Strategic Management and Reduction of Treatment Delays in Radiotherapy (Smart – Rad) – A Prospective Quality Improvement Study from a Tertiary Cancer Centre in South India
Download
Abstract
Background: Prolonged waiting times for daily radiation treatment negatively impact patient satisfaction, adherence, and workflow efficiency in radiotherapy centers. Our centre is a tertiary care centre with a high workload, treating around 300 patients a day. The average waiting time was recorded as 54 minutes, which led to patient dissatisfaction. To overcome this, this study was conducted to implement targeted quality improvement interventions to reduce waiting times and optimize treatment workflows.
Methods: A baseline analysis identified key inefficiencies through fishbone and 2x2 matrix analyses. Contributing factors included inefficient scheduling, non-compliance with appointment timings, manpower shortages, and a lack of imaging protocols. Interventions included spaced scheduling, priority slots for special cases, patient and staff education, dedicated coordination personnel, and weekly process reviews. Statistical analysis of pre- and post-intervention waiting times was conducted to evaluate outcomes.
Results: The implementation of interventions reduced the average waiting time from 54 minutes to 36 minutes exceeding our expectation of 40 minutes. Improved patient adherence, enhanced workflow efficiency, and better utilization of the treatment unit were observed. A comparative analysis with global literature highlighted the effectiveness of the multi-faceted approach, achieving results comparable to advanced centers using more resource-intensive strategies.
Conclusion: This quality improvement initiative demonstrates that systematic interventions tailored to institutional needs can significantly reduce waiting times in radiotherapy.
Introduction
Radiotherapy is a cornerstone of cancer management, either as a standalone treatment or in conjunction with surgery and chemotherapy. Approximately 60–70% of cancer patients require radiotherapy during their treatment journey. However, prolonged waiting times for daily radiation treatment remain a significant challenge, affecting patient satisfaction, treatment adherence, and overall operational efficiency [1, 2].
At our centre, delays in initiating daily radiation treatment were identified as a critical issue. We retrospectively analysed our treatment records and found that our patients’ average waiting time was 54 minutes. This not only impacts patient satisfaction but also hinders the optimal utilization of treatment machines. Factors contributing to these delays include inefficient scheduling, the absence of a proper appointment system, patient non-compliance with appointment schedules, and a lack of streamlined imaging protocols.
Modern radiotherapy techniques, such as volumetric- modulated arc therapy (VMAT) and intensity-modulated radiotherapy (IMRT), have demonstrated time efficiency, but their benefits can only be realized with proper time management and optimized workflow [3]. To address these challenges at our institute, we implemented a targeted quality improvement project to reduce waiting times, ensuring a seamless and patient-centered treatment experience.
This initiative aimed to decrease the average waiting time for daily radiation treatment from 54 minutes to 40 minutes within a target time period, leveraging a structured approach rooted in systematic analysis and interventions.
Materials and Methods
Study Design and Setting
This quality improvement study was conducted at the Cancer Institute (WIA), Adyar, Chennai, focusing on a single radiation treatment unit. The primary objective was to identify the causes of delays and implement interventions to reduce the average waiting time for patients undergoing daily radiotherapy from 54 minutes to the target of 40 minutes within a specific time period. The study included 50 patients undergoing daily radiotherapy for head and neck cancer. All patients were treated with either Intensity Modulated Radiation Therapy (IMRT) or Volumetric Arc Therapy (VMAT) radiotherapy technique. The median age was 56 (Range 34-75). The study duration was 3 months. The post intervention phase lasted for 2 months followed by data collection and then analysed.
Baseline Data Collection
The study began with a detailed audit of the existing workflow, which included:
• Patient arrival times, appointment adherence, and delays.
• Treatment unit scheduling, utilization, and overlap in appointments.
• Workflow from patient entry to treatment completion, including imaging protocols and pre-treatment preparation times.
Waiting times were categorized into two groups:
1. First Treatment Day – Initial delays associated with onboarding patients.
2. Subsequent Treatment Days – Recurring delays due to inefficiencies in scheduling and adherence.
Root Cause Analysis
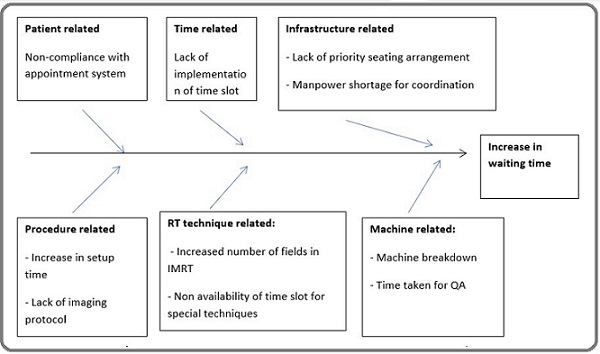
A fishbone diagram and a 2x2 analysis were used to identify the primary contributors to waiting times. Key issues included inefficient scheduling without time slots tailored to patient needs, non-compliance with appointment timings, manpower shortages leading to delays in patient coordination, lack of prioritization for special cases, such as pediatric patients or those requiring complex techniques (Table 1 and Figure 1).
