Epidemiological and Geographical Profile of Gall Bladder Cancer Patients from a Hospital-based Registry of Northern Gangetic Plains
Download
Abstract
Purpose: Gall bladder cancer (GBC) is one of the commonest and deadliest cancers of Northern and Eastern India. The absence of a population-based cancer registry in Uttar Pradesh and Bihar has resulted in a lack of statistical information even though data from several hospital-based registries suggests that incidence rates of GBC may be one of the highest in the world. We present the four-year data on GBC from our tertiary-level multispeciality hospital.
Materials & Methods: This is a retrospective and analytical study. All patients of histopathologically proven GBC over four years were included and geographic, demographic and clinical data was collected and presented. Follow up, where available, was used to assess survival at 12 months and factors affecting it.
Results: A total of 245 patients with GBC were diagnosed during the study period of which more than two-thirds were women. The majority of cases at our hospital were from the state of Uttar Pradesh with the highest number coming from the Eastern districts closer to the river Ganga and its tributaries. 26.5% of cases were early stage and surgically resectable, 19.6% were locally advanced and unresectable while 53.9% were metastatic at presentation. Age, stage and radical surgery as treatment had a significant association with survival at 12 months.
Conclusion: GBC has an extremely high incidence in the Northern plains of India. There is a high suspicion of its association with increasing pollution of the major rivers of the region. Early detection is crucial as definitive surgery is the only curative option with any significant improvement of survival.
Introduction
Gall bladder cancer (GBC) is one of the commonest as well as one of the deadliest cancers of the river basins of the Ganga and the Brahmaputra in Northern and Eastern India. It is the only gastrointestinal cancer that is more often seen in women than men and is the most frequent malignancy of the biliary tract [1, 2]. Globally, it contributes to only 1.2% of all newly diagnosed cancer cases annually [3]. But in India’s National Cancer Registry Programme (NCRP) report of 2014, it is in the top 10 leading sites of cancer in women in every one of the hospital based, as well as population based cancer registries of Northern and Eastern parts of the country, except Nagaland [4].
GBC is an aggressive disease with non-specific symptoms and lacks pathognomic clinical and radiological findings in the initial stages. It has an insidious course leading to delayed presentation in an advanced stage in 90% cases and a five year overall survival ranging from 0 to 10% [2, 4-6]. The disease has a multifactorial etiology with strong associations with cholelithiasis, gall bladder polyps, anomalous pancreatobiliary connections, chronic gall bladder infections and inflammation and exposure to environmental carcinogens [1,2,6]. It’s peculiar geographic distribution in our country with incidence rates in North India being ten times higher than South India, has been explained by the increasing industrial pollution of the Ganga and its tributaries. This has lead to exposure of the population residing in these river basins to heavy metals, pesticides, fertilizers and industrial effluents, all carcinogens implicated in causation of GBC [7-11].
