Evaluation of the Association of Indoor Living Conditions and External Work Environment with Epidemiology, Baseline Demographic and Molecular Characteristics of Lung Cancer in North India
Download
Abstract
Introduction: Lung cancer has emerged as a global problem with the highest recorded mortalities amongst all types of cancer. There are multiple etiological factors associated with lung cancer such as smoking, environmental pollution, occupational exposure to carcinogens etc. Increase in lung cancer incidence among non-smokers is generally attributed to environmental pollution and occupational exposure. Also, an increase in the percentage of patients with targetable oncogenic drivers has been observed.
Methods: Here, we evaluated the effect of domestic conditions on epidemiology, baseline demographic and molecular characterization of lung cancer in India. For this data about domestic conditions such as housing type, kitchen type, fuel type, ventilation conditions and occupation was available from April 2018 to December 2019.
Results: Clinicopathological parameters of 1689 newly diagnosed lung cancer patients over the period of 3 years were recorded. Median age was 60.0years and 74.0% patients were smokers. The analysis data set for domestic conditions included 1018 patients. Working environment (indoor versus outdoor environment) had an association with lung cancer histology. 64.5% of lung cancer cases were found in people working in open outdoor environment (construction site workers, labourer, Farmers etc). People working in a closed office environment and housewives had higher frequency of adenocarcinoma and activating EGFR mutation and ALK rearrangement.
Conclusion: Domestic conditions and working environment not only selectively impact the lung cancer histology frequency but may also affect the frequency of oncogenic mutations and gene rearrangement.
Introduction
Lung cancer is the most frequently diagnosed cancer- type and leading cause of cancer related mortality worldwide [1]. In 2018, lung cancer constituted 11.6% of all newly diagnosed cancers with high mortality (accounting for 18.4% all cancer related deaths across the globe). In India, lung cancer stands at fourth position preceded by oral cancer, breast and cervical cancer. It is the third most common cause of cancer related mortalit [2]. Histopathologically, lung cancer can be divided into two major subtypes: non-small-cell lung cancer (NSCLC) and small-cell lung cancer (SCLC). NSCLC can further be sub-divided into squamous cell carcinoma (SCC), adenocarcinoma (ADC), and no other specific (NOS) subtype [3]. Earlier male gender accounted for majority of lung cancer cases with SCC subtype being most frequently diagnosed. Over the past decade, a changing trend in smoking patterns and histology trends, variable geographic clinico‑epidemiological profile, molecular characteristics, and treatment responses has been observed [4]. A significant rise in cases of lung cancer among women has been observed which is a major concern. Due to lack of effective early lung cancer screening program, most patients present at late stages resulting in poor outcomes. Availability of targeted therapies against recurrent mutations in EGFR gene as well as ALK and ROS1 gene rearrangements has significantly improved the overall survival in patients harboring these oncogenic drivers [5].
Smoking remains the major risk factor associated with lung cancer as 80% of the patients present with a smoking history (current or former smokers), but this is changing now [6]. Lung cancer cases among non-smoker females are becoming an important concern in developing countries [7, 8]. An overall decline in smoking prevalence among lung cancer patients has been observed in developed countries. Whereas risk of developing lung cancer due to outdoor pollution, household pollution, use of solid fuel for cooking/heating and second hand smoking has increased [9, 10]. Multiple risk factor, which are genetic and external factors (environmental & occupational) are associated with lung cancer [5]. The proportion of lung cancer cases attributable to preventable risk factors vary greatly across countries [11, 12]. Various research studies have associated lung cancer with active and passive smoking, occupational agents, indoor and outdoor air pollution [13]. This study was aimed to evaluate the effect of domestic conditions and working environment on epidemiology, baseline demographic and molecular characteristics of lung cancer patients presenting to our institute.