| Lack of implementation of time slot |
| Non compliance with appointment system |
| Manpower shortage for patient Co-oridination |
| Lack of priority seating arrangement. |
| Lack of Imaging protocol. |
Figure 1. Fish Bone Analysis of Factors Contributing to Increase in Radiation Waiting Time.
Based on the root cause analysis, the following interventions were implemented:
1. Spaced Scheduling: Treatment slots were evenly distributed throughout the machine’s operational hours to prevent congestion.
2. Patient and Staff Education: Educational sessions emphasized the importance of adhering to appointment timings and maintaining efficient workflows.
3. Dedicated Manpower: A staff member was assigned to coordinate patient movements, ensuring smoother transitions between appointments.
4. Priority Slots: Special time slots were allocated for new patients, pediatric cases, and advanced treatment techniques to minimize delays.
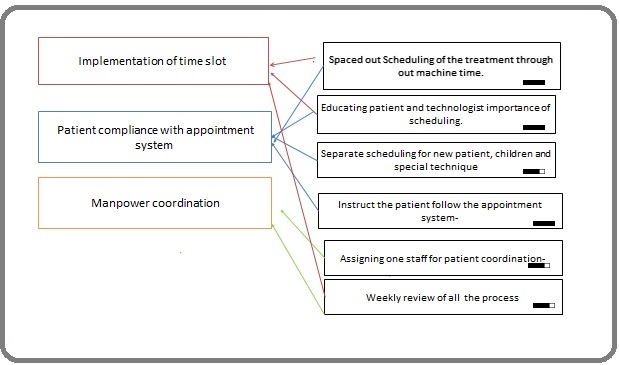
5. Weekly Process Reviews: Regular reviews were conducted to monitor adherence to the new scheduling system and address any emerging issues (Figure 2).
Figure 2. Keydrivers and Interventions.
Data Analysis
Pre- and post-intervention waiting times were analyzed using statistical methods. Key metrics included:
1. Average waiting time (gross and net).
2. Time deviations between scheduled and actual treatment start times.
3. The impact of interventions on overall workflow efficiency.
Pre- and post-intervention waiting times were compared using a paired t-test to assess the statistical significance of the observed reduction. A p-value of <0.05 was considered statistically significant.
Outcome Measures
The primary outcome was the reduction in the average waiting time for daily radiation treatment. Secondary outcomes included improved patient compliance, increased treatment unit utilization, and enhanced workflow efficiency.
Results
Baseline Waiting Time Analysis
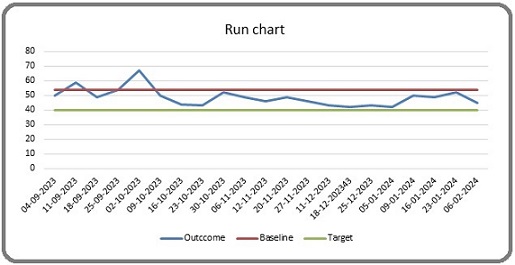
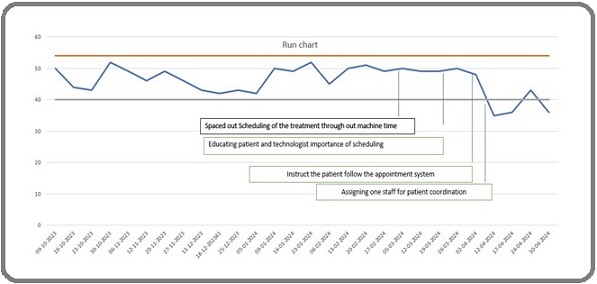
Before implementing interventions, the average waiting time for patients undergoing daily radiation treatment was recorded as 54 minutes. Contributing factors included overlapping patient appointments without tailored time slots, lack of adherence to appointment schedules by patients, manpower shortages leading to delays in patient coordination (Figure 3).
Figure 3. Radiation Waiting Time Before Planned Intervention.
Implementation of Interventions
The interventions, implemented over several months, included spaced scheduling, patient and staff education, priority slots, and weekly process reviews. These changes addressed key inefficiencies identified during the root cause analysis.