Our tertiary level cancer centre caters to five India states – Uttarakhand (UK), Uttar Pradesh (UP), Bihar, Jharkhand and Madhya Pradesh (MP). The river Ganga and its tributaries flow through the first three of them and partially through the fourth. Absence of a population based cancer registry in the states of UP and Bihar has resulted in lack of statistical data from this region which is one of the most densely populated places in the world. Thankfully, several hospital based cancer registries are available and indicate that the region may have one of the highest recorded GBC incidence rates [11-13]. In this article, we are presenting the demographic and clinical profile of GBC patients seen at our tertiary care centre in Lucknow over three years. We have also tried to study the geographic distribution of our study populations in terms of their vicinity from the Ganga and its tributaries.
Materials and Methods
This was a retrospective analytical study. The schema of patient selection for the entire study population and for statistical analysis is shown at Figure 1.
Figure 1. Study Schema Showing Patient Selection.
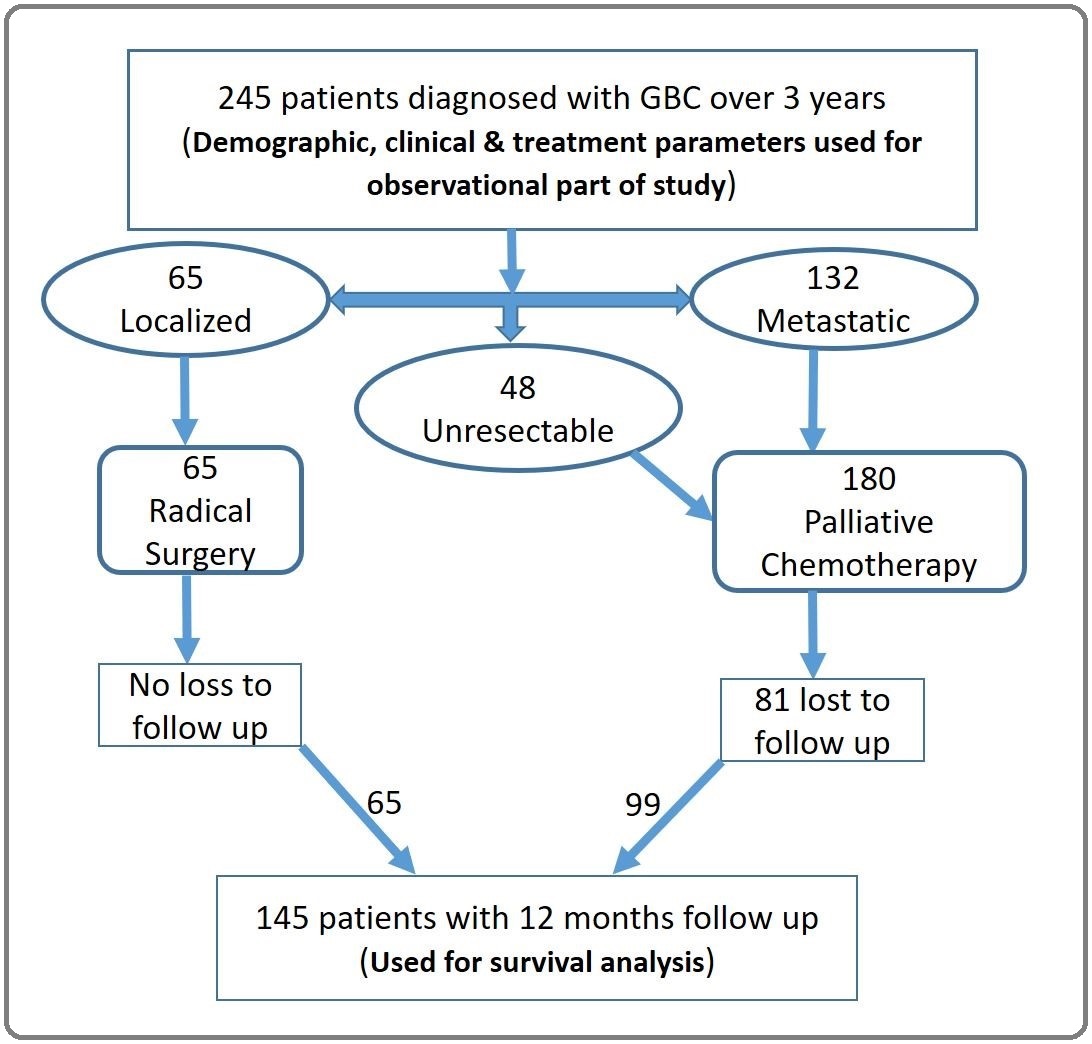
All patients of histologically proven GBC reporting to our hospital between August 2015 to July 2018 were included. The patients were classified into various demographic divisions based on gender, age group and district of residence. Though in our clinical evaluation, our institute uses the American Joint Committee of Cancer (AJCC) prescribed TNM staging (2007 edition), for the sake of simplicity, we divided our study cohort into localized (L), unresectable (U) and metastatic (M) based upon their clinico-radiological and in some cases, intra- operative findings. The L subgroup included patients who had local or lo-regional disease that was amenable to curative surgical resection. The subgroups U and M are self-explanatory. Patients were also classified into the type of treatment they received, either as curative (C) or palliative (P). Only patients who underwent radical surgery with or without adjuvant chemo/radiotherapy were included in the C group while P group included patients who received palliative chemotherapy, radiotherapy or supportive care alone. Survival of patients at 12 months from diagnosis was recorded and compared between different variable groups. Data was analyzed using frequency distribution, crosstabs, Kaplan-Meier survival curves and pie and bar diagrams by Statistical Product and Service Solutions version 20 (SPSS 20, IBM, Armonk, NY, USA). Geographico-political maps were used to display distribution of patients as per their districts of residence. We also compared the total number of incidental GBC picked up during cholecystectomies done for benign reasons.
Results
A total of 245 patients of GBC were registered with our hospital between Jan 2015 to Dec 2018. Table 1 shows the distribution of study parameters amongst the study population.
| Study Parameters | Range | n | % |
| Age in Years | 31-50 | 57 | 23.3 |
| 51-70 | 151 | 61.6 | |
| >70 | 37 | 15.1 | |
| Gender | Female | 167 | 68.2 |
| Male | 78 | 31.8 | |
| Stage | Local | 65 | 26.5 |
| Unresectable | 48 | 19.6 | |
| Metastatic | 132 | 53.9 | |
| Surgery | Total | 99 | 40.4 |
| Radical | 65 | 26.5 (65.7)* | |
| Palliative | 34 | 13.9 (34.3)* | |
| Chemotherapy | Total | 152 | 62.04 |
| Neoadjuvant | 5 | 0.02 (3.2)* | |
| Adjuvant | 54 | 22.02 (35.5)* | |
| Palliative | 98 | 40 (64.5)* | |
| Radiotherapy | Total | 11 | 4.5 |
| Adjuvant | 4 | 1.6 (36.4)* | |
| Palliative | 7 | 2.9 (63.6)* | |
| Intent of Treatment | Radical | 65 | 26.5 |
| Palliative | 180 | 73.4 | |
| Total | 245 |
* The figure outside parentheses represents percentage of full study population while the figure within parentheses represents percentage of the cohort receiving the specific treatment modality.
73% cases (178) were from the state of UP and only 01 (0.4%) case was from Jharkhand. Figure 2 shows the state-wise distribution of cases.
Figure 2. Number of Cases from each State.