Materials and Methods
Patient enrollment
All the newly diagnosed cases of lung cancer, aged 18 years or above, attending Lung Cancer Clinic of PGIMER, Chandigarh from 1st April, 2017 – 31st December, 2019 were included. As per the normal protocol of our LC clinic, all patients were registered only after LC diagnosis was confirmed by histopathological and/or cytological examination of representative tissue specimens at the authors’ institute [1, 14]. Patient details such as age, gender, smoking status, tumor sample type and treatment history were recorded. To assess the impact of living condition on lung cancer patients were asked to fill a designated performa (supplementary 1). Briefly, data about their housing type whether residing in a concrete/ wood based house or mud straw based house; kitchen type that is open kitchen (kitchen which are open from all sides and without a roof), semi-open (supported by walls at least at one side and a roof) or closed kitchen (walls separating kitchen from rest of the house forming a room of its own) was recorded. Based on type of cooking fuel used, households were categorized into four categories: LPG based, wood based, mixed type (LPG + wood/coal/ cow- dung cake) and others (cow-dung cake, coal, biogas). Ventilation conditions in house and kitchen were classified as well-ventilated with option of windows and ventilators for proper air circulation in rooms and chimney/exhaust fan in kitchen, or inadequate ventilation. Based on occupation, patients were grouped into four categories: indoor (working in closed office environment), outdoor (working in open environment such as labourers, masons, drivers etc), house-wives and farmers.
Histological classification
All cases of lung cancer were classified histologically on the basis of morphology and relevant immunochemistry, as deemed appropriate, by the use of the IASLC/ATS/ ERS classification of lung tumors into: Adenocarcinoma, Squamous cell carcinoma, NSCLC-NOS, Small cell lung cancer (SCLC) [3].
Molecular profile
All cases of adenocarcinoma and selected cases of non- adenocarcinoma NSCLC (never-smokers, females) were tested for presence of EGFR gene mutations using EntroGen EGFR mutation analysis kit for Real Time PCR as per manufacturer protocol and ALK gene rearrangements were analyzed on a VENTANA BenchMark XT or BenchMark GX immunohistochemical automated slide stainer using VENTANA anti-ALK (D5F3) Rabbit Monoclonal Primary Antibody (VENTANA anti-ALK (D5F3)).
Statistical analysis
Statistical analysis was performed using the statistical software SPSS version 22.0 (SPSS Inc., Chicago, IL, USA). Data were expressed as the mean ± standard deviation (SD) or median (interquartile range [IQR]) or as number (percentages). Continuous and categorical variables in two groups were compared using Mann–Whitney U-test and Chi-square/Fisher’s exact test, respectively. Multivariate logistic regression analysis was performed for factors associated with domestic condition, histology, EGFR mutation and ALK rearrangement with 95%CI. For all analyses P<0.05 was considered significant.
Results
During the time period (April 2017- December 2019) a total of 1689 newly diagnosed lung cancer patients were enrolled in the study. Among these 1352 were males and 337 were females with male to female ratio of 4:1 (Table 1).
| Baseline characteristics | n (%) |
| Age | |
| Mean (SD) | 60 (±10.15) |
| Median(IQR) | 62 (54-67) |
| Gender | |
| Male | 1352 (80.0) |
| Female | 337 (20.0) |
| Smokers | 1254 (74.2) |
| Male | 1148 (91.5) |
| Female | 106 (8.5) |
| Histology | |
| SCC | 639 (37.8) |
| ADC | 691 (40.9) |
| NOS | 165 (9.8) |
| SCLC | 164 (9.7) |
| EGFR Mutation (n= 553) | 166 (30.0) |
| ALK Rearrangement (n=449) | 39 (8.7) |
| ROS1 Rearrangement (n= 260) | 6 (2.3) |
3.9% patients were between age group 18-40, 41.5% in 41-60 and 53.1% in 61- 80 age group. 1.4% patients were above 80 years of age. Mean and Median age were 60.0(SD ±10.2) and 62.0 (IQR 54-67) years, respectively. 74.2% patients were smokers of which 91.5% were males and 8.5% were females. Smoker to non-smoker ratio was 3:1. Histologically, 37.8% were SCC, 40.9%ADC, 9.8% NOS and 9.7% SCLC. EGFR mutation analysis was done in 553 patients of whom 30.0% were found to be harboring an EGFR mutation (60.3% males and 39.7% females). Among patients tested positive for EGFR mutations 38.5% were smokers. Frequency of EGFR mutation among non-smokers was significantly higher than smoker (p<0.008). ALK rearrangement analysis was done in 449 patients, with 8.7% positive cases (77.3% males and 22.7% females), 10.2% were smokers. Rearrangement for ROS1 gene was analyzed in 260 patients and 2.3% were positive for ROS1 rearrangement (Table 1).
