care system is essential to the lower-middle income countries, their efficiency is always a subject of improvement. Many government cancer centers often have inadequate basic clinical resources and treatment modalities comparing to the large patient population of India. Many studies have highlighted that standard anti-cancer therapies are significantly low in countries like India especially in public hospitals [6]. Considering the geographical data, almost 60% of special cancer hospitals are in south and west parts of India. Whereas regions like northeast which have high cancer rates have shortage of cancer treatment facilities, this results in the delay of the treatment which can cause increase in the extent of cancer making it more operationally tough. The wait time for treatment is stretched many times especially for radiotherapy, because of the shortage of linear accelerators in the hospital. In India the number of oncologist available are very less than the growing number of cancer cases which has resulted in the lack of availability of oncologist for clinical research and making the research and innovation work on treatment and diagnosis more difficult and delayed.
1. RGCIRC’ Philanthropic strategy to tackle pediatric cancer care
1.1 Expanding Patient Welfare Schemes: Each year, we introduce new schemes to broaden the scope of support available to patients, ensuring that evolving needs are met and that our support remains relevant and effective.
1.2 Elevating Fundraising Endeavors: Over the past three years, our fundraising efforts have significantly increased, with funds rising from 4.38 crores to 7.8 crores. This growth enables us to support more children and cover a broader range of treatments.
1.3 Holistic Support Services: We believe in treating the whole child, not just the disease. Our holistic support includes counseling services to address emotional needs and playful education in our dedicated playroom to ensure that childhood joy is not lost. Additionally, we provide comforting accommodations at Grace, a home away from home, offering a sanctuary of solace and growth for both patients and their families.
1.4 Forging Collaborative Alliances: Collaboration amplifies our impact. We partner with government bodies and compassionate organizations to strengthen our support network and ensure comprehensive care.
Elaborated 360˚ Philanthropic model for Pediatric Cancer
Rajiv Gandhi Cancer Institute and Research Centre lead the way in establishing the first privately dedicated pediatric oncology unit in the country in 1998. Since then, it has been a pioneer benchmark for pediatric cancer care.
1. Financial Model
The most important pillar of the philanthropic services available in the hospital is the financial model which is maintained by the philanthropy department of the hospital by using funds from government and various other collaboration with different organizations.
1.1 Policy Process Involved
Through partnerships with government initiatives, NGOs, and CSR donations, we have established robust frameworks for affordable pediatric cancer treatment. Patients in need are referred by the Department of Pediatric Oncology to the Department of Philanthropic Services. Here, patients and their caregivers receive counseling and information on available schemes tailored to cover their treatment costs.
1.2 Financial Policy Results
During the period from 2021 to 2023, RGCIRC registered 43,731 malignancies, of which 1,098 (2.51%) were pediatric patients aged 0-19 years. Among these young patients, 997 (90.84%) received treatment at our center.
Figure 1 represents Annual Treatment Rates (TPA + Cash + Funds): 2021: 88.04%, 2022: 91.50%, 2023: 93%.
Figure 1. Trend of Treated Malignancies Over the Period (2021-2023).
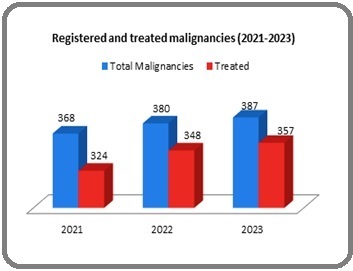
Figure 2 depicts the mode of payment by patients in the year (2021-2023).
Figure 2. Mode of Payment Adopted Patients in the Year (2021-2023).
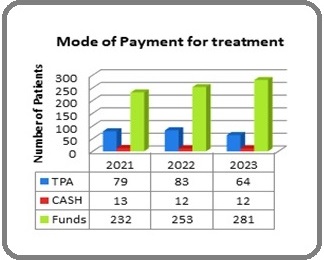
Figure 3 represents the Financial Assistance Exclusively Through Funds: 2021: 71.60%, 2022:72.70%, 2023: 78.70%.
Figure 3. Amount of Funds Raised Through Different Schemes in the Year (2021-2023).
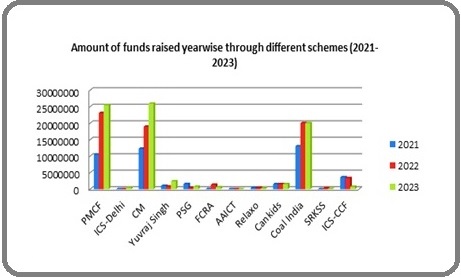
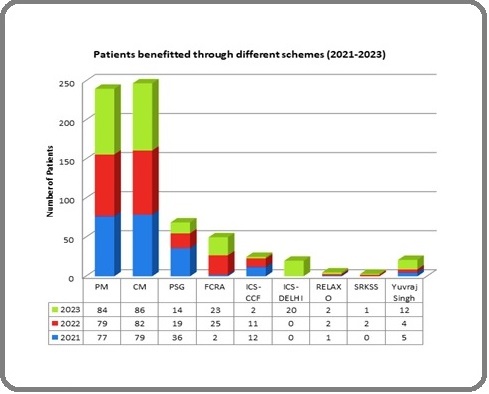
Figure 4 represents number of patients benefitted through different schemes.
