Role of Hospice Care Centre in a Resource Constraint Area for the Care of Terminally Ill Cancer Patients
Download
Abstract
Context: Cancer patients in advanced stages often face severe physical, psychological, and spiritual challenges, impacting their quality of life (QOL) significantly. Ganga Prem Hospice (GPH) in Uttarakhand, India, provides specialized palliative care aimed at improving end-of-life experiences for terminally ill cancer patients.
Objective: This study aimed to assess the effects of hospice-based palliative care on pain relief, symptom management, and QOL for terminal cancer patients.
Methods: This prospective study included 99 terminally ill cancer patients admitted to GPH from January 2022 to January 2023. Patient data collected included demographics, cancer stage, pain levels, symptom relief, QOL assessments, and place of death. Pain and symptom relief were assessed using the Visual Analog Scale (VAS), while QOL was categorized as “good” or “poor.” Descriptive statistics and comparative analysis were used to measure changes pre- and post-admission.
Results: The median age of patients was 49 years, with 58.6% male and 41.4% female representation. Advanced cancer stages (96.96% at Stage IV) were prevalent, with head and neck (34.34%), gastrointestinal (24.24%), and gynecological cancers (21.21%) as the most common types. Post-admission, patients reporting no pain increased from 4% to 23%, while 86% experienced symptom relief compared to 10% at admission. QOL improved markedly, with 86% of patients reporting good QOL after admission, up from 22% initially. The majority (72.6%) chose to remain at GPH for end-of-life care.
Conclusion: Palliative care at GPH significantly improved pain relief, symptom control, and QOL for terminally ill cancer patients, highlighting the essential role of hospice settings in end-of-life care, especially in resource-limited regions. These findings advocate for expanded hospice services to support both patients and families in terminal care.
Introduction
Cancer remains a significant global health challenge, with projections indicating that by 2040, around 16.3 million individuals will live with the disease, predominantly in low- and middle-income countries [1]. In these regions, cancer is often diagnosed during advanced stages, limiting treatment accessibility [2]. The symptoms associated with cancer can impact patients’ quality of life (QOL), causing physical discomfort, mental strain, and financial burdens [3-6]. Recognizing these challenges, the World Health Organization (WHO) introduced the palliative care (PC) initiative in 1990.
End-of-Life Interventions
1. Palliative Care
It focuses on enhancing the QOL of patients with serious illnesses and short expected time left to live, by managing symptoms through a holistic approach [7, 8]. This approach involves interdisciplinary efforts to assess and alleviate pain, address physical and psychosocial issues, and offer spiritual support. Implementing an effective palliative care strategy is crucial for providing patients with appropriate support and symptom management. Palliative care can offer improved QOL to both patients’ and their family members [9].
2. Hospice offering dignified care
Ensuring dignity for those who are terminally ill, struggling with unbearable symptoms in the final days of their life, at the hospice during this crucial period calls for a profound improvement in the alleviation of physical, psychological, spiritual, and existential suffering. Yet, healthcare professionals may find themselves grappling with the challenge of initiating conversations with patients about their limited time remaining and the inevitability of death. Central to preserving dignity in these final moments is the presence of a compassionate companion, offering solace and support throughout the journey’s end. It is imperative that those facing the end of life receive not only effective pain management but also compassionate assistance in navigating the tumult of anxiety, worry, and physical anguish [10]. Achieving this noble objective requires a harmonious synergy among patients, their devoted families, and empathetic healthcare providers, particularly in the specialized environment of hospice care. While the needs of those in the twilight of life may vary, certain timeless principles underpin what defines “exceptional care” in hospice settings. These encompass not only the alleviation of emotional and physical distress but also the nurturing social support, the unwavering continuity of care, and the gentle reassurance that effective communication with both physicians and nurses brings. Indeed, the measure of success in hospice care often lies in the profound satisfaction experienced by those who receive it [11].
Aims and Objectives
To evaluate the impact of palliative care on symptom relief, pain relief, and quality of life.
Secondary objectives
1. Examine the demographics of patients presenting to the GPH.
2. Enumerate the clinical characteristics of the patients presenting to the GPH.
Materials and Methods
• Study Design – Prospective Cohort Study
• Location – Ganga Prem Hospice (GPH)
• Time Period – January 1st 2022 to January 1st 2023
Data Collection
Data of all patients admitted to the hospice between 2022 – 2023 was collected propectively. Data collected included the demographic details (age, gender), clinical characteristics at presentation (site of cancer, stage at presentation, any prior treatment), level of pain relief, symptom relief status, quality of life, vital parameters, cause of death and place of death.