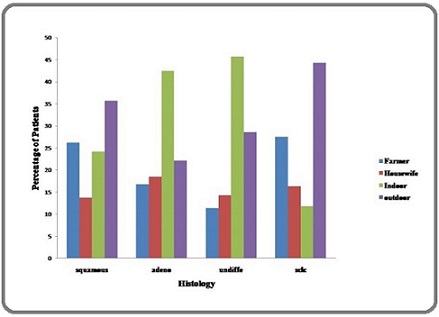
For assessment of the impact of domestic condition on lung cancer incidence, data about housing type, kitchen type, fuel type, ventilation conditions and occupation from 1018 patients was available. Out of 1018 patients 69.6% resided in concrete house, 22.1% in mud straw based house and 8.3% in mixed type house. Majority (88.3%) of the house were well ventilated. Household kitchens To find the correlation between domestic condition and lung cancer histology frequency, a multivariate logistic regression analysis was done. Histologically, people working in agriculture sector or under outdoor condition had SCLC and NSCLC-SCC as most common and frequently diagnosed subtype. Whereas, people working in indoor environment and house wives had higher frequency of NSCLC-ADC and NSCLC-NOS subtype (Figure 1).
Figure 1. Occupation-wise Histology of Patients.
Also, living and working conditions were compared with frequency of targetable EGFR mutations and ALK rearrangement among lung cancer patients. Housing type, ventilation conditions, kitchen type and fuel used for cooking has no statistically significant (p<0.2) impact on EGFR mutation frequency (Table 2).
| Parameters | EGFR mutation Positive n (%) | ALK rearrangement Positive n (%) |
| Housing type | ||
| a) Concrete house | 81 (69.8) | 14 (63.6) |
| b) Mud straw house | 26 (22.4) | 6 (27.3) |
| c) Mixed (concrete + mud-straw) | 9 (7.8) | 2 (9.1) |
| Ventilation in house | ||
| a) Adequate | 104 (89.6) | 18 (81.8) |
| b) Inadequate | 12 (10.4) | 4 (18.2) |
| Kitchen type | ||
| a) Open | 22 (19.0) | 4 (18.2) |
| b) Closed | 44 (37.9) | 13 (59.1) |
| c) Semi-open | 50 (43.1) | 5 (22.7) |
| Ventilation in Kitchen | ||
| a) Adequate | 101 (87.1) | 17 (77.3) |
| b) Inadequate | 15 (12.9) | 5 (22.7) |
| Fuel Used in Kitchen | ||
| a) LPG only | 62 (53.4) | 18 (81.8) |
| b) Wood/Coal/Cow-dung cakes | 11 (9.5) | 2 (9.1) |
| c) Mixed (LPG+ Wood/Coal/Cow-dung cakes) | 43 (37.1) | 2 (9.1) |
| Working conditions | ||
| a) Indoor Environment | 39 (33.6) | 5 (22.7) |
| b) Outdoor Environment | 31 (26.7) | 5 (22.7) |
| c) Farmer | 20 (17.3) | 9 (41.0) |
| d) Housewife | 26 (22.4) | 3 (13.6) |
However, people working in indoor conditions and housewives had a higher number of EGFR mutations as compared to people working in outdoor conditions and farmers. But, the difference was not statistically significant (p<0.6). Although housing type, ventilation conditions, kitchen type and kitchen ventilation had no impact on ALK rearrangement, but fuel type used in houses has a significant impact on frequency of ALK gene rearrangement as it was found to be higher in households using LPG as main cooking fuel (p<0.01). were categorized as open semi-open, closed and mixed type. 41.6% houses had semi-open kitchen followed by closed type kitchen (39.6%), open kitchen (18.3%) and mixed type (0.8%). In 82.7% houses kitchens were well ventilated. Type of fuel used in the household can give a rough idea about the levels of household pollution as biomass solid fuels (BSFs) are major contributers to the household air pollution in developing countries. 46.1% household use LPG as cooking fuel followed by mixed type (44.4%), wood (8.8%) and others (0.7%). Occupation wise, 43.3% patients worked in outdoor conditions followed by indoor environment (31.1%), farmers (21.2%) and house-wives (16.3%).
