Unveiling Cancer Burden: An Epidemiological Study in a Tertiary Cancer Center, Thailand
Download
Abstract
Objective: Cancer is a significant health burden. This research describes the current state of cancer epidemiology and trends in a tertiary cancer center in Thailand.
Materials and Methods: Data from Saraburi Hospital electronic medical records (SBH), Thai cancer based (TCB), Pathological data, and Saraburi Provincial Public Health Office (PPHO) were merged using identification numbers and birthdates, establishing Saraburi hospital-based cancer registry. Cancers were categorized according to ICD10. Population at risk was obtained from the Thai national census department. Prevalence was calculated by dividing cancer cases by population in each district. Cause-specific incidence rates (CIRs) and mortality rates (CMRs) were estimated for cancer types and gender. Age-standardized incidence rates (ASIRs) and mortality rates (ASMRs) were calculated, weighting with 2020 Thai population data.
Results: Between 2018 and 2022, 10,669 cases were identified in Saraburi province. Breast cancer was the most diagnosed cancer (17.6%), followed by colorectal (13.4%), lung cancer (7.8%), cervical cancer (5.9%), and liver cancer (5.5%). ASIR peaked at 509 (492-527) per 100,000 person-years in 2018 and decreased to 232 (220-244) per 100,000 person-years in 2022. Leading cancers for males were colorectal, lung, liver; females had breast, colorectal, cervical and lung cancer. 5-year prevalence was 1.7%. Males died mostly from lung and liver cancer (ASMR 30 and 29 per 100,000 person-years), while females died from breast cancer (ASMR 21 per 100,000 person-years). Life-time cumulative risk of death from cancer was 11%.
Conclusion: This study reveals the cancer burden in Saraburi province, emphasizing the need for preventive strategies and resource allocations. The establishment of a cancer registry warrants future research.
Introduction
Cancer is a significant global health issue, and the incidence is rising. In Thailand, cancer is the second most common cause of mortality following cardiovascular diseases. In Thailand in 2020, the prevalence was 0.6%, 190,636 new cases were diagnosed, and 124,866 people died from cancer [1].
Although nationwide data is useful for identifying the problem of cancer from a broad perspective, understanding local epidemiology helps with planning effective prevention, resource allocation and treatment strategies.
Saraburi province, in central Thailand, comprises approximately 1% of the country’s population, with increasing cancer and related mortality [2].
This study analyzed the current state of cancer epidemiology in Saraburi province by examining incidence and mortality rates of various types of cancer and assessing prevalence across different districts. The incidence and mortality rates were categorized by cancer sites and gender to explore a detailed understanding of the disease.
Materials and Methods
Data and sources
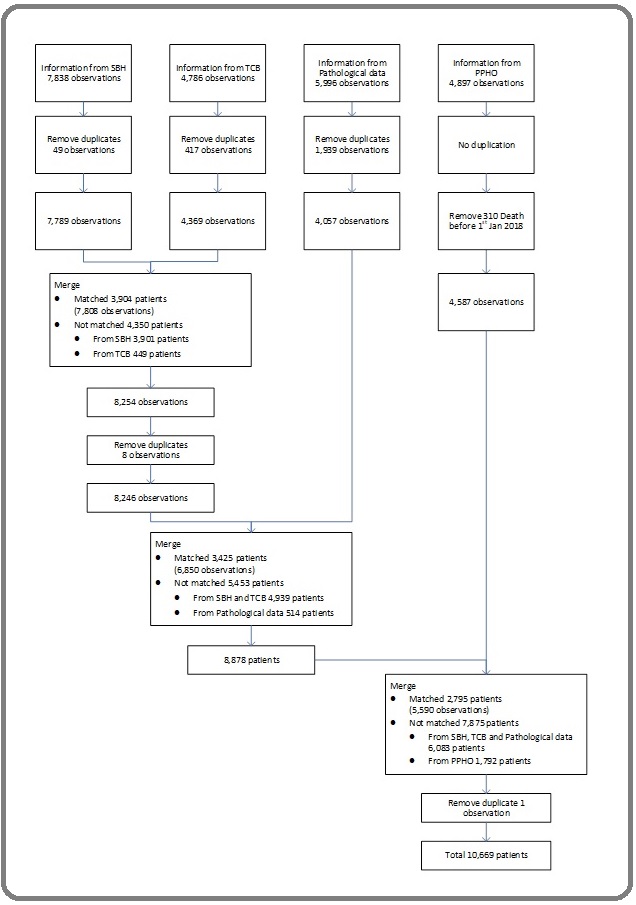
All existing cancer cases between 2018 and 2022 were identified using the 10th edition of the international classification of diseases (ICD10) codes C00-C97 [3]. The cases were obtained from Saraburi Hospital electronic medical records (SBH), Thai cancer based (TCB), Pathological data, and Saraburi Provincial Public Health Office (PPHO). The data from these sources were merged using unique identification numbers and birth dates in STATA version 17 [4]. The process of data merging is illustrated in Figure 1.
Figure 1.The Diagram Illustrates the Sources of Information, Including SBH, TCB, Pathological Data and PPHO Data, along with the steps required to obtain Saraburi Hospital-based Cancer Registry.
The final data established the Saraburi hospital-based cancer registry which was analyzed in this study.
Quality of data
The quality of registry was inspected according to a standard procedure proposed by Bray and Parkin in 2009 [5,6]. The ICD10 codes from SBH, TCB, and PPHO were cross-referenced with topography data from pathological records to ensure the accuracy of the cancer type classification. The proportion of cases categorized as ill-defined sites (ICD10 C80.9) within the registry was only 0.3% and approximately 78% of cases had a morphologically verified (MV) diagnosis. About 14.6% of cases were sourced only from death certificates (DCO). All source databases were randomly cross checked for age, gender, address, and ICD10 before data linkage to ascertain internal data consistency.
Method of estimation
Cancer sites were classified according to ICD10 [3]. Lip and oral cavity defined as C00-C08; nasopharynx as C11; other pharynx as C09-C10 and C12-C14; esophagus as C15; stomach as C16; small intestine as C17; colon and rectum (including anus) as C18-21; malignant neoplasm of liver as C22 except C22.1; ampullar and gall bladder as C23 and 24.1; intra- and extra-hepatic cholangiocarcinoma as C22.1, C24.0, 24.9; pancreas as C25; larynx as C32; lung including trachea as C33-C34; melanoma of skin as C43; Kaposi sarcoma as C46; female breast as C50; cervix uteri as C53; corpus uteri as C54; ovary as C56; prostate as C61; testis as C62; kidney including renal pelvis and ureter as C64-C66; bladder as C67; brain and central nervous system as C70-C72; thyroid as C73; Hodgkin lymphoma as C81; non-Hodgkin lymphoma as C82-C85, C96; multiple myeloma as C88-C90; leukemia as C91-C95; other and unspecified cancer as cancer that ungroupable. The calculation for all cancer sites was performed by summing the counts for individual cancer sites together with “other and unspecified cancer” category.
