Knowledge, Attitude and Awareness of HPV Vaccination among College-Going Girls (18–26 years) in Delhi NCR
Download
Abstract
Objective: This study aimed to evaluate the knowledge, attitude, and awareness (KAA) regarding HPV vaccination among college-going girls aged 18–26 years in Delhi-NCR, focusing on identifying barriers to vaccine uptake and factors influencing vaccination status.
Methods: A cross-sectional survey was conducted between July 2024 and January 2025, involving 506 college students from various institutions in Delhi-NCR. Data were collected using an online structured questionnaire addressing demographics, knowledge of cervical cancer and HPV, awareness of the HPV vaccine, and attitudes toward vaccination. The responses were analyzed using descriptive statistics and chi-squared tests to assess associations between awareness and vaccination status.
Results: Among the respondents, 80.2% correctly identified cervical cancer as a malignancy of the cervix, but 20% mistakenly associated it with other cancers like neck or bone cancer. Only 58.3% accurately recognized HPV as a virus linked to cancer, while a significant proportion confused HPV with HIV/AIDS (37.2%) or considered it a bacterial infection (16.6%). Despite 51% of participants being aware of the HPV vaccine, only 11.9% reported receiving it. Social media emerged as the most common information source (98%). Financial constraints (48%) were identified as the most significant barrier to vaccination, followed by a lack of awareness (40%) and safety concerns (12%). Social stigma also played a role, with many respondents finding it difficult to discuss HPV vaccination with their families.
Conclusion: The findings reveal substantial knowledge gaps and socio-cultural barriers to HPV vaccination among college-going girls in Delhi-NCR. While awareness of cervical cancer was moderate, misconceptions regarding HPV and its vaccine persist. To increase vaccination coverage, it is crucial to implement educational campaigns targeting young women, address misinformation on social media, and advocate for the inclusion of the HPV vaccine in the National Immunization Programme. Reducing financial barriers through policy interventions could further enhance vaccine uptake.
Introduction
Cervical cancer is a preventable but prevalent global health issue, ranking as the fourth most common cancer among women worldwide. According to the World Health Organization (WHO), cervical cancer accounts for approximately 604,127 new cases and 341,831 deaths annually [1]. The disease disproportionately affects low- and middle-income countries (LMICs), where access to screening and vaccination is limited. In India, cervical cancer ranks as the second most common cancer among women after breast cancer, with an estimated 1,27,526 new cases and 79,906 deaths in 2022, contributing to about 25% of the global cervical cancer burden [1].
A Preventable Tragedy: The Role of HPV
The primary cause of cervical cancer is persistent infection with high-risk types of Human Papillomavirus (HPV), particularly types 16 and 18, responsible for approximately 70% of cervical cancer cases worldwide [2]. HPV is a sexually transmitted virus, with most infections being asymptomatic and self-limiting. However, in some cases, the virus persists and progresses to precancerous lesions or invasive cervical cancer. Besides cervical cancer, HPV is also linked to anogenital cancers and oropharyngeal cancers [3].
Vaccination as a Key Preventive Measure
HPV vaccination is one of the most effective primary prevention strategies. The WHO recommends vaccinating girls between the ages of 9 and 14 years, ideally before the onset of sexual activity. The vaccines available in India include Cervavac, Gardasil, targeting different high-risk strains of HPV. Countries like Australia have integrated HPV vaccination into their national immunization programs, achieving over 80% coverage, leading to a 90% reduction in HPV infections among vaccinated cohorts [4].
Barriers to HPV Vaccination in India
In India, several socio-cultural and economic factors hinder HPV vaccine coverage. Vaccines are predominantly available in the private healthcare sector, making them inaccessible for many due to high costs [5]. Additionally, cultural stigma associating HPV vaccination with promiscuity deters acceptance, as families often perceive the vaccine as linked to sexual behavior. Misconceptions persist, as highlighted by previous studies indicating that 45.61% of Indian college girls had no knowledge of HPV, confusing it with HIV/AIDS [6].
Rationale for the Study
College-going girls, particularly those aged 18–26 years, are at a critical stage where vaccination could still be beneficial. However, awareness levels among this group remain low. This study aimed to assess the awareness, knowledge, and attitudes (KAA) regarding the HPV vaccine among college-going girls in Delhi-NCR, a metropolitan region that reflects diverse socio-cultural perspectives. Understanding their perceptions is essential for designing targeted interventions to improve vaccine acceptance.
Materials and Methods
Study Design
A cross-sectional study was conducted from 26 July 2024 to 21 January 2025 to evaluate KAA towards the HPV vaccine among college-going girls aged 18–26 years in Delhi-NCR.
Study Population
The study included 506 students from various colleges across Delhi-NCR. Participants were included based on the following criteria:
• Age between 18–26 years.
• Currently enrolled in a college in Delhi-NCR.