Assessment of pain levels was done pre and post GPH admission according to the VAS Pain Scale and was categorized into no pain, mild pain, moderate pain and very severe pain. Symptom relief was measured before and after GPH admission and was categorized to yes or no. Similarly assessment of quality of life was done before and after GPH admissions and was categorized to poor or good.
Statistical Analysis
Descriptive statistics were used to summarize the demographic and clinical characteristics. Frequencies and percentages were used to present categorical variables. Comparative analysis was used to assess the change pre and post admission to GPH in pain level, symptom relief and quality of life.
Ethical Considerations
All ethical considerations were adhered to during the course of the study. The anonymity and confidentiality of the patient was maintained during the study.
Financial Considerations
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors.
Results
Demographic and Clinical Details
Table 1 shows demographic and clinical details of 99 terminally ill cancer patients admitted at GPH Hospice during 2022-23.
| Demographic Details: | |||
| Age | Minimum: 18 | Median Age: 49 | |
| Maximum: 92 | |||
| Gender | Male: 58 (58.58%) | ||
| Female: 41 (41.41%) | |||
| Clinical Details: | |||
| Site of Cancer | Gastrointestinal: 24 (24.24%) | ||
| Gynecological: 21 (21.21%) | |||
| HNC: 34 (34.34%) | |||
| Respiratory: 11 (11.11%) | |||
| Urological: 9 (9.09%) | |||
| Stage | Stage III: 3 (3.03%) | ||
| Stage IV: 96 (96.96%) | |||
| Prior Treatment | Taken: 70 (71%) | ||
| Not Taken: 29 (29%) | |||
| Reasons for Treatment not taken | Old Age: 2 (6.89%) | ||
| Advanced Stage and fear: 13 (44.82%) | |||
| Financial issues: 14 (48.27%) |
The age distribution ranged from (18 to 92) years, with a median age of 49 years. Gender composition showed a balanced representation, with (58.58%) male and (41.41%) female patients. Cancer site distribution revealed that head and neck (34.34%), gastrointestinal (24.24%), and gynecological (21.21%) cancers were the most prevalent, while respiratory (11.11%) and urological (9.09%) cancers were less common. The overwhelming majority of patients were diagnosed at Stage IV (96.96%), indicative of the advanced disease stage. Of the patients, 70% had received prior treatment, whereas 29% did not, citing reasons such as advanced stage and fear (44.82%), financial constraints (48.27%), and old age (6.89%).
Palliative Care Interventions
Analysis of pain management using the VAS Pain Scale as shown in Table 2, indicated a significant improvement post-GPH admission.
| VAS Pain Scale | Level of Pain | Before GPH Admission | Post GPH Admission |
| No. of Patients (%) | No. of Patients (%) | ||
| 0 | No Pain | 4 (4) | 23 (23) |
| 1-3 | Mild Pain | 60 (61) | 70 (71) |
| 4-7 | Moderate Pain | 34 (34) | 6 (6) |
| 7-10 | Very Severe | 1 (1) | 0 (0) |
Notably, the proportion of patients reporting no pain increased from 4 before admission to 23 post-admission, alongside a reduction in moderate to severe pain levels. Symptom relief status, as shown in Table 3 exhibited marked enhancement post-admission, with 86% of patients experiencing relief compared to 14% before admission.
| Symptom Relief Status | Before GPH Admission | Post GPH Admission |
| No. of Patients (%) | No. of Patients (%) | |
| Yes | 10 (10) | 85 (86) |
| No | 89 (90) | 14 (14) |
Similarly, assessments of quality of life post-GPH admission showed improvement, with 86% of patients reporting good quality of life, contrasting with 22% prior to admission as shown in Table 4.
| Quality of Life | Before GPH Admission | Post GPH Admission |
| No. of Patients (%) | No. of Patients (%) | |
| Poor | 77 (78) | 14 (14) |
| Good | 22 (22) | 85 (86) |
Vital Status and Death Analysis
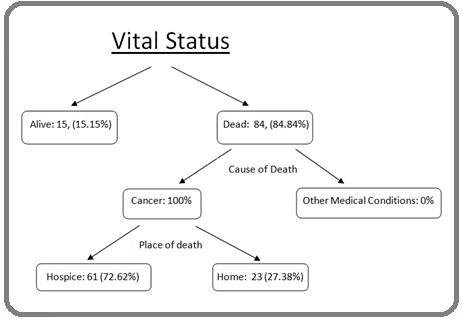
Among the patient cohort, 84.8 % were deceased, with cancer as the primary cause of death. The hospice setting served as the preferred place of passing for the majority of patients (72.62%), while 27.38% passed away at home as shown in Figure 1.