Period prevalence rates were calculated as the number of existing cancer cases divided by the average population for each district between 2018 and 2022. The cause-specific incidence rate (CIR) was computed by dividing new cancer cases by the at-risk population during the specified period [7]. The incidence rate is presented as cases per 100,000 person-years to avoid the use of decimals and be able to compare results to standard reports [8].
The population and age distribution in Saraburi province was obtained from the national census department [9]. Age-specific incidence rates were determined by dividing new cancer cases in defined age groups (e.g., 0-4, 5-9,…, 70-74, ≥75) by the corresponding at-risk population in each group. The age-standardized incidence rates (ASIRs) were computed using Segi and Doll’s direct method, [10- 12] by weighting age-specific incidence rates with the 2020 age distribution of the Thai population [13]. The cumulative rates for each cancer type were derived by summing age-specific incidence rates across 5-year age intervals. Cumulative risks were determined to estimate the likelihood of cancer development up to age 74. The crude mortality rates (CMRs) by cancer sites were calculated from actual number of cancer specific deaths divided by population at risk of dying during the study period. The age-standardized mortality rates (ASMRs) were calculated weighting age-specific mortality rates with the age distribution of Thai population in 2020. The detailed mathematical formular to calculate CIR, ASIR, CMR, ASMR and cumulative risk are explained elsewhere [7, 10, 14].
Results
Brief number
Between 2018 and 2022, the average population in Saraburi province was 642,879, with 316,442 males and 326,437 females. Among the population, 10,669 individuals across all 13 districts were identified as having cancer. Of these, 4,803 were male and 5,866 were female. There were 9,105 new cancer cases, and the number of deaths during the study period was 5,931. Figure 2 illustrates the proportions of the leading 10 cancers in terms of new cases and deaths in Saraburi province, categorized by male, female, and both genders combined.
Figure 2. The pie charts depict the distribution of new cancer cases and deaths for the 10 Most common cancer type from 2018 to 2022, categorized by A) Both Genders, B) Males, and C) Females.
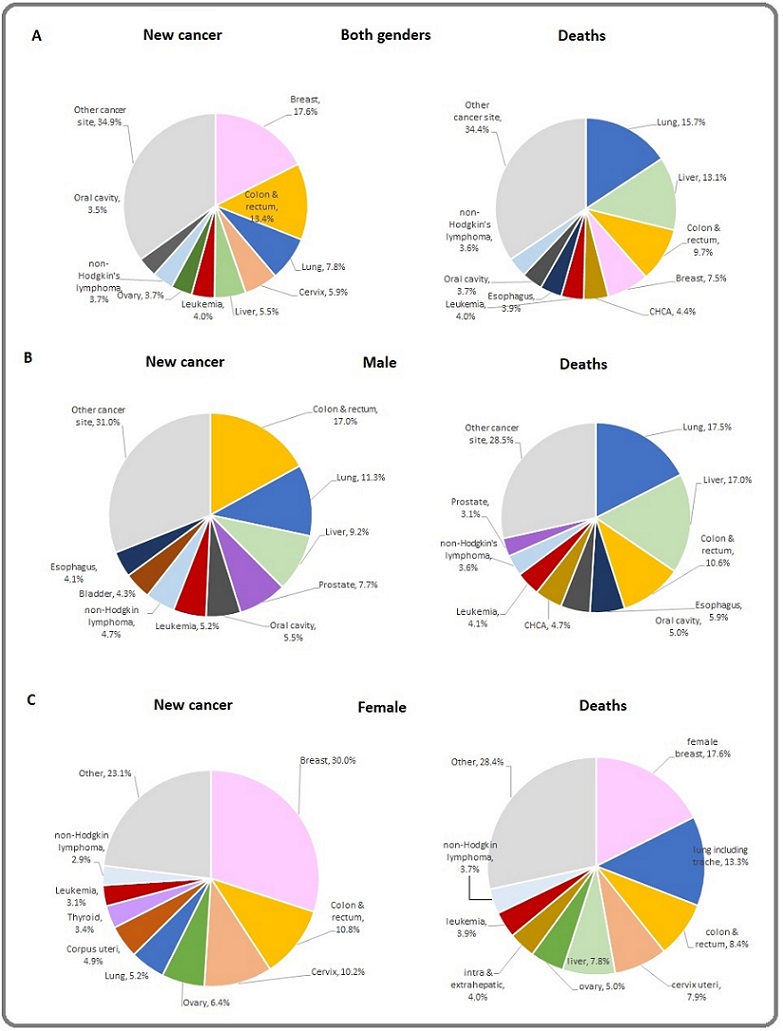
Breast cancer stands as the most frequently diagnosed malignancy, comprising 17.6% of total cases with mortality accounting for 7.5% of cancer-related deaths. Colorectal cancer contributes to 13.4% of total cases, with mortality of 9.7%. Lung cancer was the third most frequent cancer, accounting for 7.8% of new cases, yet it was the primary cause of cancer-related death at 15.7%. New cases diagnosed with cervical cancer and liver cancer were similar at 5.9% and 5.5%. While liver cancer had a smaller proportion of new cases than colon and lung cancer, it ranked as the second highest cause of cancer-related deaths at 13.1% (Figure 2).
Incidence rate
At the initiation of Saraburi Hospital-based cancer registry, the ASIR for all cancer types in 2018 reached a peak at 509.2 (491.7-526.6) per 100,000 person-year.
The ASIR dropped to 238.3 (226.3-250.3) per 100,000 person-year in 2019. The rate remained steady at 222.8 (211.3-234.3) per 100,000 person-year in 2020, 214.3 (203.0-225.7) in 2021, and 232.2 (220.4-243.9) per 100,000 person-year in 2022. The most frequent cancer sites were breast, colon and rectum, cervix, lung, and liver in every year during the study period. In 2022, the top five most common cancers were colorectum with ASIR of 32.9 (28.5-37.4) per 100,000 person-year followed by breast [ASIR 29.3 (25.2-33.5) per 100,000 person-year], lung [ASIR 22.8 (19.1-26.5) per 100,000 person-year], liver [ASIR 15.5 (12.5-18.6) per 100,000 person-year] and cervical cancer [ASIR 13.5 (10.7-16.3) per 100,000 person-year] (Figure 3A).
