Meta Analysis of the Outcomes in Doing Active Surveillance and Surgical Approach for Micropapillary Thyroid Carcinoma
Download
Abstract
Introduction: Micropapillary thyroid carcinoma was emerging as an epidemic disease worldwide. Due to its unaggressiveness and slow-growing feature, either doing active surveillance or surgical approach were controversial for its management. This meta analysis aimed to determine the pooled proportion outcomes of doing active surveillance and surgery in micropapillary thyroid carcinoma.
Methods: This meta analysis of the results in doing active surveillance and surgical approach for micropapillary thyroid carcinoma, designed followed the PRISMA guidelines. Relevant studies were obtained from Medline (2008-2018) and SCOPUS (2008-2018) in the last 20 years. The scope of data collection is about the author, year of study, and number of subjects. The parameter of this study was pooled proportion. Data were analyzed by MedCalc 13.5 and the significance limit was 0.05.
Results: The pooled proportion of cases of surgery conversion, increasing tumor size more than 3 cm, and the presence of lymph node metastases during active surveillance of micropapillary thyroid carcinoma were 14.996; 6.125%; and 4.988%, respectively. The pooled proportion of cases of recurrence and lymph node metastases after surgery of micropapillary thyroid carcinoma were 3.539% and 14.071%, respectively. Discussion: In this study, it was showed that result was favorable in doing active surveillance. The rate of lymph node metastases were comparable in non and interventional group. However, this approach should be considered cases by cases. Many individual factors like age, gender, and comorbidities should be considered.
Conclusion: Active surveillance was a safe and considered approach for micropapillary thyroid carcinoma. However, some risk factor should be considered for surveillance exclusion.
Introduction
Papillary carcinoma accounted approximately 85% of thyroid tumors, in which surgery is the standard of care [1]. In several cases where, papillary thyroid was dicovered as microcarcinoma, either doing surgical or conservative approach was still controversial until now [2]. Papillary microcarcinomas mostly was less aggressive, in which active surveillance was preferred. Recently, some authors classified there were low- risk and high risk disease. Thus, immediate surgical management was being reconsidered and debated [3]. Active surveillance has emerged to address the concern for over-treatment of low-risk papillary microcarcinoma [4]. The term of active surveillance can be defined as a care plan that observe the patient’s condition regularly without any treatment unless the condition is getting worse [5]. Ito and team were the first team to propose the modality of active surveillance for micropapillary thyroid carcinoma in Japan. Supported by their study from 1993 to 2010, they proved that active surveillance was comparable to that of surgery in 22 year prospective follow up [6]. After that, most studies from Japan highlighted the modalities of active surveillance rather than surgical approach for micropapilary thyroid carcinoma [7]. Kwon et al. in single-center study of South Korea also showed that it was worth of doing active surveillance due to the stability of tumor over 3.8 years [8]. Then, in 2017, Tuttle from United States proved that the growth rates of papillary thyroid microcarcinomas were lower than 1.5 cm, therefore, recommended the conservative modalities [9]. Recently, the ATA introduced guidelines for active surveillance management as an alternative to immediate thyroid surgery for patients with very low-risk tumors [1]. Despite these results, active surveillance has yet to become widely accepted. Progression on its clinical stage remains an absolute switch to surgical intervention [10-28]. Therefore, this meta analysis aim to determine results in doing active surveillance and surgical approach for micropapillary thyroid carcinoma.
Materials and Methods
This study presented a meta-analysis of the results in doing active surveillance and surgical approach for micropapillary thyroid carcinoma. The study design followed the PRISMA guidelines for meta-analysis, based on the Cochrane Handbook for Systematic Review of Interventions guidelines.
A comprehensive literature search were conducted by the authors on December 30th, 2018 to March 1st 2019. Relevant studies were obtained from Medline (2008-2018) and SCOPUS (2008-2018) in the last 20 years. The eligible studies were searched with the keywords based on the meta analysis title. Duplicate journals were managed using EndNote. The title and abstract of the studies were reviewed. The full texts were analyzed for inclusion if they contain original data from the group, clinical trials, and observational studies. Only English language journals and full text are included in this study.