Figure 1. Vital Status of Patients Admitted at GPH.
These findings underscore the pivotal role of hospice care in providing comprehensive end-of- life support to terminally ill cancer patients, emphasizing the significance of patient-centered care in the terminal stage.
Discussion
Cancer remains a significant health challenge with projections estimating that there will be 16.3 million individuals living with the disease by 2040 with a large proportion of these living in low income countries [1]. As most of these patients are diagnosed in late stages palliative care becomes an essential part of their treatment. Palliative care consists of a holistic approach to enhance the quality of life of the patients diagnosed with serious illnesses with short life expectancy [2].
These patients who are struggling with unbearable symptoms in the final days of life require alleviation of physical, psychological, spiritual and existential suffering. It is important that along with symptom relief these patients also receive compassionate assistance in handling anxiety, worry and physical anguish. These form the bedrock of hospice care.
Through this study we aim to present our experience providing hospice care at the Ganga Prem Hospice (GPH) between July 2022 – June 2023 and its role in providing pain relief, symptom relief and quality of life improvements to our terminally ill cancer patients. It was a prospective study consisting of all the patients admitted to the Ganga Prem Hospice, Raiwala, Uttarakhand, India between 2022 and 2023. Patient data included demographic details, clinical characteristics, pain relief status, symptom relief status, quality of life improvement, cause of death and place of death.
There were 99 patients in the study aged between 18 to 92 years with a median age being 49 years. Majority of the patients were male (58.6%) with females making up only 41.4% of the patient group. This difference could just be a marker of increased incidence of malignancy in males as compared to females. There have also been differences noted in the preference for palliative care between males and females. In the analysis of the data from the VOICE clinical trial it was noted that females preferred palliative care more than the males. It has also been noted that males were more likely to adopt to aggressive care in advanced stages as compared to females who are more likely to adopt to hospice/palliative care [3].
Head and neck (34.3%), Gastrointestinal (24.2%) and Gynaecological Malignancies (21.25) were the most common malignancies noted in our study. Other studies from India reported similar results with Head and Neck malignancies being the most common in India [4-8]. Studies from higher income countries like Brazil [9-12] China [13-15] and South Korea [16] had higher incidence of lung, GI, breast and gynaecological malignancies. Reasons for seeking admission for hospice care could be increased requirement for specialized care in head and neck cancer in advanced stages. Advanced head and neck malignancies present with fungating wounds, severe pain and with various tubes in situ like RT and PEG tubes that are difficult to manage at home and hence such patients seek care in hospice. Similarly advanced abdominal malignancies presenting with multiple drains, feeding tubes and with severe symptoms like recurrent vomiting, pain, obstruction and surgical wounds can be difficult to manage at home.
Almost all of the patients in our study (97%) were stage IV patients with 30% of them being treatment naive. The reasons for not seeking treatment were varied with the most common ones being fear of treatment, advanced stage (44.8%) and financial constraint (48.2%). Khankeh et al [17] in his study similarly observed that fear of treatment due to its complications and past experiences of a loved one dying from cancer were the major reasons for refusing treatment in cancer patients. Oshiro et al [18], in his study of factors involved in seeking help in cancer patients identified that age, low educational level, difficult financial conditions, symptom appraisal, lack of knowledge and fear of treatment were the most important factors in delaying cancer care. The other important reason for delay in treatment in a country like India with lack of affordable oncological care is the use of Complementary and Alternative medicine (CAM) in initial stages of cancer. In a study by Pandey et al [19], it was noted that out of 2614 patients who were getting treated for malignancy in a tertiary care centre in Uttarakhand almost 46.2% were reported to have been treated with CAM out of which 85% patients used CAM as the sole modality of treatment. In another study by Kumar et al [20], 38.7% patients out of 1117 patients were found to be CAM users majority belonging to low socio-economic status.
Studies have been conducted to identify patient priorities at the end of life. In an important study by Steinhauser et al [21], the most important priorities were excellent pain and symptom control, being able to spend quality time with family and to deal with unfinished businesses. It has also been noted that good hospice care is better at providing analgesia to patients as compared to those who do not have access to hospice. Similar results were noted in our study where symptom relief status and quality of life pre and post admission to the GPH were markedly better. Patients suffering no pain increased from 4% to 23.2% and patients experiencing symptom relief increased from 14% to 86% after their treatment at GPH. Eighty-six percent patients reported a good quality of life after receiving care at the GPH as compared to 22% prior to their admission. Other factors that have been identified with better quality of life in terminal phase are female gender, sociodemographic factors like (level of education, presence of children, presence of a partner) and type of treatment received in the terminal stages [22]. A cohort study in India showed that in inoperable head and neck carcinoma short course palliative radiotherapy was better than conventional radiotherapy in improving social well-being [6]. A study conducted in Brazil also showed that palliative chemotherapy improved QOL in terminal phases [9].