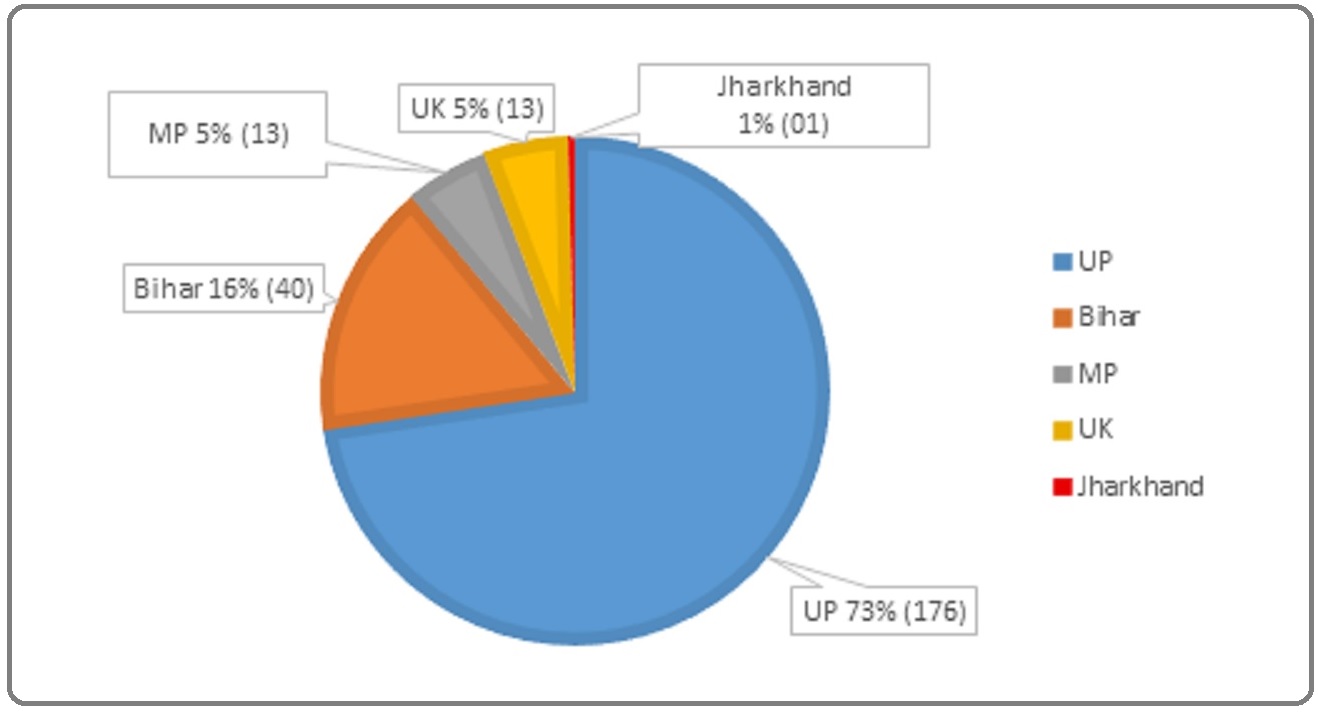
Figure 3 shows the map of UP with the distribution of cases from the state as per their district of residence and in relation to the river Ganga and it’s tributaries.
Figure 3. District Wise Distribution of GBC Cases in the State of Uttar Pradesh (Each Red Dot Represents a Case from the Respective District).

Out of the total 245 patients, complete follow up details for a minimum of 12 months from diagnosis was available for 164 patients. Univariate analysis of association of age, gender, stage and surgery with overall survival (OS) and plotting of survival curves was carried out for these 164 patients. Table 2 and Figure 4 show the results of the statistical analysis.
| Factors | n | OS at 1 year (%) | p Value | |
| Age in Years | 31-50 | 37 | 73 | 0 |
| 51-70 | 99 | 61.6 | ||
| >70 | 28 | 28.6 | ||
| Gender | Female | 112 | 61.6 | 0.162 |
| Male | 52 | 51.9 | ||
| Stage | Local | 65 | 85.9 | 0 |
| Metastatic | 59 | 18.6 | ||
| Unresectable | 40 | 0 | ||
| Radical Surgery (Sx) | Yes | 65 | 85.9 | 0 |
| No | 99 | 16.9 | ||
| Total | 164 | 58.5 |
Statistical analysis carried out only for patients for whom minimum follow up of 12 months was available.
Figure 4. Kaplan Meier Survival Plots for Overall Surviva at 12 Months.