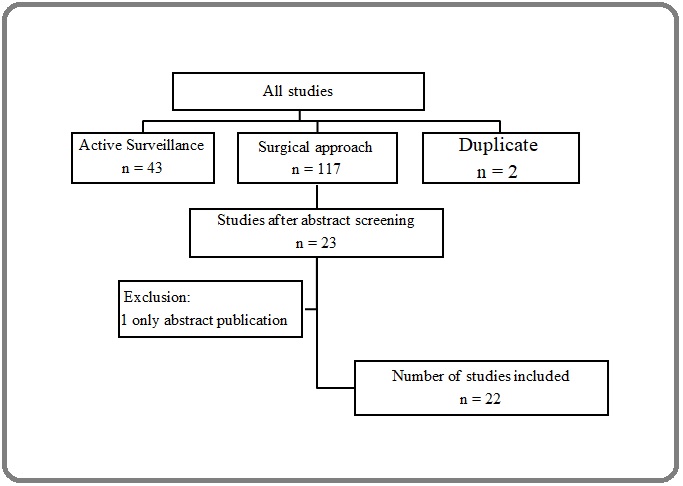
The scope of data collection is about the author, year of study, and number of subjects. The parameter of this study was pooled proportion. Data were analyzed by MedCalc 13.5 and the significance limit was 0.05. For those studies with the data of survival proportion, dichotomous analysis were perfomed. Dichotomous data were presented as odds ratios (ORs) with 95% confidence intervals (CI) (Figure 1).
Figure 1. Flow Chart PRISMA of this Meta Analysis.
Results
There were respectively 11 studies that included in this meta analysis to determine the recurrence and lymph node metastasis rate in micropapillary thyroid managed by surgery (Table 1).
| Study | Year | Country | N | Modalities | Duration (year) | Recurrence (n) | Lymph node metastasis (n) | Overall survival (%) |
| Besic [12] | 2007 | Slovenia | 228 | Surgery | 31 | 7 | ||
| Hay [13] | 2008 | USA | 892 | Surgery | 40 | 72 | ||
| Zuniga [14] | 2009 | Colombia | 266 | Surgery | 45 | 122 | ||
| Ross [15] | 2009 | USA | 2572 | Surgery | 30 | |||
| Ito [16] | 2010 | Japan | 1055 | Surgery | 15 | 32 | 146 | |
| Yu [17] | 2011 | USA | 18445 | Surgery | 19 | 91 | 2294 | 90.7 |
| Gershinsky [18] | 2012 | Israel | 293 | Surgery | 7.2 | 34 | 54 | |
| Karatzas [19] | 2013 | Greece | 311 | Surgery | 12 | 30 | ||
| Nixon [20] | 2013 | USA | 1129 | Surgery | 5.8 | 1 | ||
| Hwangbo [21] | 2016 | Korea | 3282 | Surgery | 2 | 55 | 121 | |
| Li [22] | 2019 | China | 161 | Surgery | 3 | 10 |
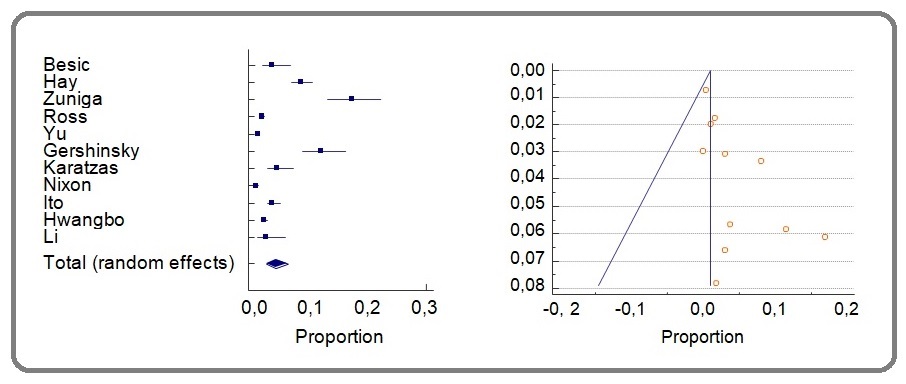
The pooled proportion of recurrence after surgery of micropapillary thyroid carcinoma was 3.539% (95% CI 1.898-5.665; I2 97.8 %; Figure 2).
Figure 2. The Forest Plot and Graph of Pooled Proportion of the Recurrence rate in Micropapillary Thyroid Carcinoma Managed by Surgery.