Discussion
This observational study sought to assess the association between epidemiology, demographic characteristics and molecular profile of lung cancer patients diagnosed at a tertiary care centre with variables related to domestic living conditions and external work environment. A shift in LC clinico-epidemiological profile over a decade has been observed [14]. In our previous publication, involving 1301 patients, it was observed that majority of the patients were males (82.3%) and current/ex-smokers (76.9%). Whereas, in the present study a slight decrease in the number male patients (80.0%) and a corresponding increase in female patients was observed. Previously, ADC and SCC (36.4% each) were equally prevalent. Whereas, now an increase in number of ADC cases over SCC was seen. In concordance with our previous reports, number of patients with ADC histology are increasing (40.9% vs 36.4% vs. 27.5%) [14]. Smoking is most common risk factor associated with lung cancer. Tobacco contains minimum of 50 carcinogens in addition to other hazardous compounds such as oxidative gases, cyanide, heavy metals [15, 16]. Various studies have shown that industrialization and smoking trend has a dismal impact on lung cancer epidemiology in India. Gender based smoking habits reflect the epidemiologic changes in the lung cancer incidence [13]. With the increasing trend of smoking among females, an increase in female lung cancer incidence has been observed. There is 10–30- fold relative risk of lung cancer in the smokers versus nonsmokers depending upon the smoking index [15]. Occupational exposure and environmental air pollution by waste burning, cooking, automobile, chimneys, and factories are also important contributory factors. Cancer incidence rate has been correlated to environmental pollution and occupational hazards but lung cancer is most important of them. In order to understand the effect of household environment and occupation (which is directly related to a person’s socioeconomic status) on lung cancer we gathered information on factors such as occupation, living conditions etc which contribute to domestic pollution.
Lung cancer has most commonly been linked with occupational exposures to the pollutants and socioeconomic status [13]. Similar observations were also seen in the present study as people associated with construction industry, manual labour, masons, drivers, carpenters, painters etc had high incidence of lung cancer compared to others. Many epidemiological studies, conducted in different countries, found significantly raised mortality rate for lung cancer among construction workers [17-20]. It is also seen that longer exposure to diesel exhaust put drivers at greater risk towards lung cancer.
Histologically, a contrast was observed among people belonging to different occupations. People working in a closed office environment or house‑wives tend to develop NSCLC-ADC subtype more frequently as compared to people working in agriculture industry, construction site etc which had high frequency of SCC and SCLC. This is in corroboration to the observations made by a study which evaluated the impact of socioeconomic status on lung cancer incidence. They observed that people with high socioeconomic status had higher incidence of ADC whereas those with lower socioeconomic status had higher incidence of SCC and SCLC [17]. Likewise frequency of activating mutations like EGFR and ALK were higher among people working indoor and agriculturist compared to people working in outdoor conditions and housewives. Hence, it can hypothesized that smoking habits and type of pollution at work place or inside home not only affect the lung cancer incidence but may also influence the histology favored and frequency of targetable activating mutations in EGFR and ALK rearrangement.