Figure 3. The bar charts show (A) ASIRs (B) ASMRs per 100,000 person-year by top five of cancer site (breast, colon and rectum, cervix, lung, and liver) in Saraburi Hospital-cancer Registry from 2018 to 2022.
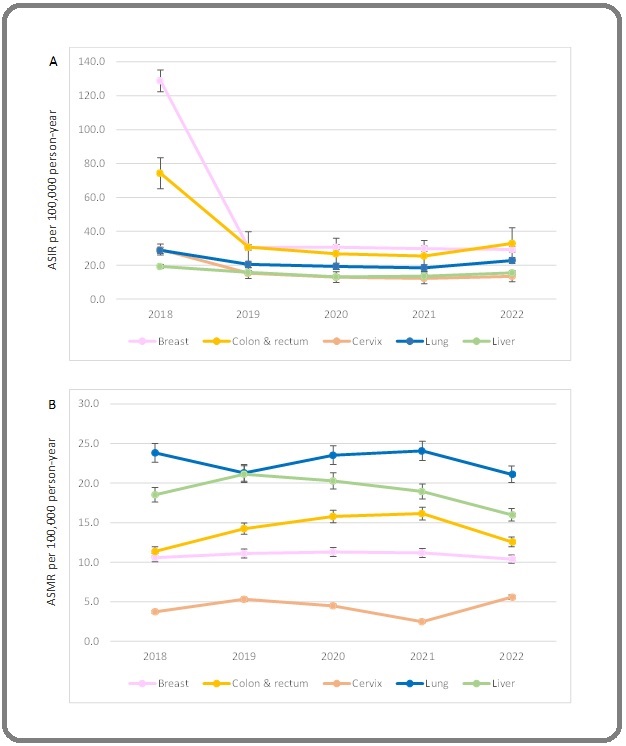
During 2018-2022, the highest ASIRs for both genders were breast, colon, lung, cervical, and liver cancer (ASIRs of 50.5, 39, 22.6, 16.9 and 15.9 per 100,000 person- years, respectively). The top five most common cancers for males were colorectal cancer (ASIR 43.4) followed by lung (ASIR 29.1), liver (ASIR 23.2), prostate (ASIR 20.1) and lip/oral cavity cancer (ASIR 13.6). The top five most frequent cancer sites for females were breast (ASIR 96.9) followed by colorectum (ASIR 35.2), cervix (ASIR 33.1), ovary (ASIR 20.7) and lung (ASIR 16.7).
The summation of cumulative risk to develop any cancer up to age 74 was 21.5%, with 20.5% for males and 22.8% for females. The CIRs, ASIRs per 100,000 person-year and lifetime cumulative risk to develop cancer by site are presented in Table 1.
| Cancer site | Both genders | Male | Female | |||||||||
| New cases (%) | CIRs | ASIRs | Cum. Risk % | New cases (%) | CIRs | ASIRs | Cum. Risk% | New cases (%) | CIRs | ASIRs | Cum. Risk% | |
| Lip, oral cavity | 315 (3.5) | 9.8 | 10 | 0.5 | 210 (5.5) | 13.3 | 13.6 | 0.7 | 105 (2.0) | 6.4 | 7.1 | 0.3 |
| Nasopharynx | 82 (0.9) | 2.6 | 2.6 | 0.2 | 59 (1.5) | 3.7 | 3.8 | 0.3 | 23 (0.4) | 1.4 | 1.4 | 0.1 |
| Other pharynx | 159 (1.7) | 4.9 | 5 | 0.3 | 135 (3.5) | 8.5 | 8.8 | 0.5 | 24 (0.5) | 1.5 | 1.5 | 0.1 |
| Esophagus | 191 (2.1) | 5.9 | 6.1 | 0.4 | 161 (4.2) | 10.2 | 10.5 | 0.6 | 30 (0.6) | 1.8 | 1.9 | 0.1 |
| Stomach | 149 (1.6) | 4.6 | 4.8 | 0.3 | 76 (2) | 4.8 | 5 | 0.3 | 73 (1.4) | 4.5 | 4.5 | 0.3 |
| Small intestine | 14 (0.2) | 0.4 | 0.4 | 0 | 8 (0.2) | 0.5 | 0.5 | 0.1 | 6 (0.1) | 0.4 | 0.4 | 0 |
| Colon & rectum | 1,222 (13.4) | 38 | 39 | 0.9 | 652 (17.0) | 41.2 | 43.4 | 1 | 570 (10.8) | 34.9 | 35.2 | 0.9 |
| Liver cancer | 497 (5.5) | 15.5 | 15.9 | 0.7 | 353 (9.2) | 22.3 | 23.2 | 0.9 | 144 (2.7) | 8.8 | 8.9 | 0.5 |
| Ampular & gall bladder | 41 (0.5) | 1.3 | 1.3 | 0.1 | 14 (0.4) | 0.9 | 0.9 | 0.1 | 27 (0.5) | 1.7 | 1.7 | 0.1 |
| Intra and extrahepatic CHCA | 225 (2.5) | 7 | 7.2 | 0.4 | 131 (3.4) | 8.3 | 8.7 | 0.5 | 94 (1.8) | 5.8 | 5.8 | 0.3 |
| Pancreas | 107 (1.2) | 3.3 | 3.4 | 0.2 | 56 (1.5) | 3.5 | 3.7 | 0.2 | 51 (1) | 3.1 | 3.1 | 0.1 |
| Larynx | 85 (0.9) | 2.6 | 2.7 | 0.2 | 76 (2) | 4.8 | 5 | 0.3 | 9 (0.2) | 0.6 | 0.6 | 0 |
| Lung, trachea | 707 (7.8) | 22 | 22.6 | 0.8 | 436 (11.3) | 27.6 | 29.1 | 0.9 | 271 (5.2) | 16.6 | 16.7 | 0.7 |
| Melanoma of skin | 20 (0.2) | 0.6 | 0.6 | 0 | 6 (0.2) | 0.4 | 0.4 | 0 | 14 (0.3) | 0.9 | 0.9 | 0 |
| Kaposi sarcoma | 2 (0) | 0.1 | 0.1 | 0 | 1 (0) | 0.1 | 0.1 | 0 | 1 (0) | 0.1 | 0.1 | 0 |
| Breast | 1,601 (17.6) | 49.8 | 50.5 | 1 | 26 (0.7) | 1.6 | 1.7 | 0.1 | 1,575 (30) | 96.5 | 96.9 | 1 |
| Cervix | 536 (5.9) | 16.7 | 16.9 | 0.7 | 0 | 0 | 0 | 0 | 536 (10.2) | 32.8 | 33.1 | 0.9 |
| Corpus uteri | 258 (2.8) | 8 | 8.2 | 0.5 | 0 (0) | 0 | 0 | 0 | 258 (4.9) | 15.8 | 15.9 | 0.7 |
| Ovary | 337 (2.8) | 10.5 | 10.6 | 0.5 | 0 (0) | 0 | 0 | 0 | 337 (6.4) | 20.6 | 20.7 | 0.8 |
| Prostate | 298 (3.3) | 9.3 | 9.6 | 0.4 | 296 (7.7) | 18.7 | 20.1 | 0.7 | 2 (0) | 0.1 | 0.1 | 0 |
| Testis | 27 (0.3) | 0.8 | 0.8 | 0.1 | 27 (0.7) | 1.7 | 1.7 | 0.1 | 0 (0) | 0 | 0 | 0 |
| Kidney & ureter | 69 (0.8) | 2.1 | 2.2 | 0.2 | 46 (1.2) | 2.9 | 3 | 0.2 | 23 (0.4) | 1.4 | 1.4 | 0.1 |
| Bladder | 210 (2.3) | 6.5 | 6.8 | 0.4 | 166 (4.3) | 10.5 | 11.2 | 0.5 | 44 (0.8) | 2.7 | 2.7 | 0.2 |
| Brain & CNS | 82 (0.9) | 2.6 | 2.6 | 0.2 | 43 (1.1) | 2.7 | 2.7 | 0.2 | 39 (0.7) | 2.4 | 2.4 | 0.2 |
| Thyroid | 229 (2.5) | 7.1 | 7.2 | 0.4 | 52 (1.4) | 3.3 | 3.4 | 0.2 | 177 (3.4) | 10.8 | 10.9 | 0.5 |