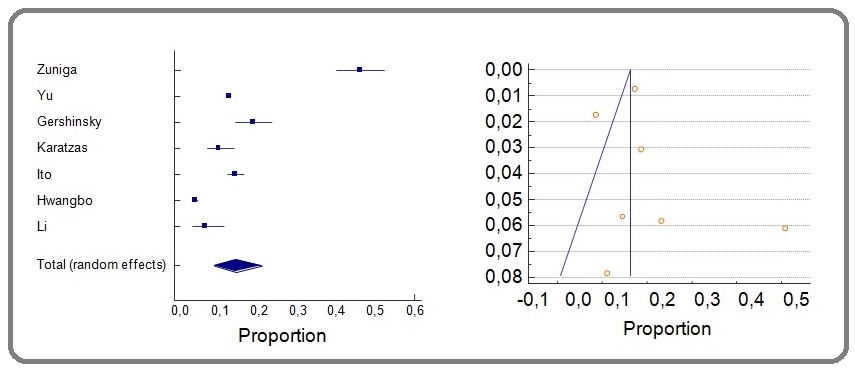
The pooled proportion of lymph node metastasis cases after surgery in micropapillary thyroid carcinoma was 14.071% (95% CI 8.449-20.843; I2 98.83%; Figure 3).
Figure 3. The Forest Plot and Graph of Pooled Proportion of the Lymph Node Metastasis Cases in Micropapillary Thyroid Carcinoma Managed by Surgery.
There were 12 studies that included in this meta analysis to determine the rate of delayed surgeries, cases of increasing tumor size more than 3 cm, lymph node metastasis, and symptomatic cases in micropapillary thyroid managed by active surveillance (Table 2).
| Study | Year | Country | N | Observation | Duration (years) | Convert to surgery (n) | Increase tumor size > 3 mm (n) | Lymph node metastases (n) | Symptomatic (n) |
| Ito [16] | 2010 | Japan | 340 | Periodic USG | 75 mo | 109 | 31 | 7 | 8 |
| Sugitani [23] | 2010 | Japan | 244 | Periodic | 5 | 22 | 3 | ||
| physical | |||||||||
| examination | |||||||||
| and USG | |||||||||
| Smulever [24] | 2015 | Argentina | 34 | Periodic USG | 4 | 5 | 6 | ||
| Fukuoka [25] | 2016 | Japan | 480 | Periodic USG | 6.8 | 29 | |||
| Oda [26] | 2016 | Japan | 1179 | Periodic USG | 0.9 | 94 | 27 | 6 | |
| Leboulleux [27] | 2016 | France | 1235 | Periodic USG | 5 | 129 | 136 | 136 | |
| Kwon [8] | 2017 | Korea | 192 | Periodic | 2.5 | 24 | 23 | 8 | |
| physical | |||||||||
| examination | |||||||||
| and USG | |||||||||
| Tuttle [9] | 2017 | USA | 291 | Periodic USG | 2.1 | 11 | |||
| Sanabria [29] | 2018 | Colombia | 57 | Periodic USG | 1.4 | 5 | 2 | ||
| Kim [30] | 2018 | Korea | 126 | Periodic USG | 2.2 | 18 | 7 | 1 | |
| Oh [31] | 2018 | Korea | 370 | Periodic | 2.7 | 58 | 139 | 108 | |
| physical | |||||||||
| examination | |||||||||
| and USG | |||||||||
| Sakai [32] | 2019 | Japan | 61 | Periodic USG | 2 | 36 |
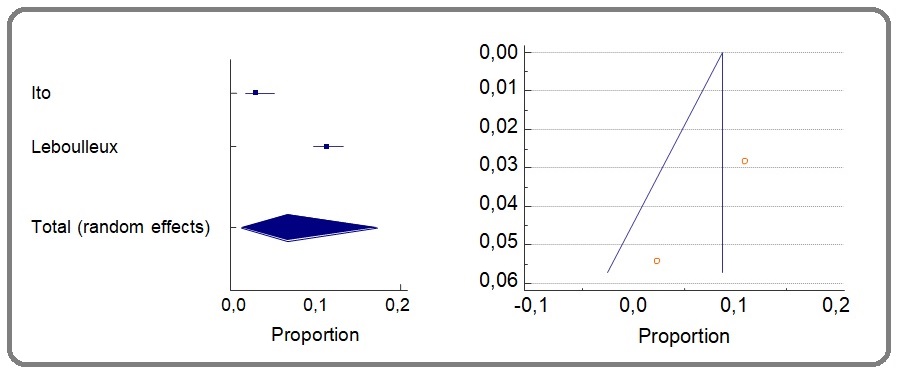
The pooled proportion of the symptomatic cases micropapillary thyroid carcinoma managed by active surveillance was 6.125% (95% CI 0.538-17.312; I2 97.12%; Figure 4).