According to Butow et al [23] and Munday et al [24] deciding the place of death in the terminal hours is influenced by many factors. In our study 84.8% of the patients died due to cancer with majority of them choosing to die at GPH (72.6%). This number is in contrast with other studies from the high income countries where the patients preferred home as the place of death [25, 26]. The systematic study published by Bell et al [27], also showed that home is the preferred place of death for most patients. The above could be explained as we cater to the low socio-economic strata which have difficulty managing advanced terminally ill patients at home. The facilities provided to them at the hospice includes free nursing care, lodging, free food for one of the family members which makes hospice as a preferred place to choose for the end. Also, most of patients in the terminal stage have bed sores, open wounds, multiple tubes in form of Ryles tubes, FJ tubes, PEG tubes and abdominal drains which are difficult to manage at home. Factors such as lack of home-based hospice care facilities and sociological factors which consider dying at home as unacceptable could also be the reasons for the disparity.
These terminally ill patients are difficult to manage at home. Moreover, nuclear families, socioeconomic factors, life in difficult geographic terrain makes it difficult to take care of these patients at home. Ganga Prem hospice provides all palliative care services at no cost including food and stay facility for one attendant. Patients in their terminal phase prefer staying at the GPH to improve quality of life and relief for caregivers.
In conclusion, the palliative care model implemented at Ganga Prem Hospice plays a transformative role in enhancing the quality of life for terminally ill cancer patients by providing effective pain management, symptom relief, and compassionate support. The marked improvements in QOL, alongside the preference for hospice as a place of passing, underscore the value of structured end-of-life care in alleviating both physical and emotional suffering.
This study emphasizes the need for expanded access to hospice services, particularly in low-resource settings where home-based care may not be feasible. With its holistic and patient-centered approach, GPH demonstrates a viable model for end-of-life care that not only supports patients but also alleviates the care giving burden on families. Future research should explore ways to integrate palliative care into national healthcare frameworks to ensure equitable access to dignified, compassionate care for all terminally ill patients.
Acknowledgments
Statement of Transparency and Principals
• Author declares no conflict of interest
• Study was approved by Research Ethic Committee of author affiliated Institute.
• Study’s data is available upon a reasonable request.
• All authors have contributed to implementation of this research.
Disclosure
The authors report no conflicts of interest in this work.
References
- It Is Time to Close the Gap in Cancer Care Dunn J. JCO global oncology.2023;9. CrossRef
- Palliative care [Internet]. [cited 2024 Oct 24]. Available from: https://www.who.int/news-room/fact-sheets/detail/palliative-care .
- Values and options in cancer care (VOICE): study design and rationale for a patient-centered communication and decision-making intervention for physicians, patients with advanced cancer, and their caregivers Hoerger M, Epstein RM , Winters PC , Fiscella K, Duberstein PR , Gramling R, et al . BMC cancer.2013;13. CrossRef
- Fatigue and Quality of Life Outcomes of Palliative Care Consultation: A Prospective, Observational Study in a Tertiary Cancer Center Ghoshal A, Salins N, Deodhar J, Damani A, Muckaden MA . Indian Journal of Palliative Care.2016;22(4). CrossRef
- Symptom Burden and Quality of Life in Advanced Head and Neck Cancer Patients: AIIMS Study of 100 Patients Gandhi AK , Roy S, Thakar A, Sharma A, Mohanti BK . Indian Journal of Palliative Care.2014;20(3). CrossRef
- Hypofractionated Palliative Radiotherapy in Locally Advanced Inoperable Head and Neck Cancer: CMC Vellore Experience Das S, Thomas S, Pal SK , Isiah R, John S. Indian Journal of Palliative Care.2013;19(2). CrossRef
- Symptom Interference and Relation between the Domains of Quality of Life among Cancer Patients of Tertiary Care Hospital Nayak MG , George A, Shashidhara Y. N., Nayak BS . Indian Journal of Palliative Care.2019;25(4). CrossRef
- Spirituality, distress, depression, anxiety, and quality of life in patients with advanced cancer Kandasamy A., Chaturvedi S. K., Desai G.. Indian Journal of Cancer.2011;48(1). CrossRef
