Evaluation of the Impact of Timeliness of Care on Patient Experience in Suspected Lung Cancer: A Mixed-methods Study
Download
Abstract
Background: Lung cancer has the highest burden of cancer in Australia and delays in healthcare can significantly worsen outcomes and cause psychological harm. Australian Optimal Care guidelines recommend a 14-day interval between primary care referral and an appointment with a specialist, however, many healthcare providers are not currently meeting this target. The aim of this pilot study was to assess the patient experience during the interval between referral from primary care to being seen in tertiary care.
Methods: We recruited patients with suspected lung cancer referred to a tertiary respiratory clinic. A questionnaire was conducted including Likert-style questions to understand patient perspectives of timeliness, coordination, and communication regarding the early stages of lung cancer care. Additional open-ended questions were included to expand the understanding of patients’ perspectives.
Results: The questionnaire was completed by 37 of 52 eligible participants (71%), the median age of participants was 69 years old (IQR 15.5-33.5) and the most common diagnosis was lung adenocarcinoma. Overall, patients reported a positive perception of timeliness of care, despite wait time of median 25 (IQR 15.5-33.5) days. Just one participant stated they were aware of a timeliness clinical guideline. The most common stressors reported by patients were ‘fear of the unknown’ and ‘waiting.’
Conclusions: There appears a paradox in perception of expected wait time within the healthcare system and reported concerns by individuals with suspected lung cancer. Awareness of timeliness guidelines is poor. There is scope for interventions such as improved information resources and access to earlier telehealth appointments to impact on patient reported satisfaction.
Introduction
Lung cancer has the highest burden of any cancer in Australia [1]. Although the five-year survival rate for lung cancer is improving, it remains low at 24% [2]. The introduction of the Australian National Lung Cancer Screening Program in July 2025 will likely place additional demands on existing healthcare services that are already under pressure [1, 3].
The Australian Optimal Care Pathway recommends that patients referred from primary care should see a lung cancer specialist within 14 days [4, 5]. This two-week period was initially proposed by the British Thoracic Society in 1998 and has been adopted in multiple international guidelines [6]. While existing literature recognises the importance of timely care in the effective treatment of lung cancer, there is limited research specifically evaluating the efficacy of the 14-day interval [7-9].
Further, delays in receipt of treatment can result in cancer stage progression [10]. However, the evidence for timely care such as the 14-day target benefiting lung cancer survival is inconclusive. Studies have linked timely diagnosis with positive patient experience, and conversely, delayed diagnosis and treatment have been linked to increased patient stress [11, 12]. This pilot study aimed to address the gap in research by exploring patients’ perceptions of timeliness in the early stages of lung cancer care.
Methods
Design
This feasibility study employed a mixed-methods survey design, using a quantitative questionnaire with Likert-style questions and qualitative open-ended questions.
Population
The study population included patients referred to the Sir Charles Gairdner Hospital (SCGH) lung cancer clinic in Western Australia with a clinical suspicion of lung cancer. The clinic receives approximately 300-350 new cases annually from both metropolitan and rural areas. Data was collected from 23 July to 17 September 2024. ‘Rural’ was defined by being under the catchment of the Western Australian Country Health Service.
Questionnaire Development
A questionnaire was designed around three key themes: timeliness, communication, and coordination. Questions were designed to be simple and easy to understand, with positive and negative statements alternated to reduce bias. The questionnaire consisted of 11 possible questions using a 5-point Likert scale. Additional background questions were included to enable branching logic within the questionnaire. Two open-ended questions were included to gather further insights into patients’ awareness of guidelines and their most stressful experiences during the waiting period. A complete copy of the questionnaire is available in the online supplement.
Participant Recruitment
Participants were identified based on referral reasons and then approached for participation prior to their specialist appointment.
Inclusion criteria:
- Patients referred to the SCGH lung cancer service with clinical suspicion of lung cancer.
- Patients attending their first face-to-face appointment.
- Able to complete the questionnaire.
- Aged >18 years old.
Exclusion criteria:
- Patients already under follow-up with the respiratory service
- Patients who were not fit for participation due to advanced disease, poor cognition, or concerns about capacity to participate.
- Patients suspected to have metastatic disease that has spread to the lungs (i.e. not primary lung cancer).
Questionnaire Delivery
The questionnaire was administered using a tablet with Microsoft Forms (Microsoft Corp, USA), with investigators reading the questions aloud to patients and recording their verbal responses. All participants elected to have the questions read to them.
Data Collection
In addition to the questionnaire, patient notes were used to collect data on postcode, smoking status, referral date, first contact date, first contact type (telehealth, face to face), multidisciplinary team discussion date, final diagnosis, and diagnosis date.