Figure 4. The Forest Plot and Graph of Pooled Proportion of the Symptomatic Cases in Micropapillary Thyroid Carcinoma Managed by Active Surveillance.
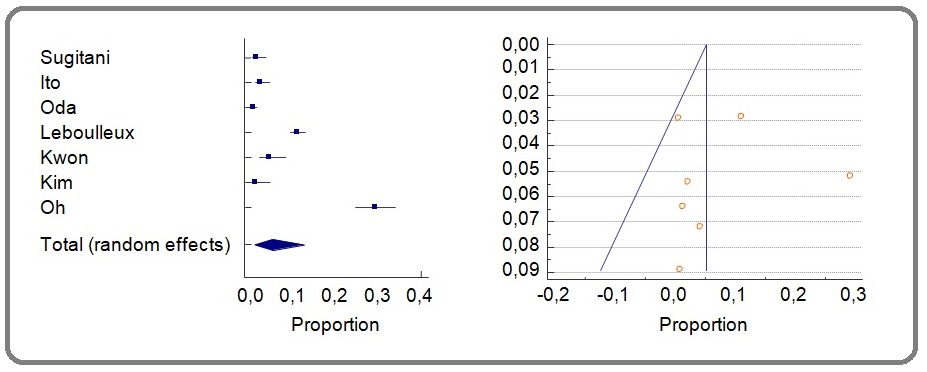
The pooled proportion of the lymph node metastases cases in micropapillary thyroid carcinoma managed by active surveillance was 4.988% (95% CI 0.792-12.499; I2 98.4%; Figure 5).
Figure 5. The Forest Plot and Graph of Pooled Proportion of the Lymph Node Metastasis Cases in Micropapillary Thyroid Carcinoma Managed by Active Surveillance.
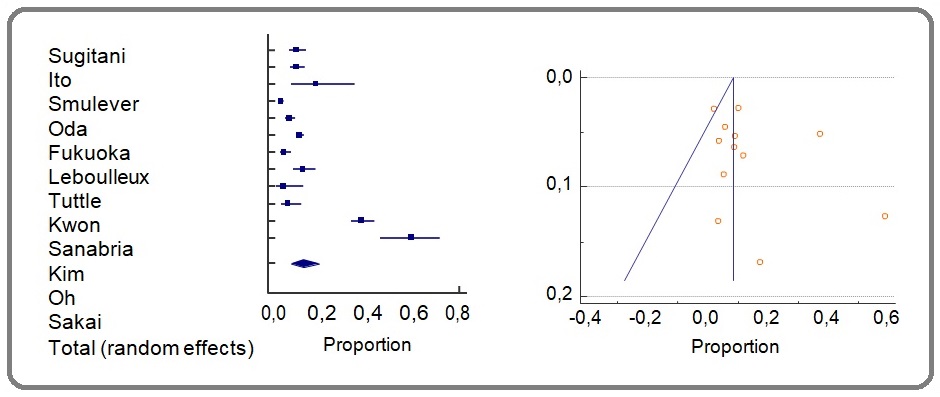
The pooled proportion of cases of increase tumor size > 3 mm during active surveillance of micropapillary thyroid carcinoma was 12.212% (95% CI 6.769-18.891; I2 97.29%; Figure 6).
Figure 6. The Forest Plot and Graph of Pooled Proportion of the Cases of Increasing Tumor Size more than 3 cm in Micropapillary Thyroid Carcinoma Managed by Active Surveillance.