- Assessment of quality of life in patients with advanced non-small cell lung carcinoma treated with a combination of carboplatin and paclitaxel Avelino CUR , Cardoso RM , Aguiar SS , Silva MJS . Jornal Brasileiro De Pneumologia: Publicacao Oficial Da Sociedade Brasileira De Pneumologia E Tisilogia.2015;41(2). CrossRef
- The feasibility and benefit of a brief psychosocial intervention in addition to early palliative care in patients with advanced cancer to reduce depressive symptoms: a pilot randomized controlled clinical trial Carmo TM , Paiva BSR , Oliveira CZ , Nascimento MSDA , Paiva CE . BMC cancer.2017;17(1). CrossRef
- Quality of life in responders after palliative radiation therapy for painful bone metastases using EORTC QLQ-C30 and EORTC QLQ-BM22: results of a Brazilian cohort Mendez LC , Raman S, Wan BA , Silva JLP , Moraes FY , Lima KMLB , Silva MF , et al . Annals of Palliative Medicine.2017;6(Suppl 1). CrossRef
- Effectiveness of a palliative care outpatient programme in improving cancer-related symptoms among ambulatory Brazilian patients Paiva C. E., Faria C. B., Nascimento M. S. D. A., Dos Santos R., Scapulatempo H. H. L. R. C., Costa E., Paiva B. S. R.. European Journal of Cancer Care.2012;21(1). CrossRef
- Factors associated with lower quality of life among patients receiving palliative care Chui YY , Kuan HY , Fu ICY , Liu RKY , Sham MK , Lau KS . Journal of Advanced Nursing.2009;65(9). CrossRef
- Quality of life in patients with advanced cancer at the end of life as measured by the McGill quality of life questionnaire: a survey in China Cui J, Fang F, Shen F, Song L, Zhou L, Ma X, Zhao J. Journal of Pain and Symptom Management.2014;48(5). CrossRef
- Quality of life in Chinese home-based advanced cancer patients: does awareness of cancer diagnosis matter? Fan X, Huang H, Luo Q, Zhou J, Tan G, Yong N. Journal of Palliative Medicine.2011;14(10). CrossRef
- Clinical implication of bile spillage in patients undergoing laparoscopic cholecystectomy for gallbladder cancer Lee J, Kim B, Kim W, Wang H, Kim MW . The American Surgeon.2011;77(6). CrossRef
- How do cancer patients refuse treatment? A grounded theory study Khankeh HR , Vojdani R, Saber M, Imanieh M. BMC palliative care.2023;22(1). CrossRef
- Factors related to help-seeking for cancer medical care among people living in rural areas: a scoping review Oshiro M, Kamizato M, Jahana S. BMC health services research.2022;22(1). CrossRef
- Use of complementary and alternative medicine among patients with cancer in a sub-Himalayan state in India: An exploratory study Pandey L, Pasricha R, Joseph D, Ahuja R, Yanthan Y, Garg PK , Gupta M. Journal of Ayurveda and Integrative Medicine.2021;12(1). CrossRef
- Complementary and alternative medicine use among the cancer patients in Northern India Kumar D, Goel NK , Pandey AK , Sarpal SS . South Asian Journal of Cancer.2016;5(1). CrossRef
- Factors considered important at the end of life by patients, family, physicians, and other care providers Steinhauser K. E., Christakis N. A., Clipp E. C., McNeilly M., McIntyre L., Tulsky J. A.. JAMA.2000;284(19). CrossRef
- Quality of life of cancer patients at palliative care units in developing countries: systematic review of the published literature Gayatri D, Efremov L, Kantelhardt EJ , Mikolajczyk R. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation.2021;30(2). CrossRef
- The dynamics of change: cancer patients' preferences for information, involvement and support Butow P. N., Maclean M., Dunn S. M., Tattersall M. H., Boyer M. J.. Annals of Oncology: Official Journal of the European Society for Medical Oncology.1997;8(9). CrossRef
- Exploring preferences for place of death with terminally ill patients: qualitative study of experiences of general practitioners and community nurses in England Munday D, Petrova M, Dale J. BMJ (Clinical research ed.).2009;339. CrossRef
- Determinants of preference for home death among terminally ill patients with cancer in Taiwan: a cross-sectional survey study Chen CH , Lin Y, Liu L, Tang ST . The journal of nursing research: JNR.2014;22(1). CrossRef
- Predictors of dying at home for patients receiving nursing services in Japan: A retrospective study comparing cancer and non-cancer deaths Ikezaki S, Ikegami N. BMC palliative care.2011;10. CrossRef
- Factors associated with congruence between preferred and actual place of death Bell CL , Somogyi-Zalud E, Masaki KH . Journal of Pain and Symptom Management.2010;39(3). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Nursing , 2025
Author Details
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times