| Hodgkin lymphoma | 28 (0.3) | 0.9 | 0.9 | 0.1 | 13 (0.3) | 0.8 | 0.8 | 0.1 | 15 (0.3) | 0.9 | 0.7 | 0.1 |
| Non-Hodgkin lym- phoma | 334 (3.7) | 10.4 | 10.6 | 0.6 | 180 (4.7) | 11.4 | 11.8 | 0.6 | 154 (2.9) | 9.4 | 9.5 | 0.5 |
| Multiple myeloma | 139 (1.5) | 4.3 | 4.4 | 0.3 | 58 (1.5) | 3.7 | 3.9 | 0.3 | 81 (1.5) | 5 | 5 | 0.3 |
| Leukemia | 368 (4) | 11.4 | 11.6 | 0.6 | 201 (5.2) | 12.7 | 13 | 0.6 | 167 (3.2) | 10.2 | 10.2 | 0.5 |
| Other, unspecified | 773 (8.5) | 24 | 24.5 | 0.8 | 362 (9.4) | 22.9 | 23.7 | 0.8 | 411 (7.8) | 25.2 | 25.3 | 0.8 |
| All cancer sites | 9,105 (100) | 283 | 289 | 21.5 | 3,844 (100) | 243 | 254 | 20.5 | 5,261 (100) | 322 | 322 | 22.8 |
Prevalence rate
Between 2018 and 2022, the 5-year prevalence of all cancer in the Saraburi province population was 1.7%. The prevalence of females living with cancer was slightly higher than that of males by 0.3%. The 5-year prevalence was analyzed across different districts in Saraburi province. Amphur Muang and Sao Hai district had the highest prevalence of cancer cases, with 2.1% of the population affected in those areas. Interestingly, Phra Phutthabat district had the lowest reported cases, with only 0.99% of the population affected. This could suggest that patients in Phra Phutthabat district sought treatment at nearby hospitals in Lopburi province, while patients in Amphur Muang and Sao Hai districts were closer to Saraburi Hospital. The 5-year prevalence of cancer by district and by gender are presented in Table 2.
| District | Cancer cases | Average population during 2018-2022 | Prevalence of cancer (%) | ||||||
| Male | Female | Total | Male | Female | Total | Male | Female | Total | |
| Muang | 1,027 | 1,469 | 2,496 | 60,707 | 57,514 | 118,221 | 1.69 | 2.55 | 2.11 |
| Kangkoi | 714 | 939 | 1,653 | 49,805 | 51,021 | 100,827 | 1.43 | 1.84 | 1.64 |
| Nong Kae | 772 | 1,014 | 1,786 | 45,860 | 48,629 | 94,489 | 1.68 | 2.09 | 1.89 |
| Wihan Daeng | 298 | 366 | 664 | 18,978 | 19,897 | 38,876 | 1.57 | 1.84 | 1.71 |
| Nong Sang | 143 | 169 | 312 | 7,585 | 8,293 | 15,878 | 1.89 | 2.04 | 1.97 |
| Ban Mor | 303 | 259 | 562 | 20,656 | 21,809 | 42,465 | 1.47 | 1.19 | 1.32 |
| Don Phut | 62 | 46 | 108 | 3,292 | 3,426 | 6,718 | 1.88 | 1.34 | 1.61 |
| Nong Don | 110 | 73 | 183 | 6,785 | 7,232 | 14,017 | 1.62 | 1.01 | 1.31 |
| Phra Phutthabat | 331 | 298 | 629 | 30,522 | 33,247 | 63,769 | 1.08 | 0.9 | 0.99 |
| Sao Hai | 291 | 424 | 715 | 16,140 | 17,799 | 33,939 | 1.8 | 2.38 | 2.11 |
| Muaeng Lek | 368 | 396 | 764 | 28,044 | 28,406 | 56,451 | 1.31 | 1.39 | 1.35 |
| Wang Muang | 112 | 92 | 204 | 9,844 | 10,218 | 20,063 | 1.14 | 0.9 | 1.02 |
| Chaloem Phrakiat | 272 | 321 | 593 | 18,223 | 18,946 | 37,169 | 1.49 | 1.69 | 1.6 |
| All district | 4,803 | 5,866 | 10,669 | 316,442 | 326,437 | 642,879 | 1.52 | 1.8 | 1.66 |
Mortality rate
Lung cancer exhibited the highest ASMR at 23.4 per 100,000 person-years followed by liver cancer (ASMR 19.4), colorectal cancer (ASMR 14.4), breast cancer (ASMR 11.1) and intra- or extra-hepatic cholagiocarcinoma (CHCA) (ASMR 6.5) across both genders. In males, lung and liver cancer were the primary causes of cancer-related death with ASMR at 31.4 and at
29.9 per 100,000 person-years, followed by colorectum (ASMR 19), esophagus (ASMR 10.4) and lip/oral cavity (ASMR 8.8). For females, breast cancer stands as the primary cause of cancer-related death, with an ASMR of 21.4 per 100,000 person-year; lung cancer ranked 2nd in mortality with ASMR of 16.1; colorectum, cervix and liver cancer followed as common causes of death, with ASMRs of 10.2, 9.6 and 9.6 per 100,000 person-years, respectively. Cumulative risk of death from any cancer for the population was 11%. Males had higher cumulative risk of cancer death than females by 6.4%. CMRs, ASMRs, and cumulative risk of death were categorized according to cancer types and genders (Table 3).