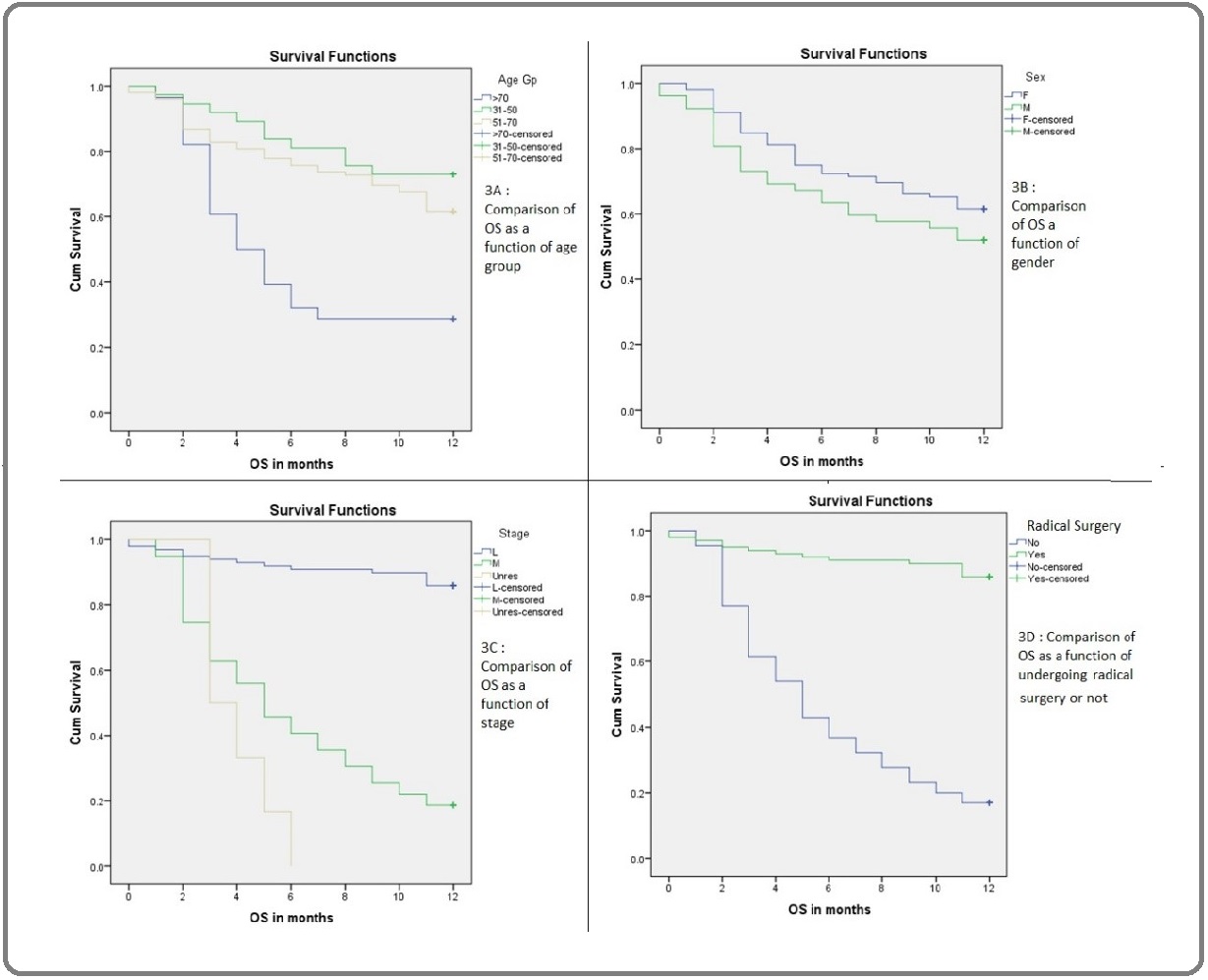
Figure 5 shows the total number of gall bladder surgeries done annually at our centre during the study period and the percentage of those surgeries that were done for GBCs.
Figure 5. Annual Gall Bladder Surgeries Done at Our Centre.
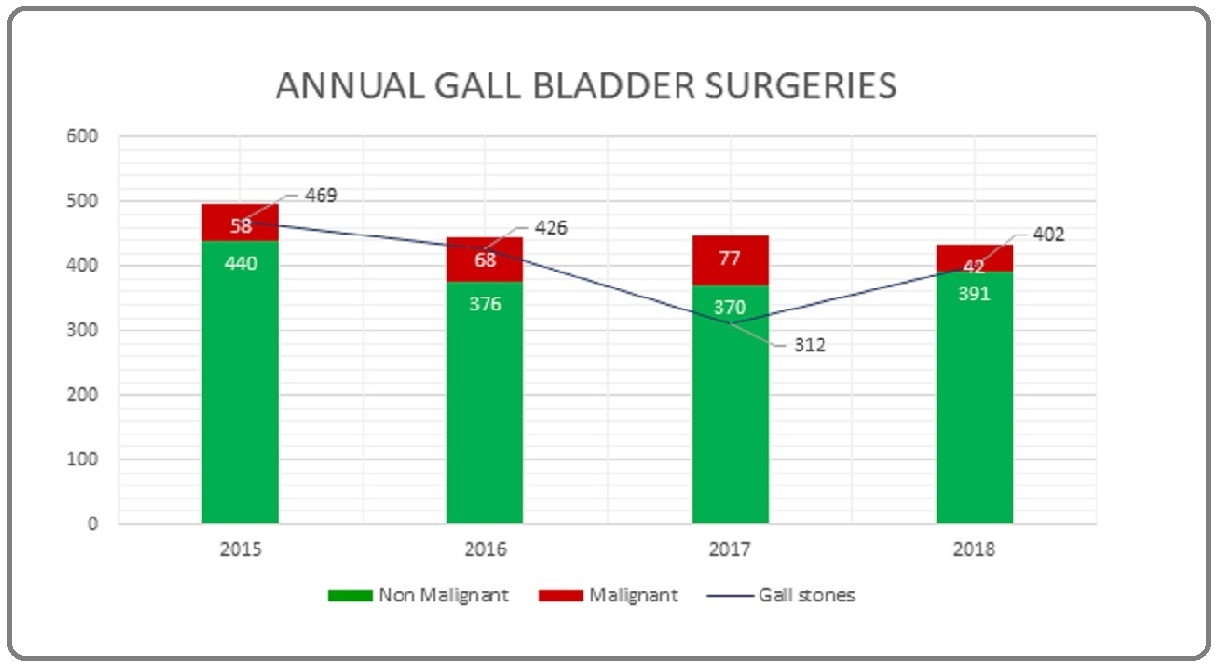
It also shows the total number of patients who underwent gall bladder surgeries, both for benign and malignant causes, that were found to be suffering from cholelithiasis on histopathological examination.