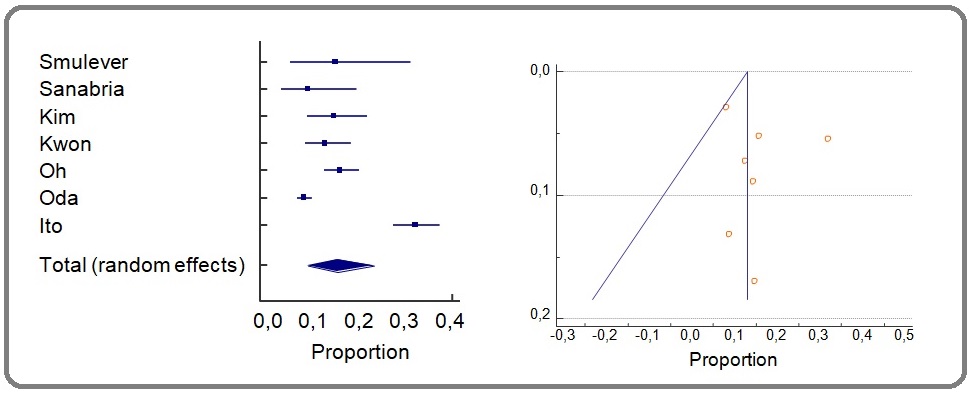
The pooled proportion of number of delayed surgeries during active surveillance of micropapillary thyroid carcinoma was 14.996% (95% CI 11.589-14.371; I2 94.53%; Figure 7).
Figure 7. The Forest Plot and Graph of Pooled Proportion of the Number of Delayed Surgeries in Micropapillary Thyroid Carcinoma Managed by Active Surveillance.
Discussion
Micropapillary thyroid carcinoma has a less aggressive behavior and mostly presence without any symptoms [3]. Recent studies have shown more than 400% increase in micropapillary thyroid carcinoma prevalence along with the improvement of imaging technologies [33]. High-risk micropapillary thyroid carcinoma was defined as a microcarcinoma having one or more lymph node or distant metastasis, high- grade cytology, extra-thyroid extension or significant growth during a previous observation. Low-risk micropapillary thyroid carcinoma was defined a microcarcinoma having none of the afore-mentioned features [34].
Not all clinicians accepted the act of active surveillance for micropapillary thyroid carcinoma, with many aspect of considerations. Small papillary cancer can indeed metastasize or spread to other parts of the body. On the other hand, there is a common belief that thyroid cancer is relatively benign, because of the slow growth. Some studies showed that many considerations should be taken in applying active surveillance for micropapillary thyroid cancer [35]. Age, race, gender can significantly affect survival. Among these 3 factors, age of the subject was the most factor to be considered [36]. A recent report from the SEER program showed that the death rate from thyroid cancer was 2.7 of 100,000 in patients older than 65 years, while it is only 0.1 of 100,000 in patients younger than 65 years, a greater than 25-fold difference [37]. This phenomenon is reflected in several staging systems,including AJCC/pTNM and AMES staging systems. In this meta analysis, it was showed that the rate of cases that converted to surgeries while doing active surveillance was 14.996%, which was still an acceptable rate. The duration of follow up in active surveillance was ranging from 1 to 24 years [35]. The pooled proportion of cases with increasing tumor size more than 3 cm was 12.2%, which showed that no doubt the number of delayed surgeries was about similar. In this study, the pooled proportion cases of lymph node metastases were higher in intervention than active surveillance group, while this could be due to the cases chosen for intervention majority with N1 before. However, this number still indicated that active surveillance was promising to be done for micropapillary thyroid carcinoma.
This study supported the active surveillance approach for micropapillary thyroid cancer with low pooled proportion of numbers of delayed surgeries and lymph node metastases. This approach in the other hand should be preferred also due to its cost-effectivity. However, this approach should be considered cases by cases. Few studies were on going to carry out the exclusion criteria for active surveillance candidate. The upcoming study based in Canada (NCT03271892) was on going in patients with previously untreated papillary thyroid carcinoma with a tumor size less thant 2 cm, no lymph node involvement, and metastasis. The estimated completion date of the study is May 2026. Another study in Los Angeles (NCT02609685) also on going, was recruiting patients with papillary thyroid carcinoma, with tumor size less than 1.5 cm and estimated to be completed in December 2030. In conclusion, active surveillance was a safe and considered approach for micropapillary thyroid carcinoma.