| Cancer site | Both genders | Male | Female | |||||||||
| Deaths (%) | CMR | ASMR | Cum. Risk% | Deaths (%) | CIR | ASMR | Cum. Risk% | Deaths (%) | CIR | ASMR | Cum. Risk% | |
| Lip, oral cavity | 174 (3.7) | 5.4 | 5.5 | 0.3 | 135 (5.0) | 8.5 | 8.8 | 0.5 | 39 (2.0) | 2.4 | 2.4 | 0.1 |
| Nasopharynx | 33 (0.7) | 1 | 1 | 0.1 | 24 (0.9) | 1.5 | 1.5 | 0.1 | 9 (0.5) | 0.6 | 0.6 | 0.1 |
| Other pharynx | 107 (2.3) | 3.3 | 3.4 | 0.3 | 93 (3.5) | 5.9 | 6.1 | 0.4 | 14 (0.7) | 0.9 | 0.9 | 0 |
| Esophagus | 182 (3.9) | 5.7 | 5.8 | 0.4 | 160 (6.0) | 10.1 | 10.4 | 0.6 | 22 (1.1) | 1.3 | 1.4 | 0.1 |
| Stomach | 120 (2.6) | 3.7 | 3.8 | 0.2 | 61 (2.3) | 3.9 | 4 | 0.3 | 59 (3.0) | 3.6 | 3.6 | 0.2 |
| Small intestine | 13 (0.3) | 0.4 | 0.4 | 0.3 | 11 (0.4) | 0.7 | 0.7 | 0.1 | 2 (0.1) | 0.1 | 0.1 | 0 |
| Colon & rectum | 451 (9.7) | 14 | 14.4 | 0.6 | 285 (10.6) | 18 | 19 | 0.8 | 166 (8.4) | 10.2 | 10.2 | 0.4 |
| Liver cancer | 610 (13.1) | 19 | 19.4 | 0.8 | 456 (17.0) | 28.8 | 29.9 | 0.9 | 154 (7.8) | 9.4 | 9.6 | 0.5 |
| Ampular & gall bladder | 42 (0.9) | 1.3 | 1.3 | 0.1 | 18 (0.7) | 1.1 | 1.2 | 0.1 | 24 (1.2) | 1.5 | 1.5 | 0.1 |
| Intra and extrahepatic CHCA | 203 (4.4) | 6.3 | 6.5 | 0.4 | 125 (4.6) | 7.9 | 8.3 | 0.5 | 78 (4) | 4.8 | 4.8 | 0.3 |
| Pancreas | 108 (2.3) | 3.4 | 3.4 | 0.2 | 58 (2.2) | 3.7 | 3.8 | 0.3 | 50 (2.5) | 3.1 | 3.1 | 0.2 |
| Larynx | 47 (1.0) | 1.5 | 1.5 | 0.1 | 44 (1.6) | 2.8 | 2.9 | 0.2 | 3 (0.2) | 0.2 | 0.6 | 0 |
| Lung, trachea | 732 (15.7) | 22.8 | 23.4 | 0.8 | 471 (17.5) | 29.8 | 31.4 | 0.9 | 261 (13.3) | 16 | 16.1 | 0.7 |
| Melanoma of skin | 4 (0.1) | 0.1 | 0.1 | 0 | 2 (0.1) | 0.1 | 0.1 | 0 | 2 (0.1) | 0.1 | 0.1 | 0 |
| Kaposi sarcoma | 0 (0.0) | 0 | 0 | 0 | 0 (0.0) | 0 | 0 | 0 | 0 (0.0) | 0 | 0 | 0 |
| Breast | 351 (7.5) | 10.9 | 11.1 | 0.6 | 4 (0.1) | 0.3 | 0.3 | 0 | 347 (17.6) | 21.3 | 21.4 | 0.8 |
| Cervix | 156 (3.4) | 4.9 | 4.9 | 0.3 | 0 (0.0) | 0 | 0 | 0 | 156 (7.9) | 9.6 | 9.6 | 0.4 |
| Corpus uteri | 58 (1.2) | 1.8 | 1.8 | 0.1 | 0 (0.0) | 0 | 0 | 0 | 58 (2.9) | 3.6 | 3.6 | 0.2 |
| Ovary | 98 (2.1) | 3 | 3.1 | 0.2 | 0 (0.0) | 0 | 0 | 0 | 98 (5.0) | 6 | 6 | 0.4 |
| Prostate | 83 (1.8) | 2.6 | 2.7 | 0.1 | 83 (3.1) | 5.2 | 5.6 | 0.3 | 0 (0.0) | 0 | 0 | 0 |
| Testis | 2 (0.0) | 0.1 | 0.1 | 0 | 2 (0.1) | 0.1 | 0.1 | 0 | 0 (0.0) | 0 | 0 | 0 |
| Kidney & ureter | 23 (0.5) | 0.7 | 0.7 | 0 | 14 (0.5) | 0.9 | 0.9 | 0.1 | 9 (0.5) | 0.6 | 0.6 | 0 |
| Bladder | 77 (1.7) | 2.4 | 3.7 | 0.3 | 57 (2.1) | 3.6 | 3.8 | 0.2 | 20 (1.0) | 1.2 | 1.2 | 0.1 |
| Brain & CNS | 57 (1.2) | 1.8 | 1.8 | 0.1 | 39 (1.5) | 2.5 | 2.5 | 0.2 | 18 (0.9) | 1.1 | 1.1 | 0.1 |
| Thyroid | 20 (0.4) | 0.6 | 0.6 | 0.3 | 7 (0.3) | 0.4 | 0.5 | 0 | 13 (0.7) | 0.8 | 0.8 | 0 |
| Hodgkin lymphoma | 5 (0.1) | 0.2 | 0.2 | 0 | 2 (0.1) | 0.1 | 0.1 | 0 | 3 (0.2) | 0.2 | 0.2 | 0 |
| Non-Hodgkin lymphoma | 168 (3.6) | 5.2 | 5.4 | 0.3 | 96 (3.6) | 6.1 | 6.4 | 0.4 | 72 (3.7) | 4.4 | 4.5 | 0.3 |
| Multiple myeloma | 55 (1.2) | 1.7 | 1.8 | 0.1 | 32 (1.2) | 2 | 2.2 | 0.2 | 23 (1.2) | 1.4 | 1.4 | 0.1 |
| Leukemia | 186 (4.0) | 5.8 | 5.9 | 0.3 | 109 (4.1) | 6.9 | 7.2 | 0.4 | 77 (3.9) | 4.7 | 4.7 | 0.2 |
| Other, unspecified | 491 (10.5) | 15.3 | 15.7 | 0.7 | 301 (11.2) | 19 | 19.9 | 0.8 | 190 (9.7) | 11.6 | 11.7 | 0.6 |
| All cancer sites | 4,656 (100) | 145 | 148 | 11 | 2,689 (100) | 170 | 178 | 14.5 | 1,967 (100) | 121 | 120 | 8.1 |
Discussion
This study explored the current state of cancer epidemiology in Saraburi province. The estimated ASIR for all cancer sites between 2018 and 2022 was 289 per 100,000 person-year with the ASMR at 148 per 100,000 person-year. The five most prevalent cancers in Saraburi province included breast, colorectal, cervical, lung, and liver cancer, corresponding to the Thailand’s national report [1]. The occurrence of cancer differed by gender. The highest incidences among males were colorectal, lung, liver, prostate, and lip/oral cavity cancer. The highest incidences among females were breast, colorectal, cervical, ovarian, and lung cancer. Lung cancer was the leading cause of cancer-related death for both genders, followed by liver cancer, colorectal cancer, breast cancer, and CHCA. Males died mostly from lung and liver cancer, whereas females died mostly from breast, lung, colorectal, and cervical cancer. Males had higher cumulative risk of cancer-related death than females.