•Willingness to participate and provide informed consent.
Data Collection
Data were collected using an online structured questionnaire that covered:
• Demographics: Age, education, vaccination status.
• Knowledge of Cervical Cancer and HPV: Understanding the disease and its causes.
• Awareness of the HPV Vaccine: Knowledge of vaccine availability and benefits.
• Attitudes Towards Vaccination: Willingness to vaccinate and perceived barriers.
Statistical Analysis
Data were analyzed using IBM SPSS Statistics version
23. Descriptive statistics summarized demographic characteristics and KAA responses. Associations between awareness and vaccination status were assessed using chi-squared tests, with p<0.05 considered statistically significant.
Results
Demographic Characteristics
There were 506 participants, predominantly undergraduate students from Delhi-NCR colleges, with ages ranging from 18–26 years.
Knowledge About
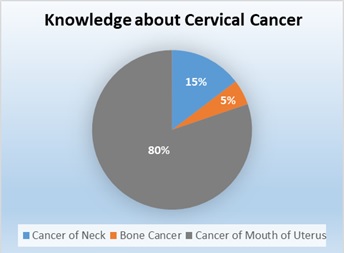
Cervical Cancer 80.2% (406/506) correctly identified cervical cancer as a malignancy affecting the cervix. However, 20% associated it with neck or bone cancer, reflecting a knowledge gap as depicted in Figure 1.
Figure 1. Represents Knowledge about Cervical Cancer. It depicts that 80% (406/506) of the respondents correctly identified cervical cancer.
Knowledge of HPV
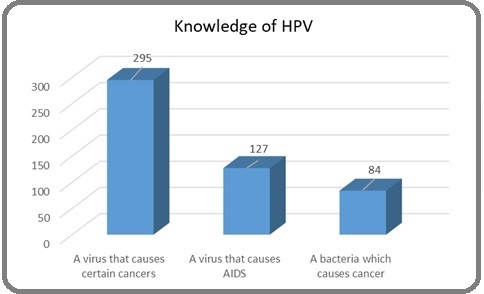
Figure 2 depicts that only 58.3% (295/506) correctly identified HPV as a virus causing cancer. Notably, 188 participants mistakenly associated HPV with HIV/AIDS, while 84 thought it was a bacterial infection.
Figure 2. Represents Knowledge about HPV. It depicts that 58.3% (295/506) correctly identified HPV as a virus causing cancer. Notably, 25% participants mistakenly associated HPV with HIV/AIDS, while 16% thought it was a bacterial infection.
Awareness of HPV Vaccine
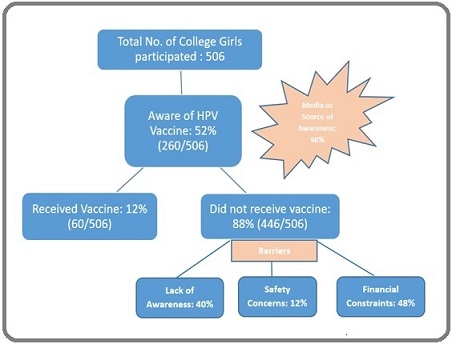
Of the 260 respondents aware of the vaccine, only 52% knew its role in preventing cervical cancer. Social media was the primary source of information (98%).
Vaccination Status
Figure 3 represents that only 11.9% (60/506) had received the HPV vaccine despite 395 expressing trust in its safety. Barriers included lack of awareness (40%), safety concerns (12%), and financial constraints (48%).
Figure 3. Depicts Vaccination Status and Barriers to Vaccination .
Discussion
This study highlights the substantial gaps in awareness, knowledge, and attitudes regarding HPV vaccination among college-going girls in Delhi-NCR. Despite 78.8% of respondents correctly identifying cervical cancer, knowledge about HPV and its vaccine remains significantly limited. Similar findings have been observed in studies across India, where misconceptions about HPV being related to HIV/AIDS persist [6].
Global Context and Lessons
Globally, countries with integrated national immunization programs for HPV vaccines have shown remarkable success. For example, Australia achieved a 90% reduction in HPV infections after implementing a school-based vaccination program, reaching over 80% coverage [4]. In contrast, India lacks a nationwide school-based vaccination strategy, with vaccines being predominantly available in the private sector. Consequently, affordability becomes a significant barrier, as noted by 48% respondents in our study who cited financial issues as a deterrent.
Cultural and Social Challenges
One of the most significant challenges identified is the social stigma associated with HPV vaccination. In conservative societies, where sexual health is rarely discussed openly, vaccines perceived as linked to sexual activity are met with resistance. This was evident as 60% of participants indicated that discussing HPV vaccination within families was difficult. Similar cultural barriers were noted in Thailand, where perceived moral implications hindered vaccine acceptance [7].