However, the presence of some risk factors should be considered for surveillance exclusion.
References
- Papillary Thyroid Carcinoma. [Updated 2020 Oct 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan Limaiem F, Rehman A, Mazzoni T. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536943/..
- Low-risk papillary thyroid microcarcinoma: Optimal management toward a more conservative approach Ramundo Valeria, Sponziello Marialuisa, Falcone Rosa, Verrienti Antonella, Filetti Sebastiano, Durante Cosimo, Grani Giorgio. Journal of Surgical Oncology.2020;121(6). CrossRef
- Immediate Surgery Might Be a Better Option for Subcapsular Thyroid Microcarcinomas Jiang Jun, Lu Hui. International Journal of Endocrinology.2019;2019. CrossRef
- Active surveillance in low risk papillary thyroid carcinoma Pitoia Fabian, Smulever Anabella. World Journal of Clinical Oncology.2020;11(6). CrossRef
- Clinical application of active surveillance in papillary thyroid microcarcinoma. of active surveillance in papillary thyroid microcarcinoma Chung KW. Annals of thyroid.2017;2(3):7-10. CrossRef
- An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid Ito Yasuhiro, Uruno Takashi, Nakano Keiichi, Takamura Yuuki, Miya Akihiro, Kobayashi Kaoru, Yokozawa Tamotsu, Matsuzuka Fumio, Kuma Seiji, Kuma Kanji, Miyauchi Akira. Thyroid: Official Journal of the American Thyroid Association.2003;13(4). CrossRef
- Insights into the Management of Papillary Microcarcinoma of the Thyroid Miyauchi Akira, Ito Yasuhiro, Oda Hitomi. Thyroid: Official Journal of the American Thyroid Association.2018;28(1). CrossRef
- Active Surveillance for Patients With Papillary Thyroid Microcarcinoma: A Single Center's Experience in Korea Kwon Hyemi, Oh Hye-Seon, Kim Mijin, Park Suyeon, Jeon Min Ji, Kim Won Gu, Kim Won Bae, Shong Young Kee, Song Dong Eun, Baek Jung Hwan, Chung Ki-Wook, Kim Tae Yong. The Journal of Clinical Endocrinology and Metabolism.2017;102(6). CrossRef
- Natural History and Tumor Volume Kinetics of Papillary Thyroid Cancers During Active Surveillance Tuttle R. Michael, Fagin James A., Minkowitz Gerald, Wong Richard J., Roman Benjamin, Patel Snehal, Untch Brian, Ganly Ian, Shaha Ashok R., Shah Jatin P., Pace Mark, Li Duan, Bach Ariadne, Lin Oscar, Whiting Adrian, Ghossein Ronald, Landa Inigo, Sabra Mona, Boucai Laura, Fish Stephanie, Morris Luc G. T.. JAMA otolaryngology-- head & neck surgery.2017;143(10). CrossRef
- 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer Haugen Bryan R., Alexander Erik K., Bible Keith C., Doherty Gerard M., Mandel Susan J., Nikiforov Yuri E., Pacini Furio, Randolph Gregory W., Sawka Anna M., Schlumberger Martin, Schuff Kathryn G., Sherman Steven I., Sosa Julie Ann, Steward David L., Tuttle R. Michael, Wartofsky Leonard. Thyroid: Official Journal of the American Thyroid Association.2016;26(1). CrossRef
- Puzzle over active surveillance for micropapillary thyroid carcinoma Sun Hui, Carcoforo Paolo, Dionigi Gianlorenzo. Annals of Translational Medicine.2018;6(7). CrossRef
- Extent of thyroidectomy and lymphadenectomy in 254 patients with papillary thyroid microcarcinoma: a single-institution experience Besic Nikola, Zgajnar Janez, Hocevar Marko, Petric Rok. Annals of Surgical Oncology.2009;16(4). CrossRef
- Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period Hay Ian D., Hutchinson Maeve E., Gonzalez-Losada Tomas, McIver Bryan, Reinalda Megan E., Grant Clive S., Thompson Geoffrey B., Sebo Thomas J., Goellner John R.. Surgery.2008;144(6). CrossRef