Lung cancer ranked as the primary cause of cancer- related deaths and the third most prevalent cancer in Saraburi province. The disease accounted for nearly one in five (15.7%) cancer-related deaths in the province. This pattern mirrors findings from GLOBOCAN 2020.
[8] In this study, the incidence of lung cancer was about twofold higher in males compared to females (ASIR 29.1 vs 16.7 cases per 100,000 person-year). This pattern was comparable to a previous report on Thai lung cancer incidence (32.0 for male and 10.1 for female per 100,000 person-year) [15]. The disparity in the lung cancer incidence between genders is attributed to variations in tobacco smoking habits, with males smoking more frequently than females (smoking prevalence of 40.8% and 2.2%, respectively) [16]. Although lung cancer incidence in females is lower than in males in Saraburi province, it remains significant. This pattern possibly signified elevated outdoor air pollution and exposure to inhalable agents such as solid fuel combustion for household heating and cooking [8]. Lung cancer mortality in northern Thailand has been linked to elevated concentration of air pollutants, specifically particular matter ≤ 2.5 µm (PM2.5) exceeding 40 µg/m3 [17]. The presence of elevated PM2.5 and PM10 concentrations due to quarrying factories in the province raises concerns about potential impact on lung cancer incidence in the area [17-19]. Health and environmental policies related to emission control must be implemented rigorously.
In Saraburi province, the 1-, 3-, and 5-year mortality rate from lung cancer were 58.8%, 91.3% and 95%, respectively [20]. Despite significant improvements in treatment due to the emergence of EGFR TKIs and immunotherapies in the past decades, three-fourths of lung cancer cases were detected in the advanced stage, causing high risk of mortality [21, 22]. The ASMR of lung cancer in this province is the highest among all types of cancer at 23.4 per 100,000 person-years. This is more pronounced among males, with an ASMR of 31.4 per 100,000 person-years. Since two-thirds of lung cancer-related deaths are caused by smoking tobacco, the disease is preventable through the adoption of effective tobacco control policies and regulations. Multiple randomized control trials have shown that lung cancer screening with low-dose CT scans for high-risk individuals effectively reduced mortality [23-25]. However, the cost-effectiveness of such screening in populations residing in lower to middle-income countries is not known.
In this cohort, 75% of malignant liver neoplasm cases (ICD10 C22) were identified as hepatocellular carcinoma (HCC; ICD10 C22.0). While HCC was the fifth most prevalent cancer in Saraburi province, it was the second highest cause of cancer-related fatalities. HCC incidence was nearly threefold greater in males than in females, with ASIRs of 23.2 and 8.9 cases per 100,000 person-years, respectively. This number is comparable to the national data where the ASIR of HCC is 22.3 per 100,000 person-years [26]. The primary risk factors for HCC in the Thai population are chronic infections with hepatitis B virus (HBV) and hepatitis C virus (HCV) [27]. Chronic HBV infection in the Thai population is estimated at 5-8% [28] but the prevalence in Saraburi province is not known. Primary prevention using recombinant HBV vaccine effectively prevents vertical transmission in infants and long-term development of cirrhosis and HCC [29]. Since 1988, the Thai Ministry of Public Health has advised HBV screening for pregnant women and introduced HBV vaccination to prevent vertical transmission. Additionally, infants born to carriers are given HBV immunoglobulin for post-exposure prophylaxis. However, due to limited supply and high cost, not all infants of HBV-carrying mothers in Saraburi province received the prophylaxis treatment [30]. Although the carrier rate for those under 30 is only 0.1-3.1%, [29] difficulties monitoring individuals who are not immune and carriers born before the vaccination campaign have raised public health concern. A rapid HBV test is now provided for the high- risk population born before 1992 [31].
Intra- and extra-hepatic cholangiocarcinoma (CHCA) is another common form of liver cancer in this region, where it is associated with liver fluke infection, Opisthorchis viverrini (OV). OV is found in raw freshwater fish, which is popularly consumed in the north and northeast regions. In Saraburi province, located on the northeast border of the central region, the incidence of CHCA is 7.2 cases per 100,000 person-years. This incidence falls between the rates in the northeast and central regions (3.8% - 15.7%), [32] possibly due to migration of people from the northeast area to Saraburi province. Previously reported risk factors for cholangiocarcinoma include infection with other types of liver flukes (Clonorhis sinensis, Schistosomiasis japonica), primary sclerosing cholangitis, hepatolithiasis, diabetes, obesity and heavy alcohol consumption [33]. These risk factors have not been explored in this region. Despite having a lower incidence rate than HCC, CHCA is a fatal liver cancer and among the top five contributors to cancer-related mortality in this province.
Colorectal cancer is a prominent global cancer, especially in high-income regions [8]. In lower-income regions like South-Eastern Asia, including Thailand, the rates are lower. Lifestyle changes, such as high consumption of animal products and sedentary behavior, contribute to increased body weight and elevated risk for the disease [8]. In Saraburi province, colorectal cancer incidence is approximately three times higher than the national average (around 15 cases per 100,000 person- years) [34]. The ASIR peaked at 74.3 cases per 100,000 person-years in 2018 when the fecal immunochemical test (FIT) screening program began, but later declined to 25-35 cases per 100,000 person-years. This elevated incidence might reflect the area’s high consumption of red and processed meat due to livestock farming industries, but the potential risk factors have never been explored. Colorectal screening with FITs test effectively reduced mortality in a Taiwanese population-based study.