In addition to occupational exposure, emissions from biofuel used for cooking especially biomass solid fuels (BSFs) contribute to a significant amount of air pollutants, which are now recognized for their role in climatic change and adverse human health impacts. A study proposed that prolonged exposure to emissions from BSFs can increase the risk to cancer. In this study a increased incidence of lung cancer was observed among patients who use both LPG and BSFs as cooking fuel [21]. This observation could also be attributed to the fact that in majority of the households (as recorded in present study) use both LPG and BSFs as cooking fuel.
Categorization of patients based on their living conditions and occupation only tells us about possible pollutants to which the patient might have been exposed. Limitation of this study is absence of information about exposure probability, intensity, duration and other risk factors. In conclusion, occupational exposure (or in other word the socioeconomic status) and domestic environment may impact the lung cancer incidence and histology. To substantiate this hypothesis a longitudinal study is needed to be done.
Acknowledgments
Statement of Transparency and Principals:
• Author declares no conflict of interest
• Study was approved by Research Ethic Committee of author affiliated Institute.
• Study’s data is available upon a reasonable request.
• All authors have contributed to implementation of this research.
References
- Management of advanced lung cancer in resource-constrained settings: a perspective from India Singh N, Aggarwal AN , Behera D. Expert Review of Anticancer Therapy.2012;12(11). CrossRef
- Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries Bray F, Ferlay J, Soerjomataram I, Siegel RL , Torre LA , Jemal A. CA: a cancer journal for clinicians.2018;68(6). CrossRef
- The IASLC Lung Cancer Staging Project: proposals regarding the relevance of TNM in the pathologic staging of small cell lung cancer in the forthcoming (seventh) edition of the TNM classification for lung cancer Vallières E, Shepherd FA , Crowley J, Van Houtte P, Postmus PE , Carney D, Chansky K, Shaikh Z, Goldstraw P. Journal of Thoracic Oncology: Official Publication of the International Association for the Study of Lung Cancer.2009;4(9). CrossRef
- Unchanging clinico-epidemiological profile of lung cancer in north India over three decades Singh N, Aggarwal AN , Gupta D, Behera D, Jindal SK . Cancer Epidemiology.2010;34(1). CrossRef
- Feasibility of lung cancer screening in developing countries: challenges, opportunities and way forward Shankar A, Saini D, Dubey A, Roy S, Bharati SJ , Singh N, Khanna M, Prasad CP , Singh M, Kumar S, Sirohi B, Seth T, Rinki M, Mohan A, Guleria R, Rath GK . Translational Lung Cancer Research.2019;8(Suppl 1). CrossRef
- Current status of tobacco policy and control Paoletti L, Jardin B, Carpenter MJ , Cummings KM , Silvestri GA . Journal of Thoracic Imaging.2012;27(4). CrossRef
- Epidemiology of lung cancer in India: focus on the differences between non-smokers and smokers: a single-centre experience Noronha V., Dikshit R., Raut N., Joshi A., Pramesh C. S., George K., Agarwal J. P., Munshi A., Prabhash K.. Indian Journal of Cancer.2012;49(1). CrossRef
- The relevance of "Nonsmoking-associated lung cancer" in India: a single-centre experience Krishnamurthy A., Vijayalakshmi R., Gadigi V., Ranganathan R., Sagar T. G.. Indian Journal of Cancer.2012;49(1). CrossRef