Discussion
Gall bladder cancers are one of the deadliest cancers of the biliary tract with a widely variable geographic distribution. Uncommon elsewhere, it shows high rates of incidence in Central and South America, Eastern Europe and South East Asia. Globocan 2018 figures put GBC as the 22nd most common cancer worldwide with 2,19,420 new cases (1.2% of all malignancies) and 1,65,087 deaths (1.7% of all cancer related mortality). Though the overall Age Specified incidence rate (ASR) in our country is only 2.5 per 100,000, which appears safely below the highest ASR of 14.0 of Bolivia, due to our voluminous population, India has the second highest number of gall bladder cases occurring annually after China. In 2018, this figure was close to 26,000 with nearly 20,000 deaths being attributed to this disease [3].
Within India too, the disease shows a characteristic distribution pattern. It is more prevalent in the Northern and Eastern states in the basins of the Ganga and Brahmaputra rivers. As per NCRP reports of 2013- 14, the highest ASR of 17.1 per 100,000 females has been reported by the population registry in Kamrup, Assam. This is one of the highest in the world. Even amongst hospital based registries, Silchar, Assam has the highest incidence of 15.8 amongst females. Other Eastern states like Manipur, Meghalaya and Sikkim also show high incidence [4]. Similar high incidence of GBC has also been reported in various studies from the Gangetic plains of UP and Bihar [10-14]. The migrant population from these 2 states possibly also contributes to the high incidence rates of Delhi and Mumbai [4, 15]. The etiology of GBC can be described under four heads :
a) Demographic factors: Advanced age, obesity, female gender, multiparity, geography (South American, North & East Indian, Korean, Japanese, East Europeon) & genetic predisposition
b) Gall bladder pathologies and abnormalities: Cholelithasis, chronic inflammation, porcelain bladder, gallbladder polyps, pancreaticobiliary maljunction abnormalities & congenital biliary cysts
c) Exposure to carcinogens: Heavy metals, insecticides, fertilizers, estrogen, smoking & alcohol
d) Infections: Salmonella & Helicobacter.
The prevalence of these risk factors can be used to explain the geographic distribution of GBC [16-20]. The strongest risk factor for GBC appears to be a high prevalence of gallstones in the population. Several studies have shown such a high prevalence of cholelithiasis in the northern and eastern Indian states and it’s strong association with GBC [10,11,21-22]. Similarly, the worldwide distribution of high gallstone prevalence shows a strong positive correlation with higher incidence rates of GBC in populations in South America and parts of Europe [1]. Interestingly, the higher incidence of GBC in South East Asia (China, Japan and Korea) appears to be related to the higher incidence of congenital malformations in pancreato-biliary junctions and are not associated with cholelithiasis. In our study too, a very high prevalence of gall stones was seen in the patients undergoing gall bladder surgeries (Figure 5).
The GANGA (Gallbladder Abnormalities in Northern Gangetic Area) study group identified drinking unprotected water with high levels of heavy metal pollutants and eating excess chickpeas (chana) as risk factors for developing gall bladder disease (GBD) [10]. Rapid industrialization and liberalization of India in the past two decades has led to an increase in the effluents being released in our rivers. Pollution of river water with heavy metals and industrial chemicals are the suspected cause for rise in number of cancer cases [8]. High concentrations of chromium, zinc, arsenic, lead, nitrate fertilizers and pesticides like DDT and BHC have been found in the biliary tracts of GBC cases in this region [23-25]. Overall, there is an increasing trend in the incidence in GBCs over the past 25 years [26]. As nearly 3/4th of our study population was from UP, we compared the geographical distribution of cases by projecting them on map displaying the districts of the state along with the river Ganges and its tributaries (Figure 2). On visual examination two things are clearly apparent. One is that 63% of the cases are residents of districts through which the Ganga and its two major tributaries, the Yamuna and the Gomti pass through. All three rivers are considered to be some of the most heavily polluted in the world. Populations living in the vicinity of these rivers are likely to be exposed to carcinogens like heavy metals, pesticides, fertilizers as well as bacterial and salmonella infections increasing their risk of gallstone disease and GBC. The second thing noted from the map is that the cases from districts in the eastern part of the state are much more numerous than cases from districts in the western and northern parts. One possible reason contributing to the easterly distribution of cases could be a sort of proximity bias in that the patients from the western parts of the state may have a tendency to travel to Delhi to seek medical help, rather than Lucknow, as Delhi is physically closer to the western districts. However, this could also be in part because the pollution levels of the rivers is likely to be higher in the eastern districts, as the Ganga and its tributaries flow from north-west to east, collecting polluting effluents as they do so.
The district with the highest number of cases (17) in our study is Lucknow which has the river Gomti passing through it. Lucknow also happens to be the capital city of the state of UP and the city in which our hospital is situated. Therefore, it is probable, that few patients may have recorded Lucknow as their district of residence but may have travelled from other districts and may be staying in Lucknow only for the duration of their treatment. Lucknow is neither the most densely populated nor the most polluted district within UP. Incidentally, GBC is the commonest cause of malignant obstructive jaundice in Lucknow [27].
With the advent of molecular diagnostics, research is also being conducted to detect any genetic predispositions towards GBC. Genes like KRAS, C-erb-B2, TP53, hTERT (human telomerase reverse transcriptase), cholecystokinin type-A, and several more have been studied and implicated in the etiology of GBC but the true molecular pathway and genetic marker are yet to be discerned [28, 29]. This should be the direction of future studies.