[35] Under rigorous screening with FIT in Saraburi, the mortality rate from colorectal cancer fell to its lowest point with ASMR at 11.4 per 100,000 person-years. However, in recent years, screening has decreased due to a scarcity of colonoscopes and healthcare personnel to manage positive screening test cases.
Breast cancer increased steadily in Thailand from 17.8 in 1998 to 37.8 per 100,000 in 2020, with an approximate mortality rate of 7.6 per 100,000 in 2016.
[35] The incidence of this disease in Saraburi province aligns with the national data, with the ASIR ranging from 29.8-30.7 per 100,000 from 2019 to 2022. Notably, in 2018, the incidence of breast cancer in this province was exceptionally high, reaching an ASIR of 128.8 per 100,000 person-years.
The high incidence of breast cancer in 2018 may be attributed to various factors, including more accessible screening with mammography and increased awareness from prevention campaigns. Despite limited support for mammographic screening in Thai healthcare settings, [37] the breast screening program in Saraburi province received exclusive endorsement from the Kanchanabaramee Foundation that year. The initiation of the hospital cancer registry might have contributed to potential discrepancies in data collection or retrospective reporting, possibly resulting in data over-reporting for 2018. However, the low mortality rate that year (ASMR of 10.6 per 100,000 person-year) is more likely a result of the breast screening campaign than over-reporting. Furthermore, the COVID19 outbreak in 2019 could have delayed diagnoses of breast cancer because mammography was less accessible. In that case, the breast cancer incidence rate should return to its previous rate after the outbreak has subsided. This trend should be monitored in long term.
Cervical cancer is one of the top-five most prevalent cancers and the primary cause of cancer-related deaths in females. In Saraburi province, the cervical cancer incidence has declined steadily from 29.3 per 100,000 person-year in 2018 to 13.5 per 100,000 person-year in 2022. This trend aligns with the national data, where the estimated incidence rate was 14 per 100,000 person-year [34]. Since 2022, national promotion of preventive methods, such as regular screening with PAP smear for women aged between 35 and 60 years, has contributed to the decreasing trend [37]. Human papillomavirus (HPV) infection is strongly associated with cervical cancer. The quadrivalent HPV vaccination prevented precancerous lesions and was linked to reduced risk of invasive cervical cancer in population-based studies [38,39]. Since 2017, vaccination against human papillomavirus (HPV) infection types 16 and 18 has been administered to girls in fifth grade throughout Thailand [40]. This higher vaccination coverage and screening should reduce cervical cancer incidence and mortality.
This is the first study on cancer epidemiology in Saraburi province. Databases from available sources were merged to minimize incomplete data, giving rise to the initiation of Saraburi hospital-based cancer registry. Around 10% of the cases obtained from the TCB database had not been included in the SBH database. Only 0.3% of the cases were ill-defined (ICD10 80.9). The databases were cross-referenced with data from pathological records to ensure accurate cancer classification. Information for cancer stage and TNM classification was unavailable at the present due to excess incomplete data, necessitating registry enhancement. To acquire accurate survival data, mortality details were obtained from the Provincial Public Health Office registry. The resulting registry is representative of Saraburi province’s cancer cases.
In conclusion, this study reveals the burden of cancer in Saraburi province. Lung cancer and hepatocellular carcinoma pose threats to the population in the area which warrant more focused preventive interventions. Preventions against breast, colon, and cervical cancer could also reduce mortality. The Saraburi hospital-based cancer registry has emerged as a useful resource for future research and care improvement. Our findings help emphasize cancer issues and highlight the importance of preventive healthcare policies.
Conflict of interest
No conflicts of interest need to be disclosed.
Ethical declaration
The study received approval from the Institutional Review Board (IRB) of Human Research Ethics Committee Saraburi Hospital (IRB TH-032) with project code SRBR66-005 and certification number EC005/2566. This review board conforms to global ethical standards outlined in the Declaration of Helsinki, The Belmont Report, CIOMS Guidelines, and the international conference on Harmonization in Good Clinical Practice, ICH-GCP.
Authors contribution
The corresponding author contributed 90% to the work.
Acknowledgements
The authors, on behalf of the Service Plan of Thailand’s Health Region 4, extend gratitude to the Provincial Public Health Office registry, particularly Mr. Watcharapol Naiarun and Mr. Sarawut Phuvasunti, for providing valuable information.
References
- The Global Cancer Observatory. Cancer Incidence in Thailand International Agency for Research on Cancer.2021;394:2020–2021.
- TCB Report Online. Thai population cancer database. National Cancer Institute, https://nci.go.th/ (2022, accessed 9 April 2023) .
- World Health Organization. ICD-10 : international statistical classification of diseases and related health problems : tenth revision, 2nd ed, https://apps.who.int/iris/handle/10665/42980 (2004) .
- StataCorp. Stata Statistical Software: Release 17 .
- Evaluation of data quality in the cancer registry: principles and methods Part II. Completeness Parkin DM , Bray F. European Journal of Cancer (Oxford, England: 1990).2009;45(5). CrossRef
- Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness Bray F, Parkin DM . European Journal of Cancer (Oxford, England: 1990).2009;45(5). CrossRef
- Cancer registration: principles and methods. Statistical methods for registries Boyle P, Parkin DM . IARC scientific publications.1991;(95).
- Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries Sung H, Ferlay J, Siegel RL , Laversanne M, Soerjomataram I, Jemal A, Bray F. CA: a cancer journal for clinicians.2021;71(3). CrossRef
- National Statisical Office. Demography Population and Housing Branch. National Statisical Office, http://statbbi.nso.go.th/staticreport/page/sector/en/01.aspx (2022, accessed 23 June 2023). .
- Cancer incidence in five continents Bray F, Brewster DH , Mbalawa CG , et al . 2014.
- Cancer mortality for selected sites in 24 countries (1950-1957). Sendai SE -: Department of Public Health, Tohoku University School of Medicine Sendai, 1960. Epub ahead of print 1960. DOI: LK - https://worldcat.org/title/36669244. Segi M, Fujisaku S. .
- Cancer Incidence in Five Continents: A Technical Report. 1st ed Doll R , Payne P , Waterhouse J . Springer Berlin, Heidelberg, 1966..
- Ministry of public health. Public Health Statistics A.D.2021. Ministry of public health, https://bps.moph.go.th/new_bps/sites/default/files/statistic 61.pdf (2022). .
- Chapter 7 : Age standardization Bray F, Ferlay J. 1954;:0-3.