Figure 4. Patients Benefitted Through Different Schemes in the Year (2021-2023).
Funds allocated for pediatric treatment increased from Rs 4.38 crores to Rs 7.8 crores.
2 Pre-treatment fertility preservation counselling - Impairment of fertility is one of the key late side effects of chemotherapy or radiation on pediatric patients which can cause fertility problems in both sexes [7]. Hence fertility preservation is considered by the doctors for both males – as sperm banking (post-pubertal), females - Egg Freezing (Oocyte Cryopreservation). Unfortunately, in most cases parents refuse these techniques because of their primary focus of child’s current health and social discomfort to discuss terms like sperm preservation with the child. As impairment of fertility occurs in up to 30% of children treated with chemo- and/or radiotherapy [7] therefore, need of proper age specific education to child and parent’s counselling is very crucial to prevent the collapse of child’s future fertility health.
3. Accommodation Service - As the course of treatment in cancer patients can go up to several months it becomes economically unfeasible for the lower middle class groups to sustain the cost of living in the city of hospital where treatment is going on, hence it becomes one of key supporting roles of the philanthropic care department of hospital to support the accommodation of the patient’s family near the hospital at minimum or no cost. Therefore, a four-floor building is available near the RGCIRC which is called “home GRACE” by the family of pediatric patients where they can stay during the treatment period at a bare minimum cost. The home consists of 16 rooms which are self-sufficient with piped gas and kitchens, there is also a play area for children on the ground floor (Parents and Families - Rajiv Gandhi Cancer Institute & Research Centre, n.d.) [8]. From past 8 years of GRACE service RGCIRC has provide accommodation to more than 300 patients where one stay of the family can vary from 2 months to 6 months on an average.
4. Treatment community joining – During the ongoing treatment, a social media community is created on WhatsApp with names (UMANG) which make the pediatric patient and there family little normal about their disease and suffering, which help them to cope the struggle of cancer treatment like chemotherapy. Platforms like UMANG help by providing a common platform to all the ongoing chemotherapy patients so that they can interact and share their side of stories with the most relevant group of cancer patients.
5. Mental well-being of child and parents – Cancer patients that are aged 7–21 years old, almost 37% came under the DSM-5 criteria for depressive and/or anxiety disorders (Yardeni et al., 2021). Studies have shown that parental mental health is affected continuously after the diagnosis of childhood cancer in their children. The mother’s mental health is severely affected compared to father [9]. Parents are the one who are going to make continues decision regarding their child treatment, social distress not only ends in the treatment they are going to come in hospital for multiple visits for Long term follow up, all these circumstances will create a sense of uncertainty in the mind of parents which may affect their normal cognitive ability of rational decision making that can create serious medical condition in their children. Thus, timely intervention of the parents’ Psychological and emotional needs can help them cope with their child’s treatment, making the treatment process and follow- up smoother. Even timely detection of children with prolonged emotional distress is very crucial to maintain the mental wellbeing of a patient. The admitted patients in pediatric oncology of hospital RGCIRC are ensured to not to incorporate the children with tensed environment of hospital, hence a specific area is designed for pediatric care where the environment is more child friendly, it includes various board games and fun activities to engage the children during the chemotherapy period. Watching their child having an enjoyable time in the hospital creates a sense of safety in parents. A special staff is allocated to make sure the maintenance of this friendly and fun environment of pediatric care, it also includes a teacher which make sure the basic learning of children is not affected by the cancer treatment by engaging the child in simple mindful activities like puzzle or painting.
6. LTFU (Long Term Follow Up) – ACT clinic, once the treatment is completed the patient’s file is transferred to ACT clinic which is after completion therapy clinic which play a major role in checking of the relapse of the disease after treatment by conduction blood test like cbc, kft , the bmi of child on every follow up and a complete body scan like mri, CT scan which is free of cost by the hospital. On an average for 2 years after treatment, ACT clinic focuses on the prevention of relapse of cancer , after 2 years, ACT clinic keep an eye on the mental-cognitive ability of the child by running various mental ability assessment test to make sure that normal growth of brain is not affected by the chemotherapy, ACT clinic will make an ACT card for the child which will include all the possible problems in each organ can occur because of the given chemotherapy medicine wise, This is undertaken to guarantee that the patient comprehends the illness and acknowledges the rationale behind making lifestyle decisions, such as the significance of sustaining a healthy weight and augmenting fruit intake, among other factors. After 2 years of follow up for relapse prevention, ACT suggest at least 8 Years of more follow up which can me monthly, quarterly or half yearly in accordance to parents and patient, which is to make sure the smooth transfer of the child in the normal healthy human society without any side effects of the treatment he received.