Role of Media and Misinformation
Social media played a dual role in the awareness landscape. While 98% of those aware of the HPV vaccine identified social media as their primary information source, the quality and accuracy of information remain questionable. Previous studies have noted that online misinformation can lead to vaccine hesitancy, as seen in Fujian, China, where mass media significantly shaped public attitudes towards HPV vaccination [8].
Financial Barriers and Policy Gaps
Financial affordability remains a crucial barrier, as the HPV vaccines available in India are largely restricted to the private sector. In contrast, countries like Rwanda and Bhutan, where the HPV vaccine is included in national immunization programs, have seen higher uptake and reduced cervical cancer incidence [9]. Incorporating the HPV vaccine into India’s National Immunization Programme (NIP) could substantially reduce the financial burden, making it more accessible to young women.
Addressing Knowledge Gaps
The significant number of respondents who confused HPV with HIV/AIDS (188 out of 506) underscores a critical need for comprehensive health education. Schools and colleges should integrate sexual health topics into the curriculum to clarify the differences between sexually transmitted infections. Previous studies from Amity University have shown that targeted educational interventions can significantly improve knowledge and acceptance rates [6].
Strengths and Limitations
The study’s strength lies in its large sample size and inclusion of diverse college-going populations in Delhi- NCR, providing insights into urban young women’s perceptions. However, the study is limited by its cross- sectional design, which captures data at a single point in time, and the reliance on self-reported data, which may introduce recall bias. Further longitudinal studies are recommended to assess changes in awareness and vaccination rates over time.
In conclusion, the KAA survey among college-going girls highlights critical knowledge gaps and socio-cultural barriers affecting HPV vaccine uptake. Despite moderate awareness of cervical cancer, misconceptions about HPV and its vaccine persist, often conflating it with HIV. Social stigma and financial constraints further hinder vaccine acceptance.
To increase vaccination rates, it is essential to:
• Increase Awareness: Implement targeted educational campaigns in colleges.
• Leverage Media Effectively: Utilize social media responsibly to disseminate accurate information.
• Policy Integration: Advocate for including the HPV vaccine in the National Immunization Programme.
• Financial Support: Provide subsidies to reduce vaccine costs.
• Community Engagement: Involve families in educational initiatives to dispel myths and normalize vaccination.
By addressing these challenges, public health interventions can significantly reduce the burden of cervical cancer and move towards its elimination as a public health problem.
Acknowledgements
Funding Source
This study received no funding.
Scientific Approval
Approval was obtained from the Scientific committee of Rajiv Gandhi Cancer Institute and Research Centre, Rohini.
Ethical Declaration
Approval was obtained from the Institutional Review Board of Rajiv Gandhi Cancer Institute and Research Centre, Rohini. Participation was voluntary, with informed consent obtained online before survey initiation. Anonymity and confidentiality of participant data were strictly maintained.
Authors’ contributions
Indu Aggarwal: Conceptualization, study design, manuscript reviewing and editing.
Diksha Mehta: Manuscript drafting, data analysis, reviewing and editing.
Shashi Rakheja: Manuscript reviewing and editing.
Harmeet Goel: Manuscript reviewing and editing.
Data Availability: Data will be available on request from author.
Study Registration
Not Applicable
References
- Cervical Cancer Statistics. World Health Organization Globocan . 2022.
- Carcinogenic human papillomavirus infection Schiffman M, Doorbar J, Wentzensen N, Sanjosé S, Fakhry C, Monk BJ , Stanley MA , Franceschi S. Nature Reviews. Disease Primers.2016;2. CrossRef
- Beyond cervical cancer: burden of other HPV-related cancers among men and women Chaturvedi AK . The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine.2010;46(4 Suppl). CrossRef
- HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010-2019 Bruni L, Saura-Lázaro A, Montoliu A, Brotons M, Alemany L, Diallo MS , Afsar OZ , et al . Preventive Medicine.2021;144. CrossRef
- Prospects and prejudices of human papillomavirus vaccines in India Das BC , Hussain S, Nasare V, Bharadwaj M. Vaccine.2008;26(22). CrossRef
- HPV and Cervical Cancer Epidemiology - Current Status of HPV Vaccination in India Chatterjee S, Chattopadhyay A, Samanta L, Panigrahi P. Asian Pacific journal of cancer prevention: APJCP.2016;17(8).
- Cultural influences on HPV vaccine uptake in Thailand Wong LP, , Sam IC , Zimet GD . Vaccine.2012;30(2):333-338.
- Media influence on HPV vaccination among young women in China Yang XY , Zhang J, Wang Z. BMC Public Health.2019;19:963.
- Country recommendations on the inclusion of HPV vaccines in national immunization programmes among high-income countries, June 2006-January 2008 Koulova A, Tsui J, Irwin K, Van Damme P, Biellik R, Aguado MT . Vaccine.2008;26(51). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Nursing , 2025
Author Details
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times