- Prophylactic central neck dissection in stage N0 papillary thyroid carcinoma Zuniga Sergio, Sanabria Alvaro. Archives of Otolaryngology--Head & Neck Surgery.2009;135(11). CrossRef
- Recurrence after treatment of micropapillary thyroid cancer Ross Douglas S., Litofsky Danielle, Ain Kenneth B., Bigos Thomas, Brierley James D., Cooper David S., Haugen Bryan R., Jonklaas Jacqueline, Ladenson Paul W., Magner James, Robbins Jacob, Skarulis Monica C., Steward David L., Maxon Harry R., Sherman Steven I.. Thyroid: Official Journal of the American Thyroid Association.2009;19(10). CrossRef
- An observational trial for papillary thyroid microcarcinoma in Japanese patients Ito Yasuhiro, Miyauchi Akira, Inoue Hiroyuki, Fukushima Mitsuhiro, Kihara Minoru, Higashiyama Takuya, Tomoda Chisato, Takamura Yuuki, Kobayashi Kaoru, Miya Akihiro. World Journal of Surgery.2010;34(1). CrossRef
- Should all papillary thyroid microcarcinomas be aggressively treated? An analysis of 18,445 cases Yu Xiao-Min, Wan Yin, Sippel Rebecca S., Chen Herbert. Annals of Surgery.2011;254(4). CrossRef
- Total versus hemithyroidectomy for microscopic papillary thyroid cancer Gershinsky M., Barnett-Griness O., Stein N., Hirsch D., Tzvetov G., Bardicef O., Pauker J., Grozinsky-Glasberg S., Ish-Shalom S., Slutski I., Shimon I., Benbassat C.. Journal of Endocrinological Investigation.2012;35(5). CrossRef
- Risk factors contributing to the difference in prognosis for papillary versus micropapillary thyroid carcinoma Karatzas Theodore, Vasileiadis Ioannis, Kapetanakis Stylianos, Karakostas Efthimios, Chrousos George, Kouraklis Gregory. American Journal of Surgery.2013;206(4). CrossRef
- Observation of clinically negative central compartment lymph nodes in papillary thyroid carcinoma Nixon Iain J., Ganly Ian, Patel Snehal G., Morris Luc G., Palmer Frank L., Thomas Dorothy, Tuttle R. Michael, Shah Jatin P., Shaha Ashok R.. Surgery.2013;154(6). CrossRef
- Long-Term Recurrence of Small Papillary Thyroid Cancer and Its Risk Factors in a Korean Multicenter Study Hwangbo Yul, Kim Jung Min, Park Young Joo, Lee Eun Kyung, Lee You Jin, Park Do Joon, Choi Young Sik, Lee Kang Dae, Sohn Seo Young, Kim Sun Wook, Chung Jae Hoon, Lim Dong Jun, Kim Min Hee, Kim Min Joo, Jo Young Suk, Shong Min Ho, Koong Sung-Soo, Hahm Jong Ryeal, Jung Jung Hwa, Yi Ka Hee. The Journal of Clinical Endocrinology and Metabolism.2017;102(2). CrossRef
- A comparative study of short-term efficacy and safety for thyroid micropapillary carcinoma patients after microwave ablation or surgery Li Jianming, Liu Yujiang, Liu Jibin, Yang Peipei, Hu Xiangdong, Qian Linxue. International Journal of Hyperthermia: The Official Journal of European Society for Hyperthermic Oncology, North American Hyperthermia Group.2019;36(1). CrossRef
- Three distinctly different kinds of papillary thyroid microcarcinoma should be recognized: our treatment strategies and outcomes Sugitani Iwao, Toda Kazuhisa, Yamada Keiko, Yamamoto Noriko, Ikenaga Motoko, Fujimoto Yoshihide. World Journal of Surgery.2010;34(6). CrossRef
- Active surveillance in papillary thyroid carcinoma: not easily accepted but possible in Latin America Smulever Anabella, Pitoia Fabián. Archives of Endocrinology and Metabolism.2019;63(5). CrossRef
- Natural History of Asymptomatic Papillary Thyroid Microcarcinoma: Time-Dependent Changes in Calcification and Vascularity During Active Surveillance Fukuoka Osamu, Sugitani Iwao, Ebina Aya, Toda Kazuhisa, Kawabata Kazuyoshi, Yamada Keiko. World Journal of Surgery.2016;40(3). CrossRef