Similarly, like UMANG there is an online community which is being maintained by the hospital for the patients who are in follow up with the name “Aashayein,” currently there are more than 400 active members in this community. People during follow up may require additional emotional support from someone who can understand their medical struggle, hence this community fulfills this need.
7. Child education- As the duration of chemotherapy is generally very long, it can take up to 3 months to some years until there is no evidence of the disease is declared by the physician, therefore the crucial time period of child’s education get over without the basic education which adds up to their disadvantage to others for their future employability which ultimately makes them suffer more than a normal human in there career settling phase. A specialized Education and learning’s platform with ‘PRAYAS’ series to sensitize and enable Cancer survivors and volunteers towards palliative care (for a 2-3 days training program on the symptom management and improve people’s experience at the end of life care) is created to integrate the oncology health care system with the large available human resource of cancer survivors who are finding it difficult to get employed elsewhere in the industry.
Challenges yet to overcome
LTFU
“Long term Follow Up” is a way which is used by the health care providers to track the patient’s biological, physical, social, and psychological ability in terms of their social skills, mental health, physical health, and cognitive ability [10]. LTFU measures all the common parameters which can be used to track the normal life of a patient after radical treatment like chemotherapy. In pediatric patients the LTFU becomes much more important as late effects of chemotherapy on children has shown Cardiovascular Issues, Endocrine Disorders, Second Malignancies, and other complications like thyroid or cardiac dysfunction, second malignant neoplasms and neurocognitive difficulties (Childhood Cancer Survivors: What to Expect After Treatment - HealthyChildren.Org, n.d.) [11]. Therefore, the need for a proper “survivorship care plan” which is highly individually maintained becomes especially important. What we have observed in our ACT clinic is the decrease in the follow-ups of the pediatric patients because of them finding hard to inform their Adult son or daughter about their childhood cancer diagnosis as most of the pediatric patients are not aware of their proper diagnosis during the treatment and parents try to avoid the past traumatic discussion of oncological diagnosis and treatment with the child.
Insurance after no evidence of disease
Research indicates that despite achieving no evidence of disease after treatment, childhood cancer survivors often struggle with obtaining health insurance due to their medical history [12]. The stigma associated with past cancer diagnoses can result in higher premiums or denial of coverage, complicating future healthcare access [12]. This insurance injustice makes it difficult for the survivor to achieve complete social-economic integration with society which is a failure of after completion therapy clinic and a failure of healthcare system.
Parents’ Employability during treatment
The economic burden of childhood cancer treatment is significant, as many parents may lose their jobs while caring for their sick child. This loss contributes to increased financial strain on families already facing high medical costs associated with treatment and follow-up care [13].
Discussion
Childhood cancer, while often intensive, is curable. Talking about the cure the traditional cancer treatment which included surgical methods, chemotherapy and radiation had their own limitations like cytotoxicity in long term compared to latest treatment options like immunotherapy and targeted therapy which has better efficiency and less limitations, but the cost that latest treatment involve is too high and causes financial toxicity in the families of cancer patients, especially in Lower-middle-income countries(LMIC). Therefore, too many young warriors are denied access to life-saving treatment due to logistical and financial constraints in LMIC. Since its establishment in 2019, the Department of Philanthropic Services at Rajiv Gandhi Cancer Institute & Research Centre (RGCIRC) has stood as a beacon of hope for newly diagnosed cancer warriors up to the age of 19 years. Our mission is to ensure that “No one is denied treatment because of lack of funds. Our vision is to bridge the gap between children and access to sustainable treatment. Through collaborative efforts with governmental initiatives like PM Relief funds and CM Relief funds, agreements with NGOs and CSR donations from PSU’s and corporates, we strive to dismantle the barriers that stand in way of children receiving the care they deserve. Cancer diagnosis does not affect the family only financially, it disturbs them at social levels, mental levels, and even physical levels. Hence incorporating the financial help from philanthropy RGCIRC was successful in creating these 360 holistic approach models of pediatric cancer care.
Replicability Potential
Our journey has taught us that closing the gap in treatment affordability is crucial. We aim to ensure 100% access for all children by addressing the needs of the remaining 101 (9.16%) untreated patients. Our principle is simple yet powerful: no child will be denied care. To achieve this, we plan to forge connections with more organizations, expand patient welfare programs, and increase funds to leave no child behind. Pediatric cancers represent a small subset where the comprehensive approach has been successfully applied. However, this approach can be replicated in other curable cancers by RGCIRC and other institutes.