Statistical Analyses
Statistical analysis was performed using SPSS software (IBM Corp ver 30.0). Demographics and questionnaire data were summarised using descriptive statistics. Student’s t-tests were used to explore the effect of patient factors on scores. Ordinal regression analysis was used to investigate the relationship between wait times and Likert scores. Spearman’s correlation was used to analyse correlations between Likert scale items.
Ethics Approval
A waiver of formal ethical approval was obtained through the North Metro Health Service Governance Evidence Knowledge Outcomes approval process (Ref 54304), as this was considered a clinical care quality improvement project.
Results
Of the 52 eligible participants, 37 completed the questionnaire, the remainder were not included due to time constraints or declining participation. The median age was 69.3 years (interquartile range (IQR) 64.8-81.0), with 21 (57%) participants being male. There were 10 (27%) participants from rural locations, 14 (37.8%) were current smokers at the time of their appointment and 19 (51.4%) were former smokers, see Table 1.
| n= | Percentage | |
| Age group | ||
| ≤55 | 3 | 8.10 |
| 56-65 | 10 | 27.00 |
| 66-75 | 9 | 24.30 |
| 76-85 | 13 | 35.10 |
| 86-95 | 2 | 5.40 |
| Sex | ||
| Male | 21 | 56.80 |
| Female | 16 | 43.20 |
| Rurality | ||
| Metropolitan | 27 | 73.00 |
| Rural | 10 | 27.00 |
| Smoking status | ||
| Current smoker | 14 | 37.80 |
| Former smoker | 19 | 51.40 |
| Never smoker | 4 | 10.80 |
The most common eventual diagnosis was non-small cell lung cancer (n=19, 51.3%), with lung adenocarcinoma being the most frequent subtype (n=16, 43.2%). 12 (32.4%) participants had a benign diagnosis with 4 (10.8%) inconclusive at the time of censure.
Wait Times
The shortest wait time between referral and the first face-to-face appointment was 11 days with a median wait time of 25 days (IQR 15.5-33.5). Only three patients were seen within the 14-day timeframe recommended by the Australian OCP guidelines. Rural participants waited 17.8 days longer than metropolitan participants, with a median wait time of 34.5 days (IQR 19.2-58.2) compared to 22.0 days (IQR 15.0-29.0) for metropolitan (p = 0.29). The specialist lung cancer nurse had contacted eight patients by telephone appointment prior to their face-to-face appointment, six of whom were rural patients.
Questionnaire Responses
Concern over chest x-ray or CT or ‘lung nodule’ was the most common explanation given by participants for their appointments. Only one participant was aware of guidelines for timeframes and they reported having previously worked in healthcare.
Table 2 and Figure 1 summarises the responses and scores.
| Question | Indicator | Theme | Median (IQR) |
| My phone or telehealth appointment was long enough to process the information I was given. | Positive | Timeliness | 4 (2.0-5.0) |
| I felt like my doctor or nurse didn't listen to me when I asked questions. | Negative | Communication | 3 (3.0-5.0) |
| The doctor explained what to expect once I have been referred to the hospital. | Positive | Communication | 2 (1.0-4.0) |
| I waited too long to see the lung specialist. | Negative | Timeliness | 1.0 (1.0-2.5) |
| I understand the roles of the healthcare professionals taking care of me. | Positive | Coordination | 4 (2.0-5.0) |
| I feel my care has been well coordinated. | Positive | Coordination | 4 (3.8-5.0) |
Figure 1. Breakdown of Questionnaire Responses .
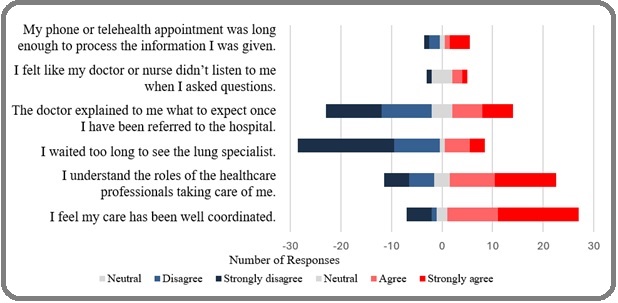
The most negative score was for the item ‘I waited too long to see the lung specialist,’ with a median score of 1 (IQR 1.0-2.5), indicating patients generally felt they were seen in a timely manner. The communication items received more negative-neutral scores, particularly the item ‘I felt like my doctor or nurse didn’t listen to me when I asked questions’ (median 3.0, IQR 1.5-3.0), reflecting the healthcare interactions prior to the current appointment. Coordination items generally received positive scores, with the item ‘I feel my care has been well coordinated’ having a median score of 4 (3.8-5.0).
Perception of Timeliness
Ordinal regression analysis found that wait time perception only slightly decreased with increased wait time. Each week had an associated increase in odds for patients feeling they waited too long (‘wait time score’), with an odds ratio of 0.83 (95% CI, 0.69 to 1.00), which was statistically significant, χ2(1) = 4.02, p=0.045. Figure 2 demonstrates the downward trend of wait time scores as wait time increases.