- Indoor air pollution and risk of lung cancer among Chinese female non-smokers Mu L, Liu L, Niu R, Zhao B, Shi J, Li Y, Swanson M, Scheider W, Su J, Chang S, Yu S, Zhang Z. Cancer causes & control: CCC.2013;24(3). CrossRef
- Household air pollution and lung cancer in China: a review of studies in Xuanwei Seow WJ , Hu W, Vermeulen R, Hosgood Iii HD , Downward GS , Chapman RS , He X, Bassig BA , Kim C, Wen C, Rothman N, Lan Q. Chinese Journal of Cancer.2014;33(10). CrossRef
- The use of common genetic polymorphisms to enhance the epidemiologic study of environmental carcinogens Rothman N., Wacholder S., Caporaso N. E., Garcia-Closas M., Buetow K., Fraumeni J. F.. Biochimica Et Biophysica Acta.2001;1471(2). CrossRef
- Environmental and heritable factors in the causation of cancer--analyses of cohorts of twins from Sweden, Denmark, and Finland Lichtenstein P., Holm N. V., Verkasalo P. K., Iliadou A., Kaprio J., Koskenvuo M., Pukkala E., Skytthe A., Hemminki K.. The New England Journal of Medicine.2000;343(2). CrossRef
- Quantified smoking status and non-small cell lung cancer stage at presentation: analysis of a North Indian cohort and a systematic review of literature Singh N, Aggarwal AN , Gupta D, Behera D, Jindal SK . Journal of Thoracic Disease.2012;4(5). CrossRef
- Evolving epidemiology of lung cancer in India: Reducing non-small cell lung cancer-not otherwise specified and quantifying tobacco smoke exposure are the key Kaur H., Sehgal I. S., Bal A., Gupta N., Behera D., Das A., Singh N.. Indian Journal of Cancer.2017;54(1). CrossRef
- Global and Regional Patterns of Tobacco Smoking and Tobacco Control Policies Islami F, Stoklosa M, Drope J, Jemal A. European Urology Focus.2015;1(1). CrossRef
- What proportion of lung cancer in never-smokers can be attributed to known risk factors? Sisti J, Boffetta P. International Journal of Cancer.2012;131(2). CrossRef
- Lung cancer and socioeconomic status in a pooled analysis of case-control studies Hovanec J, Siemiatycki J, Conway DI , Olsson A, Stücker I, Guida F, Jöckel K, Pohlabeln H, Ahrens W, Brüske I, Wichmann H, Gustavsson P, Consonni D, Merletti F, Richiardi L, Simonato L, Fortes C, Parent M, McLaughlin J, Demers P, Landi MT , Caporaso N, Tardón A, Zaridze D, Szeszenia-Dabrowska N, Rudnai P, Lissowska J, Fabianova E, Field J, Dumitru RS , Bencko V, Foretova L, Janout V, Kromhout H, Vermeulen R, Boffetta P, Straif K, Schüz J, Kendzia B, Pesch B, Brüning T, Behrens T. PloS One.2018;13(2). CrossRef
- The incidence of medically reported work-related ill health in the UK construction industry Stocks S. J., McNamee R., Carder M., Agius R. M.. Occupational and Environmental Medicine.2010;67(8). CrossRef
- A 26-year cohort mortality study of French construction workers aged 20 to 64 years Thuret A, Geoffroy-Perez B, Luce D, Goldberg M, Imbernon E. Journal of Occupational and Environmental Medicine.2007;49(5). CrossRef
- Occupational exposures, environmental tobacco smoke, and lung cancer Veglia F, Vineis P, Overvad K, Boeing H, Bergmann M, Trichopoulou A, Trichopoulos D, Palli D, Krogh V, Tumino R, Linseisen J, Steindorf K, Raaschou-Nielsen O, Tjonneland A, Gonzalez CA , Martinez C, Dorronsoro M, Barricarte A, Cirera L, Quiros JR , Day NE , Saracci R, Riboli E. Epidemiology (Cambridge, Mass.).2007;18(6). CrossRef
- Emission of black carbon from rural households kitchens and assessment of lifetime excess cancer risk in villages of North India Ravindra K. Environment International.2019;122. CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Environment and Cancer , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times