Post-Intervention Outcomes
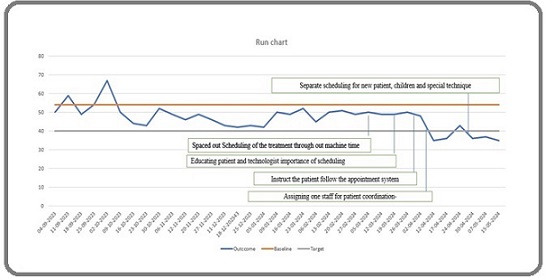
The implementation of these interventions resulted in significant improvements:
1. Reduction in Waiting Time:
- The average waiting time was reduced to 36 minutes.
2. Patient Adherence:
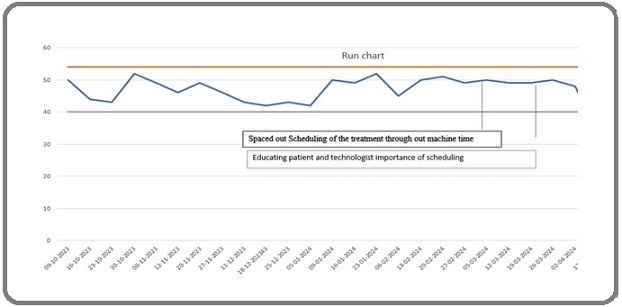
- Improved compliance with appointment schedules due to patient education efforts (Figure 4).
Figure 4. Radiation Waiting Time after Intial Planned Interventions.
1. Workflow Efficiency:
- The introduction of dedicated coordination staff and priority slots reduced delays for new patients, pediatric cases, and advanced treatments.
2. Machine Utilization:
- Optimized scheduling ensured more consistent use of the treatment unit throughout the day (Figure 5).
Figure 5. Radiation Waiting Time after All Planned Interventions.
Comparative Analysis
A comparative analysis of pre- and post-intervention waiting times demonstrated a significant improvement:
• Gross waiting time was reduced by 33%, leading to enhanced patient satisfaction and workflow efficiency.
• Weekly process reviews ensured continuous monitoring and the sustainability of the interventions.
The implementation of interventions led to a significant reduction in waiting times, from an average of 54 minutes to 36 minutes, surpassing the target of 40 minutes. A paired t-test confirmed that this reduction was statistically significant (p < 0.05). The weekly process reviews contributed to maintaining these improvements over time (Figure 6).
Figure 6. Average Reduction in Radiation Waiting Time from 54 Minutes to 36 Minutes.
Institutional Impact
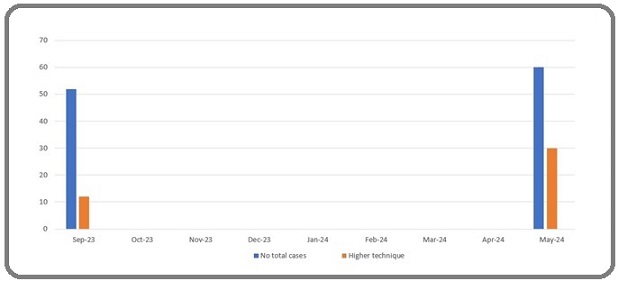
The reduced waiting times led to:
• Improved patient experience and satisfaction.
• Better utilization of existing resources within the treatment unit.
• The development of a framework for replication across other units in the hospital (Figure 7).
Figure 7. Total Number of Cases and Higher Techniques Used .
Discussion
The reduction in waiting times for daily radiation treatment at the Cancer Institute (WIA), Adyar, Chennai, aligns with global efforts to optimize radiotherapy workflows and improve patient satisfaction. Prolonged waiting times have consistently been identified as a significant issue in radiation oncology, impacting patient adherence, treatment outcomes, and overall satisfaction. Studies from advanced centers worldwide have highlighted similar challenges and proposed various solutions, providing valuable context for our findings. The baseline waiting time at our center (54 minutes) was comparable to findings from other centers. Munshi et al. reported mean gross waiting times ranging from 47.4 ± 43.9 minutes for first-day treatments to 37.4 ± 32.7 minutes for subsequent sessions in their audit of an advanced radiotherapy setup [4]. Similarly, Udayashankar et al. noted median waiting times of 25.2 minutes for on-time patients and 38.2 minutes for late-arriving patients in a low-to-moderate volume center [5]. These studies underscore the prevalence of inefficiencies in radiotherapy workflows, even in well-resourced settings.
Our interventions achieved a reduction in average waiting times to 36 minutes, a 33% improvement. This outcome surpasses reductions reported in some studies. Udayashankar et al. demonstrated a significant decrease in waiting times using logical time-slot allocations, but median delays persisted at 21 minutes for late-arriving patients post-intervention [5]. Our success can be attributed to the comprehensive nature of our approach, which combined structural changes with behavioral interventions.