Figure 2. Trend of Participant Reported wait Time Scores Based on Days Participants Waited between Referral and First in-person Appointment. A lower wait time score indicates a lower satisfaction; p=0.045 for trend.
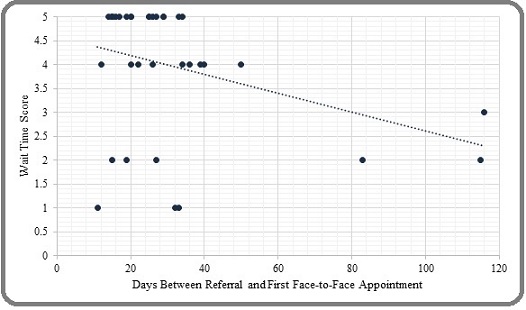
Neither rurality, nor prior telehealth contact were found to have a significant impact on perception of timeliness, for instance the median wait time score for rural was 4.00 (IQR 3.5-5.0) and metropolitan 5.0 (IQR 3.0-5.0); p=0.71. Similarly, the scores were similar for participants who attended a telehealth appointment prior to their face-to- face appointment (5.0, IQR 3.0-5.0) versus patients who had no prior appointment (4.0, IQR 3.25-5.0); p=0.69). In this case, the similarity between telehealth and rural results can be explained by the fact that most patients who had a prior telehealth appointment were rural patients.
Open-Ended Responses
The most common response to the open-ended questions was ‘not stressed’ (12/33, 32%). The next most common concerns related to ‘waiting’ (5/33), ‘fear of the unknown’ (3/33), and not knowing the diagnosis (3/33). Participants who reported stress related to waiting were generally concerned about waiting for results. Those who had to travel long distances were stressed about travel times, costs, and organising multiple appointments.
Discussion
O the author’s knowledge, this is the first study to examine attitudes and experiences of individuals with suspected lung cancer regarding the 14-day wait time in Australia. Despite most participants waiting longer than the recommended 14-day interval, they generally reported a positive experience of timeliness of care. However, paradoxically, participants also indicated that their greatest causes of stress were ‘wait times’ and ‘fear of the unknown’, and there was poor knowledge of the OCP timeliness guidelines.
It is well established that patients are likely to experience heightened stress with long wait times [13, 14]. However, this study suggests that patients appear generally satisfied with wait times that surpass the 14-day guideline. In the absence of a clear oncological driver for the 14-day interval, patient perspectives should be considered to justify the timeline target. Participants’ apparent satisfaction with wait times may be influenced by an expectation of long wait times within the public healthcare system and that participants in this study were largely unaware of the existing guidelines. Patients reserve a level of compassion for healthcare workers ‘doing their best’ in a complex system and are overall very understanding of delays. Improved knowledge of the 14-day target may impact perceived satisfaction with healthcare services.
Wait time specifically was not as great a reported concern as the waiting process itself, such as waiting for results and not knowing what to expect. Fear of the unknown has previosuly been identified as a stressor for patients [15]. Responses from participants in our study highlighted a some areas where providing imporved clarity may be helpful, such as information on what to expect in the diagnostic process, why they’re attending the lung cancer clinic and knowing how long they should expect to wait for tests. Improved communication regarding these and other concerns may reduce patient and family stress and ease them into the diagnositc journey process. Poor care coordination is associated with delays in patient care [7, 12, 16]. Our study suggests that there may be a role for improved resources dedicated to patients and/ or general practitioners to guide them on what to expect after referral to tertiary services. Simple information, such as leaflets or digital resources, could clarify questions and reduce uncertainties. During the study period, patient orientated information about the clinic was available on a departmental website, however, patients and families were not specifically directed to this resource.
This pilot study has limitations, including a small sample size and the population being from a single tertiary clinic. This limits the statistical analysis and generalisability to the broader Australian population. The study population is also potentially biased towards patients in earlier stages of lung cancer, with more advanced or symptomatic patients potentially fast tracked through investigations, perhaps as an inpatient. The use of a 5-point Likert scale introduces the possibility of central tendency bias, acquiescence bias, and social desirability bias. However, the questionnaire functioned well and the study used open-ended questions to gather additional information that could not be captured from the questions alone. The oral delivery of the questionnaire allowed for a better understanding of patients’ mindsets and enabled patients with lower literacy to participate. Participants sometimes reported ‘phone appointments’ when they had not had a telehealth appointment, these were possibly administrative calls from the clinic.
Future research could examine the impact of improved awareness about the 14-day guideline and improved provision of patient-orientated information about the clinic and diagnostic journey, on perceived satisfaction and concerns. The impact of different models of care, such as up-front more formalised telehealth appointments with specialist nurses could also be evaluated.