- Incidences of Unfavorable Events in the Management of Low-Risk Papillary Microcarcinoma of the Thyroid by Active Surveillance Versus Immediate Surgery Oda Hitomi, Miyauchi Akira, Ito Yasuhiro, Yoshioka Kana, Nakayama Ayako, Sasai Hisanori, Masuoka Hiroo, Yabuta Tomonori, Fukushima Mitsuhiro, Higashiyama Takuya, Kihara Minoru, Kobayashi Kaoru, Miya Akihiro. Thyroid: Official Journal of the American Thyroid Association.2016;26(1). CrossRef
- Papillary thyroid microcarcinoma: time to shift from surgery to active surveillance? Leboulleux Sophie, Tuttle R. Michael, Pacini Furio, Schlumberger Martin. The Lancet. Diabetes & Endocrinology.2016;4(11). CrossRef
- Should small papillary thyroid cancer be observed? A population-based study Nilubol Naris, Kebebew Electron. Cancer.2015;121(7). CrossRef
- Prognosis of patients with thyroid cancer who do not undergo surgical treatment: a SEER database analysis Sanabria Alvaro, Domínguez Luis C., Vega Valentín, Osorio Camilo. Clinical & Translational Oncology: Official Publication of the Federation of Spanish Oncology Societies and of the National Cancer Institute of Mexico.2011;13(9). CrossRef
- High Serum TSH Level Is Associated With Progression of Papillary Thyroid Microcarcinoma During Active Surveillance Kim Hye In, Jang Hye Won, Ahn Hyeon Seon, Ahn Soohyun, Park So Young, Oh Young Lyun, Hahn Soo Yeon, Shin Jung Hee, Kim Jung-Han, Kim Jee Soo, Chung Jae Hoon, Kim Tae Hyuk, Kim Sun Wook. The Journal of Clinical Endocrinology and Metabolism.2018;103(2). CrossRef
- Active Surveillance of Low-Risk Papillary Thyroid Microcarcinoma: A Multi-Center Cohort Study in Korea Oh Hye-Seon, Ha Jeonghoon, Kim Hye In, Kim Tae Hyuk, Kim Won Gu, Lim Dong-Jun, Kim Tae Yong, Kim Sun Wook, Kim Won Bae, Shong Young Kee, Chung Jae Hoon, Baek Jung Hwan. Thyroid: Official Journal of the American Thyroid Association.2018;28(12). CrossRef
- Active Surveillance for T1bN0M0 Papillary Thyroid Carcinoma Sakai Toshihiko, Sugitani Iwao, Ebina Aya, Fukuoka Osamu, Toda Kazuhisa, Mitani Hiroki, Yamada Keiko. Thyroid: Official Journal of the American Thyroid Association.2019;29(1). CrossRef
- Analysis of the rising incidence of thyroid cancer using the Surveillance, Epidemiology and End Results national cancer data registry Cramer John D., Fu Pingfu, Harth Karem C., Margevicius Seunghee, Wilhelm Scott M.. Surgery.2010;148(6). CrossRef
- Management of Low-Risk Papillary Thyroid Cancer Iñiguez-Ariza Nicole M., Brito Juan P.. Endocrinology and Metabolism.2018;33(2). CrossRef
- Active Surveillance of Papillary Thyroid Microcarcinoma: Where Do We Stand? Jeon Min Ji, Kim Won Gu, Chung Ki-Wook, Baek Jung Hwan, Kim Won Bae, Shong Young Kee. European Thyroid Journal.2019;8(6). CrossRef
- The impact of age and gender on papillary thyroid cancer survival Jonklaas J., Nogueras-Gonzalez G., Munsell M., Litofsky D., Ain K. B., Bigos S. T., Brierley J. D., Cooper D. S., Haugen B. R., Ladenson P. W., Magner J., Robbins J., Ross D. S., Skarulis M. C., Steward D. L., Maxon H. R., Sherman S. I.. The Journal of Clinical Endocrinology and Metabolism.2012;97(6). CrossRef
- Improved detection does not fully explain the rising incidence of well-differentiated thyroid cancer: a population-based analysis Morris Luc G. T., Myssiorek David. American Journal of Surgery.2010;200(4). CrossRef
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times