Patient education significantly improved adherence to appointment schedules, consistent with findings by Wallis et al. and Chan et al., who highlighted the importance of punctuality in reducing cumulative delays. [6, 7]. Furthermore, assigning dedicated staff for patient coordination enhanced workflow efficiency, aligning with recommendations for manpower optimization in high- volume centers. Similarly, other studies have addressed this issue [8-10].
Weekly process reviews and staff training programs ensured the sustainability of our interventions. Similar strategies were reported by Munshi et al., who emphasized continuous audits and feedback loops as critical for maintaining improvements. Patient education also helped patients understand the importance of keeping up with time slots/appointments, which further reduced waiting times. This aligns with a study conducted by Williams et al., which emphasizes the importance of patient punctuality in reducing waiting times [11].
Our plan to replicate these interventions across all treatment units provides a scalable model, comparable to approaches adopted by multi-center studies focusing on workflow standardization.
Implications for Practice
Our findings highlight the potential for quality improvement projects to achieve measurable outcomes in resource-constrained settings. While advanced centers in high-income countries have demonstrated success using technology-driven solutions, such as machine-learning- based scheduling systems, our cost-effective approach demonstrates that significant improvements can also be achieved through systematic workflow adjustments.
Limitations and Future Directions
Although the interventions successfully reduced waiting times, further research is needed to explore their long-term impact on treatment outcomes and patient satisfaction. Future studies could incorporate real-time monitoring tools and advanced scheduling algorithms to enhance efficiency further. Additionally, addressing patient-specific factors such as mobility and pre-treatment preparation could refine the workflow further.
In conclusion, this study demonstrates that a structured approach combining evidence-based interventions and continuous monitoring can significantly reduce waiting times for radiotherapy. These findings contribute to the growing body of literature advocating for process improvements in radiation oncology and underscore the importance of adapting solutions to the specific needs and constraints of the institution.
Acknowledgments
Statement of Transparency and Principals
• Author declares no conflict of interest
• Study was approved by Research Ethic Committee of author affiliated Institute.
• Study’s data is available upon a reasonable request.
• All authors have contributed to implementation of this research.
References
- Radiotherapy in India: History, current scenario and proposed solutions Munshi A, Ganesh T, Mohanti BK . Indian Journal of Cancer.2019;56(4). CrossRef
- Optimization of spatiotemporally fractionated radiotherapy treatments with bounds on the achievable benefit Gaddy MR , Yıldız S, Unkelbach J, Papp D. Physics in Medicine and Biology.2018;63(1). CrossRef
- How long does it take? An analysis of volumetric image assessment time Li W, Jaffray DA , Wilson G, Moseley D. Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2016;119(1). CrossRef
- Daily waiting and treatment times at an advanced radiation oncology setup: A 4-year audit of consecutive patients from single institution Munshi A, Krishnakutty S, Sarkar B, Ganesh T, Mohanti BK . Journal of Cancer Research and Therapeutics.2021;17(2). CrossRef
- Optimal time management on linear accelerator: A logical model to reduce patient waiting time Udayashankar AH , Noorjahan S, Srikantia N, Kamunuri RB , Immanuel N, Muzumder S, Chandramouli S. H., Shariff MH . Journal of Cancer Research and Therapeutics.2021;17(1). CrossRef
- Investigating Patient Wait Times for Daily Outpatient Radiotherapy Appointments (A Single-Centre Study) Chan K, Li W, Medlam G, Higgins J, Bolderston A, Yi Q, Wenz J. Journal of Medical Imaging and Radiation Sciences.2010;41(3). CrossRef
- PO‑1023: Reducing waiting room times – A 5‑year review of an in‑house KPI tool Wallis A, Moretti D. Radiother Oncol.2017;123:S564.
- An audit of travel and waiting times for outpatient radiotherapy Junor E. J., Macbeth F. R., Barrett A.. Clinical Oncology (Royal College of Radiologists (Great Britain)).1992;4(3). CrossRef
- Determinants of patient satisfaction during receipt of radiation therapy Famiglietti RM , Neal EC , Edwards TJ , Allen PK , Buchholz TA . International Journal of Radiation Oncology, Biology, Physics.2013;87(1). CrossRef
- Predicting Waiting Times in Radiation Oncology Using Machine Learning Joseph A, Hijal T, Kildea J, Hendren L, Herrera D. 16th IEEE, International Conference on Machine Learning and Applications.2017;:1024-1029.
- Patient punctuality and clinic performance: observations from an academic-based private practice pain centre: a prospective quality improvement study Williams KA , Chambers CG , Dada M, McLeod JC , Ulatowski JA . BMJ open.2014;4(5). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Environment and Cancer , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times