- Temporal Trends and Geographic Patterns of Lung Cancer Incidence by Histology in Thailand, 1990 to 2014 Chang JT , Jeon J, Sriplung H, Yeesoonsang S, Bilheem S, Rozek L, Chitapanarux I, et al . Journal of Global Oncology.2018;4. CrossRef
- Smoking prevalence and attributable deaths in Thailand: predicting outcomes of different tobacco control interventions Aungkulanon S, Pitayarangsarit S, Bundhamcharoen K, Akaleephan C, Chongsuvivatwong V, Phoncharoen R, Tangcharoensathien V. BMC public health.2019;19(1). CrossRef
- Impact of Residential Concentration of PM2.5 Analyzed as Time-Varying Covariate on the Survival Rate of Lung Cancer Patients: A 15-Year Hospital-Based Study in Upper Northern Thailand Nakharutai N, Traisathit P, Thongsak N, Supasri T, Srikummoon P, Thumronglaohapun S, Hemwan P, Chitapanarux I. International Journal of Environmental Research and Public Health.2022;19(8). CrossRef
- Temporal Variations and Potential Source Areas of Fine Particulate Matter in Bangkok, Thailand Kanchanasuta S, Sooktawee S, Patpai A, Vatanasomboon P. Air, Soil and Water Research.2020;13. CrossRef
- Long-term Exposure to PM10 Increases Lung Cancer Risks: A Cohort Analysis Lee HW , Kang S, Kim S, Cho Y, Hwang S. Cancer Research and Treatment : Official Journal of Korean Cancer Association.2022;54(4). CrossRef
- Association between duration of diagnosis to treatments and mortality among advanced stage non-small cell lung cancer patients in Saraburi Hospital Chantasartrassamee P, Vichapat V. Journal of Medicine and Health Sciences.2022;29(3).
- Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma Mok TS , Wu Y, Thongprasert S, Yang C, Chu D, Saijo N, Sunpaweravong P, et al . The New England Journal of Medicine.2009;361(10). CrossRef
- Chemotherapy for Lung Cancer in the Era of Personalized Medicine Lee SH . Tuberculosis and Respiratory Diseases.2019;82(3). CrossRef
- Prolonged lung cancer screening reduced 10-year mortality in the MILD trial: new confirmation of lung cancer screening efficacy Pastorino U, Silva M, Sestini S, Sabia F, Boeri M, Cantarutti A, Sverzellati N, et al . Annals of Oncology: Official Journal of the European Society for Medical Oncology.2019;30(7). CrossRef
- Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial Koning HJ , Aalst CM , Jong PA , Scholten ET , Nackaerts K, Heuvelmans MA , Lammers JJ , et al . The New England Journal of Medicine.2020;382(6). CrossRef
- Reduced lung-cancer mortality with low-dose computed tomographic screening Aberle DR , Adams AM , Berg CD , Black WC , Clapp JD , Fagerstrom RM , Gareen IF , et al . The New England Journal of Medicine.2011;365(5). CrossRef
- Epidemiology and treatment of hepatocellular carcinoma in Thailand Chonprasertsuk S, Vilaichone R. Japanese Journal of Clinical Oncology.2017;47(4). CrossRef
- Risk Factors for the Development of Hepatocellular Carcinoma in Thailand Chitapanarux T, Phornphutkul K. Journal of Clinical and Translational Hepatology.2015;3(3). CrossRef
- Prevalence of chronic hepatitis B virus infection in Thailand: a systematic review and meta-analysis Leroi C, Adam P, Khamduang W, Kawilapat S, Ngo-Giang-Huong N, Ongwandee S, Jiamsiri S, Jourdain G. International journal of infectious diseases: IJID: official publication of the International Society for Infectious Diseases.2016;51. CrossRef
- Long term efficacy of hepatitis B vaccine in infants born to hepatitis B e antigen-positive mothers Poovorawan Y, Sanpavat S, Pongpunglert W, Chumdermpadetsuk S, Sentrakul P, Vandepapelière P, Safary A. The Pediatric Infectious Disease Journal.1992;11(10). CrossRef
- Towards the elimination of viral hepatitis in Thailand by the year 2030 Posuwan N, Wanlapakorn N, Sintusek P, Wasitthankasem R, Poovorawan K, Vongpunsawad S, Poovorawan Y. Journal of Virus Eradication.2020;6(3). CrossRef
- Department of disease control. Guidelines for Hepatitis B and C viruses in targeted population. Department of disease control, https://ddc.moph.go.th/uploads/publish/1401120230315090152.pdf (2563) .
- National and subnational population-based incidence of cancer in thailand: Assessing cancers with the highest burdens. Cancers; 9. Epub ahead of print 2017 Virani S, Bilheem S, Chansaard W, et al . . CrossRef
- Liver Fluke-Associated Biliary Tract Cancer Prueksapanich P, Piyachaturawat P, Aumpansub P, Ridtitid W, Chaiteerakij R, Rerknimitr R. Gut and Liver.2018;12(3). CrossRef
- Cancer in Thailand: Vol.IX, 2013-2015. Bangkok (Thailand): New Thammada Press, http://www.nci.go.th/th/cancer_record/cancer_rec1.html (2018) Imsamran W, Pattatang A, Supattagorn P, et al . .
- Effectiveness of fecal immunochemical testing in reducing colorectal cancer mortality from the One Million Taiwanese Screening Program Chiu H, Chen SL , Yen AM , Chiu SY , Fann JC , Lee Y, Pan S, et al . Cancer.2015;121(18). CrossRef
- Cancer incidence in five continents, CI5plus: IARC CancerBase No. 9. Lyon, France: International Agency for Research on Cancer Ferlay J, Colombet M, Bray F. .
- Breast cancer screening among women in Thailand: analyses of population-based household surveys Mukem S, Sriplung H, McNeil E, Tangcharoensathien V. Journal of the Medical Association of Thailand = Chotmaihet Thangphaet.2014;97(11).
- HPV Vaccination and the Risk of Invasive Cervical Cancer Lei J, Ploner A, Elfström KM , Wang J, Roth A, Fang F, Sundström K, Dillner J, Sparén P. The New England Journal of Medicine.2020;383(14). CrossRef
- Human Papillomavirus Vaccination and Trends in Cervical Cancer Incidence and Mortality in the US Tabibi T, Barnes JM , Shah A, Osazuwa-Peters N, Johnson KJ , Brown DS . JAMA pediatrics.2022;176(3). CrossRef
- Human papillomavirus (HPV) vaccine status and knowledge of students at a university in rural Thailand Chanprasertpinyo W, Rerkswattavorn C. Heliyon.2020;6(8). CrossRef
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times