We had a total of 1822 gall bladder surgeries over four years at our institute of which 245 (13.44%) were for malignant diseases. These surgeries included cholecystectomies, extended-cholecystectomies, biliary diversion and drainage procedures and laparoscopic and image-guided tissue biopsies. A very high proportion of patients under going gall bladder surgeries were found to be affected by gall stones.
Gallstones and GBC are both globally more common in women with a female to male ratio for GBC ranging from 1.2 to 3 in various studies [1-4, 6,10]. In our study population, women were 2.14 times more numerous than men. Gender did not significantly affect the survival outcome of patients at 12 months from treatment (Figure 3B). Along with female gender, obesity, multiparity and use of Oral Contraceptive Pills (OCPs) have also been found to be risk factors for GBCs, indicating a potential role of estrogen in the etiopathogenesis [1,13,18].
Older age is also considered a risk factor for GBC with maximum cases presenting in the fifth and sixth decades of life. In fact, the incidence starts to increase after 45 years and reaches a peak at 65 years [7,10,12]. The age range in our study cohort was from 34 years to 90 years with a mean age of nearly 60 years for both genders. The cohort was divided into three age groups to study the influence of age on survival outcomes (Figure 3A). Though there was no significant difference between the patients who were less than 50 years or were between 50 to 70 years, there was a significantly poorer survival at 12 months in patients who were above 70 years of age. This is likely reflective of the poorer general condition and greater accumulation of comorbidities in the septuagenarian age group which would have made tolerance of radical therapies difficult. Also, the percentage of patients with localized and resectable disease varied between 45% for 30 to 50 years, to 42.4% for 50 to 70 years and only 24% for the above 70 years age group. This late presentation of the oldest age group was possibly because of the early symptoms of GBC being confused with co-morbid conditions or neglected by the caregivers.
Stage is the most important determinant of prognosis and outcomes of GBC patients with 5 year survivals varying from 60% for carcinoma in situ (Tis) to 39% for stage I and dropping to 1% for stage IV disease [30]. GBCs usually have an insidious onset with vague and non-specific symptoms like abdominal pain or distension, nausea, dyspepsia, anorexia and jaundice. In India, this often leads to a delay in seeking medical help and in subsequent diagnosis, resulting in 80 to 90% patients presenting in an advanced metastatic or unresectable state, frequently diagnosed at the time of ultrasonogram for the previously described upper abdominal symptoms [2,5,6,12]. In various series, only between 5 to 20% patients of GBC are detected in an early stage and are amenable for curative surgical resection. In our study population, 65 patients (26.5%) were in the localized (L) sub-group while 48 (19.5%) were non-metastatic but unresectable (U). More than half the patients, i.e., 132 (53.9%) had distant metastases at presentation.
GBC is a malignancy with one of the most aggressive natural courses and one with the shortest median survival from diagnosis. Radical surgery is the only curative option available and those who do undergo curative surgery have a median survival of 12 months and a five-year survival between 0 to 10% [2,5,6,12,31]. In our study, 99 patients underwent surgery of which 65 (26.5%) had radical surgery. The other 34 (13.8%) patients were those who underwent palliative surgical procedures for biliary bypass or drainage.
As described in literature, stage, as a measure of operability, had a statistically significant impact on survival (Figure 3C) with OS at 12 months dropping from 85% for L to 18.6% for M and 0% for U subgroup. Radical surgery had a clearly evident and statistically significant impact on OS as seen in the survival plot in Figure 3D. In fact, the plot is the same as the localized disease survival plot because these were the patients who underwent radical surgery. The OS at 01 year for the L group or radical surgery was 85.9% compared to 16.9% for the combined U and M sub-groups.
The relatively high percentage of cases with localized disease and radical surgery seen in our cohort (26.5%) compared to other series (10 to 20%) can be attributed to efficient diagnostic facilities and referral network available in the form of peripheral hospitals distributed in the drainage area of our tertiary care centre. Despite being a central government hospital, the clientele of our institute is limited to a specific socio-economic group (Armed Forces personnel and their families). Hence, the resource to recipient ratio in terms of healthcare facilities is expected to be better than the general population. Waiting times for investigations and surgeries are also shorter than majority of government institutes.
Use of adjuvant chemotherapy in post-op setting has shown improvements in OS and DFS in patients of GBC [32, 33]. The benefit of use of adjuvant radiotherapy is less clear [34-35]. In our study 54 out of 65 (83.1%) patients undergoing curative surgery also received adjuvant chemotherapy, with 3 of them also receiving adjuvant radiotherapy. The most commonly used regimens were single agent capecetabine, gemcitabine or a combination of one of these two with a platinum agent. 11 patients could not be offered adjuvant chemotherapy in view of their poor performance status or co-morbidity profile. A small subset of 06 patients also received neoadjuvant chemotherapy before surgery. Use of neoadjuvant chemotherapy in locally advanced and borderline resectable GBC has shown good rates of response and curative resection [36]. Only patients who could undergo radical surgery were considered in the curative group and rest were treated with palliative intent. The palliative group comprised of 73.5% (180) of the total cohort. The various treatments used for these patients were palliative surgery (biliary drainage) in 34, palliative chemotherapy in 98 and palliative radiotherapy in 7 patients. The palliative chemotherapy regimens used were a combination of oxaliplatin with either gemcitabine or capecitabine. One-third of the total cohort and 45% of the palliative group, i.e., 82 patients were unfit for any oncological management due to old age, co-morbidities or poor general condition. They were offered only supportive care at home or hospice.