In conclusion, the comprehensive 360˚ philanthropic support model at RGCIRC exemplifies a holistic and sustainable approach to tackling childhood cancer. By expanding patient welfare schemes, enhancing fundraising efforts, providing holistic support services, and forging collaborative alliances, we are making significant strides in breaking down financial and logistical barriers to treatment. Our success over the past years demonstrates the model’s effectiveness and its potential for replication to ensure that every child battling cancer receives the care they deserve. This paper highlights the transformative power of an integrated approach, ensuring that childhood cancer does not strip away the innocence and joy of young lives. Through unwavering commitment and collaborative efforts, we stand resolute in our mission to save lives, one child at a time.
Acknowledgements
Funding Source
This study received no funding.
Scientific Approval
Approval was obtained from the Scientific committee of Rajiv Gandhi Cancer Institute and Research Centre, Rohini.
Ethical Declaration
Approval was obtained from the Institutional Review Board of Rajiv Gandhi Cancer Institute and Research Centre, Rohini. Participation was voluntary, with informed consent obtained online before survey initiation. Anonymity and confidentiality of participant data were strictly maintained.
Authors’ contributions
Swarnima Jaitley and Gauri Kapoor: Conceptualization,
study design, manuscript reviewing and editing.
Diksha Mehta and Harsh Lalwani: Data Curation, Manuscript drafting, data analysis, reviewing and editing. Sandeep Jain, Payal Malhotra, Gauri Kapoor:
Manuscript reviewing and editing.
Data Availability : Data will be available on request from author.
References
- Toward the Cure of All Children With Cancer Through Collaborative Efforts: Pediatric Oncology As a Global Challenge Rodriguez-Galindo C, Friedrich P, Alcasabas P, Antillon F, Banavali S, Castillo Luis, Israels T, et al . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2015;33(27). CrossRef
- The Challenge of Quality Care for Family Caregivers in Pediatric Cancer Care Jones BL . Seminars in Oncology Nursing.2012;28(4). CrossRef
- Childhood cancer – IARC. (n.d.). Retrieved December 16, 2024, from https://www.iarc.who.int/cancer-type/childhood-cancer/. .
- Estimated National and State Level Incidence of Childhood and Adolescent Cancer in India. (n.d.). Retrieved December 16, 2024, from https://www.indianpediatrics.net/may2021/may-417-423.htm .
- A theoretical model of financial burden after cancer diagnosis Jones SM , Henrikson NB , Panattoni L, Syrjala KL , Shankaran V. Future Oncology (London, England).2020;16(36). CrossRef
- State of cancer care in India and opportunities for innovation Chintapally N, Nuwayhid M, Arroju V, Muddu VK , Gao P, Reddy BK , Sunkavalli C. Future Oncology (London, England).2023;19(39). CrossRef
- Fertility Preservation for Prepubertal Patients at Risk of Infertility: Present Status and Future Perspectives Pampanini V, Hassan J, Oliver E, Stukenborg J, Damdimopoulou P, Jahnukainen K. Hormone Research in Paediatrics.2020;93(11-12). CrossRef
- Parents and Families - Rajiv Gandhi Cancer Institute & Research Centre. (n.d.). Retrieved December 9, 2024, from https://www.rgcirc.org/clinical-services/pediatric-hematology-and-oncology-services/parents-and-families/ .
- Mental health outcomes in parents of children with a cancer diagnosis in Sweden: A nationwide cohort study Liu Y, Sundquist J, Sundquist K, Zheng D, Ji J. EClinicalMedicine.2023;55. CrossRef
- Guidelines for Long-Term Follow-Up after Childhood Cancer: Practical Implications for the Daily Work Gebauer J, Baust K, Bardi E, Grabow D, Stein A, Pal HJ , Calaminus G, Langer T. Oncology Research and Treatment.2020;43(3). CrossRef
- Childhood Cancer Survivors: What to Expect After Treatment - HealthyChildren.org. (n.d.). Retrieved December 9, 2024, from https://www.healthychildren.org/English/health-issues/conditions/cancer/Pages/Childhood-Cancer-Survivors-What-to-Expect-After-Treatment.aspx .
- Insurance, legal, and financial hardships of childhood and adolescent cancer survivors—a systematic review Ospelt M, Holmer P, Tinner EM , Mader L, Hendriks M, Michel G, Kälin S, Roser K. Journal of Cancer Survivorship.2024. CrossRef
- Long-term follow-up of survivors of childhood cancer (SIGN Clinical Guideline 132) Gan H, Spoudeas HA . Archives of Disease in Childhood. Education and Practice Edition.2014;99(4). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Nursing , 2025
Author Details
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times