In conclusion, participants being investigated for possible lung cancer generally reported a positive experience of timeliness of care, despite the fact that the majority waited longer than the current 14-day guidelines. Awareness of the timeliness guidelines was poor. Paradoxically, the study also highlighted considerable stressors, including fears of the unknown and waiting, indicating that communication and psychosocial support could be improved.
Acknowledgments
Statement of Transparency and Principals
• Author declares no conflict of interest
• Study was approved by Research Ethic Committee of author affiliated Institute.
• Study’s data is available upon a reasonable request.
• All authors have contributed to implementation of this research.
References
- Burden of cancer in Australia. Canberra: Australian Institute of Health and Welfare AIHW . 2017. (https://www.aihw.gov.au/getmedia/a1aec7bd-ddb7-416f-9a7e-f2133cd5d4cb/20965.pdf.aspx?inline=true)..
- Cancer Australia. Lung Cancer Statistics. Cancer Australia. (https://lung-cancer.canceraustralia.gov.au/statistics) .
- The TSANZ and Lung Foundation Australia 2023 landscape survey of lung cancer care across Australia and Aotearoa New Zealand Nash J, Leong T, Dawkins P, et al . Respirology.2024;29(5):405-412. CrossRef
- Optimal Care Pathway for people with lung cancer. 2nd ed: Cancer Council Victoria 2021 Melbourne, Victoria . https://www.cancer.org.au/assets/pdf/lung-cancer-optimal-cancer-care-pathway.
- Lung cancer (internet-based) Delphi (LUCiD): A modified eDelphi consensus process to establish Australasian clinical quality indicators for thoracic cancer Nash J, Stone E, Vinod S, Leong T, Dawkins P, Stirling RG , Harden S, et al . Respirology (Carlton, Vic.).2024;29(12). CrossRef
- BTS recommendations to respiratory physicians for organising the care of patients with lung cancer. The Lung Cancer Working Party of the British Thoracic Society Standards of Care Committee Thorax.1998;53 Suppl 1(Suppl 1). CrossRef
- Limitations and perceived delays for diagnosis and staging of lung cancer in Portugal: A nationwide survey analysis Barata F, Fidalgo P, Figueiredo S, Tonin FS , Duarte-Ramos F. PloS One.2021;16(6). CrossRef
- Effects of treatment delays on lung cancer survival. Guzman P, Segura S, Halpern MT . JCO Oncology Practice.2023;19(11_suppl). CrossRef
- Does timeliness of care in Non-Small Cell Lung Cancer impact on survival? Vinod SK , Chandra A, Berthelsen A, Descallar J. Lung Cancer (Amsterdam, Netherlands).2017;112. CrossRef
- Rapid disease progression with delay in treatment of non-small-cell lung cancer Mohammed N, Kestin LL , Grills IS , Battu M, Fitch DL , Wong CO , Margolis JH , et al . International Journal of Radiation Oncology, Biology, Physics.2011;79(2). CrossRef
- Patient and Health Care Professional Perspectives: A Case Study of the Lung Cancer Integrated Care Pathway Bravi F, Ruscio ED , Frassoldati A, Cavallesco GN , Valpiani G, Ferrozzi A, Wienand U, Carradori T. International Journal of Integrated Care.2018;18(4). CrossRef
- Patient and carer perceived barriers to early presentation and diagnosis of lung cancer: a systematic review Cassim S, Chepulis L, Keenan R, Kidd J, Firth M, Lawrenson R. BMC cancer.2019;19(1). CrossRef
- Use of clinical quality indicators to improve lung cancer care in a regional/rural network of health services Kim ML , Matheson L, Garrard B, Francis M, Broad A, Malone J, Eastman P, Rogers M, Yap C. The Australian Journal of Rural Health.2019;27(2). CrossRef
- Delays in diagnosis and treatment of lung cancer: Lessons from US healthcare settings Koo M. M., Zhou Y., Lyratzopoulos G.. Cancer Epidemiology.2015;39(6). CrossRef
- It is important that the process goes quickly, isn't it?" A qualitative multi-country study of colorectal or lung cancer patients' narratives of the timeliness of diagnosis and quality of care Malmström M, Rasmussen BH , Bernhardson BM , Hajdarevic S, Eriksson LE , Andersen RS , MacArtney JL . European Journal of Oncology Nursing: The Official Journal of European Oncology Nursing Society.2018;34. CrossRef
- Factors influencing the delivery of cancer pathways: a summary of the literature Brice SN , Harper P, Crosby T, Gartner D, Arruda E, England T, Aspland E, Foley K. Journal of Health Organization and Management.2021;35(9). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Nursing , 2025
Author Details
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times
- Supplementary file downloaded - 0 times