Limitations of the Study
Our data has been collected retrospectively. As mentioned earlier, some patients may have incorrectly given their place of residence as the city they were staying in during treatment. Another point that may have erroneously affected estimation of survival statistics is that the 164 patients of which 12 month follow up data is available, include all 65 of those with localized disease that underwent radical surgery but only 50% patients of those who received palliative treatment. Thus, the cohort used for survival estimation contained a greater proportion of patients with localized disease (and hence, better prognosis) than the actual full study population.
In conclusion, gall bladder cancer is a commonly seen malignancy in northern Gangetic plains of India. Rising levels of river water pollution is linked with the rising incidence of the cancer. A high percentage of these malignancies present in an advanced stage with limited treatment options and poor prognosis. In the known regions of high incidence, primary and secondary prevention strategies in the form reduction of industrial pollution and imaging based screening respectively need to be aggressively pursued to reduce the burden of this dreaded disease.
Acknowledgements
Malignant Disease Treatment Centre, Department of Radiology, Department of Nuclear Medicine, Department of Pathology, Command Hospital (Central Command), Lucknow.
References
- Gallbladder cancer worldwide: geographical distribution and risk factors Randi Giorgia, Franceschi Silvia, La Vecchia Carlo. International Journal of Cancer.2006;118(7). CrossRef
- Gallbladder cancer: epidemiology and outcome Hundal Rajveer, Shaffer Eldon A.. Clinical Epidemiology.2014;6. CrossRef
- Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries Bray Freddie, Ferlay Jacques, Soerjomataram Isabelle, Siegel Rebecca L., Torre Lindsey A., Jemal Ahmedin. CA: a cancer journal for clinicians.2018;68(6). CrossRef
- Indian Council of Medical Research. National centre for disease informatics and research. National cancer registry programme Three-year report of population based cancer registries 2012-2014. Consolidated Report of Hospital Based Cancer Registries 2012-2014.WWW page.2016. [Last accessed March 24, 2020]. URL: http://ncdirindia.org..
- Carcinoma of the gallbladder Misra Sanjeev, Chaturvedi Arun, Misra Naresh C., Sharma Indra D.. The Lancet. Oncology.2003;4(3). CrossRef
- Gallbladder Cancer in the 21st Century Kanthan Rani, Senger Jenna-Lynn, Ahmed Shahid, Kanthan Selliah Chandra. Journal of Oncology.2015;2015. CrossRef
- Indian Council of Medical Research consensus document for the management of gall bladder cancer Shukla Hari Shankar, Sirohi Bhawna, Behari Anu, Sharma Atul, Majumdar Jahar, Ganguly Manomoy, Tewari Mallika, Kumar Sandeep, Saini Sunil, Sahni Peush, Singh Tomcha, Kapoor Vinay Kumar, Sucharita V., Kaur Tanvir, Shukla Deepak Kumar, Rath Goura Kishor. Indian Journal of Medical and Paediatric Oncology: Official Journal of Indian Society of Medical & Paediatric Oncology.2015;36(2). CrossRef
- Cancer trends and burden in India Krishnatreya Manigreeva. The Lancet. Oncology.2018;19(12). CrossRef
- Gallbladder Carcinoma: A Reason to Worry in North and North-Eastern India. Routh D. Clin Surg.2017;2:1661.
- Population-based study to estimate prevalence and determine risk factors of gallbladder diseases in the rural Gangetic basin of North India Unisa Sayeed, Jagannath Palepu, Dhir Vinay, Khandelwal Chiranjeeva, Sarangi Lalatendu, Roy Tarun Kumar. HPB: the official journal of the International Hepato Pancreato Biliary Association.2011;13(2). CrossRef
- Geographical pattern of carcinoma gallbladder in Bihar and its association with river Ganges and arsenic levels: Retrospective individual consecutive patient data from Regional Cancer Centre Madhawi Richa, Pandey Avinash, Raj Shraddha, Mandal Manish, Devi Seema, Sinha Prabhat Kumar, Singh Rajesh Kumar. South Asian Journal of Cancer.2018;7(3). CrossRef
- (2018) Carcinoma Gallbladder-Epidemiological Trends in a Tertiary Hospital in North India Lal M, Raheja S, Bhowmik KT. Arch Surg Oncol.131;4. CrossRef
- Carcinoma of gall bladder: Demographic and clinicopathological profile in Indian patients Dubey AP, Rawat K, Pathi N, Viswanath S, Rathore A, Kapoor R, et al . Oncol J India.2018;2:3-6. CrossRef
- Primary carcinoma of the gall bladder: a review of a 16-year period at the University Hospital Shukla V. K., Khandelwal C., Roy S. K., Vaidya M. P.. Journal of Surgical Oncology.1985;28(1). CrossRef
- Geographic patterns in incidence of Gall Bladder cancer in India and the possible etiopathological factors Jagannath P, Dhir V, Mohandas KM. HPB 2.2000;:168-169.
- Cancer: scenario and relationship of different geographical areas of the globe with special reference to North East-India Sharma Jagannath Dev, Kalit Manoj, Nirmolia Tulika, Saikia Sidhartha Protim, Sharma Arpita, Barman Debanjana. Asian Pacific journal of cancer prevention: APJCP.2014;15(8). CrossRef
- Risk Factors for Gallbladder Cancer : A Population Based Case-Control Study in Delhi Tyagi Brijbhushan, Raina Vinod. Indian journal of medical and paediatric oncology.2008;29. CrossRef
- Lifestyle, parity, menstrual and reproductive factors and risk of gallbladder cancer Pandey M., Shukla V. K.. European journal of cancer prevention: the official journal of the European Cancer Prevention Organisation (ECP).2003;12(4). CrossRef
- Risk factors for gallbladder cancer: a case-control study Jain Kajal, Sreenivas V., Velpandian T., Kapil Umesh, Garg Pramod Kumar. International Journal of Cancer.2013;132(7). CrossRef
- Risk factors for gallbladder cancer in Nepal a case control study Tamrakar D, Paudel I, Adhikary S, Rauniyar B, Pokharel P. Asian Pac J Cancer Prev.2016;17:3447-3453.
- Clinicopathological study of gall bladder carcinoma with special reference to gallstones: our 8-year experience from eastern India Hamdani Nissar Hussain, Qadri Sumyra Khurshid, Aggarwalla Ramesh, Bhartia Vishnu Kumar, Chaudhuri Sumit, Debakshi Sanjay, Baig Sarfaraz Jalil, Pal N. K.. Asian Pacific journal of cancer prevention: APJCP.2012;13(11). CrossRef
- Gall bladder cancer and some epidemiological factors: A cross sectional study Dwivedi S, Madeshiya A, Singh D, Singh S, Krishna A. Biomed Res.2013;24:83-87.
- Biliary heavy metal concentrations in carcinoma of the gall bladder: case-control study Shukla V. K., Prakash A., Tripathi B. D., Reddy D. C., Singh S.. BMJ (Clinical research ed.).1998;317(7168). CrossRef
- Biliary nitrate and risk of carcinoma of the gallbladder Shukla V. K., Prakash A., Chauhan V. S., Singh S., Puneet null. European journal of cancer prevention: the official journal of the European Cancer Prevention Organisation (ECP).2004;13(4). CrossRef
- Organochlorine pesticides in carcinoma of the gallbladder: a case-control study Shukla V. K., Rastogi A. N., Adukia T. K., Raizada R. B., Reddy D. C., Singh S.. European journal of cancer prevention: the official journal of the European Cancer Prevention Organisation (ECP).2001;10(2). CrossRef
- Gallbladder cancer incidence in Delhi urban: A 25-year trend analysis Malhotra Rajeev Kumar, Manoharan Nalliah, Shukla N. K., Rath Gourva Kishore. Indian Journal of Cancer.2017;54(4). CrossRef
- Palliative surgical treatment of malignant obstructive jaundice Sikora SS, Kapoor R, Pradeep R, Kapoor VK, Saxena R, Kaushik SP, et al . Eur J Surg Oncol.1994;20:580-584.
- Gallbladder cancer epidemiology, pathogenesis and molecular genetics: Recent update Sharma Aarti, Sharma Kiran Lata, Gupta Annapurna, Yadav Alka, Kumar Ashok. World Journal of Gastroenterology.2017;23(22). CrossRef
- Gallbladder cancer: epidemiology and genetic risk associations Schmidt Mikayla A., Marcano-Bonilla Lorena, Roberts Lewis R.. Chinese Clinical Oncology.2019;8(4). CrossRef
- The National Cancer Data Base report on carcinoma of the gallbladder, 1989-1995 Donohue J. H., Stewart A. K., Menck H. R.. Cancer.1998;83(12). CrossRef
- Gallbladder cancer in the world: epidemiology, incidence, mortality and risk factors Mahdavifar N, Mohammadian M, Salehiniya H. World Cancer Research Journal .2018;5(3):e1124.
- Capecitabine compared with observation in resected biliary tract cancer (BILCAP): a randomised, controlled, multicentre, phase 3 study Primrose John N., Fox Richard P., Palmer Daniel H., Malik Hassan Z., Prasad Raj, Mirza Darius, Anthony Alan, Corrie Pippa, Falk Stephen, Finch-Jones Meg, Wasan Harpreet, Ross Paul, Wall Lucy, Wadsley Jonathan, Evans Jeff T. R., Stocken Deborah, Praseedom Raaj, Ma Yuk Ting, Davidson Brian, Neoptolemos John P., Iveson Tim, Raftery James, Zhu Shihua, Cunningham David, Garden O. James, Stubbs Clive, Valle Juan W., Bridgewater John. The Lancet. Oncology.2019;20(5). CrossRef
- Is postoperative adjuvant chemotherapy useful for gallbladder carcinoma? A phase III multicenter prospective randomized controlled trial in patients with resected pancreaticobiliary carcinoma Takada Tadahiro, Amano Hodaka, Yasuda Hideki, Nimura Yuji, Matsushiro Takashi, Kato Hiroyuki, Nagakawa Takukazu, Nakayama Toshimichi. Cancer.2002;95(8). CrossRef
- Adjuvant therapy in the treatment of biliary tract cancer: a systematic review and meta-analysis Horgan Anne M., Amir Eitan, Walter Thomas, Knox Jennifer J.. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2012;30(16). CrossRef
- Palliative and postoperative radiotherapy in biliary tract cancer Macdonald O. Kenneth, Crane Christopher H.. Surgical Oncology Clinics of North America.2002;11(4). CrossRef
- Outcome of neoadjuvant chemotherapy in "locally advanced/borderline resectable" gallbladder cancer: the need to define indications Chaudhari Vikram A., Ostwal Vikas, Patkar Shraddha, Sahu Arvind, Toshniwal Anup, Ramaswamy Anant, Shetty Nitin S., Shrikhande Shailesh V., Goel Mahesh. HPB: the official journal of the International Hepato Pancreato Biliary Association.2018;20(9). CrossRef
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times