Issues and Challenges in Diagnoses of Borderline Ovarian Neoplasms by Frozen Section
Download
Abstract
Introduction: Frozen section is a rapid intraoperative method of tissue sectioning with the help of cryostat to arrive at a diagnosis and guide the operative procedure. It is an important diagnostic tool in the intraoperative management of ovarian neoplasms.
Aims and Objectives: 1) To evaluate clinically suspected ovarian neoplastic lesions by frozen section. 2) To analyze the factors associated with difficulty in diagnoses of borderline ovarian neoplasms.
Materials and Methods: This is a cross-sectional study conducted in the Department of Pathology for a period of 2 years. 60 cases of ovarian neoplasms undergoing Frozen section and subsequent histopathological examination are included in the study.
Results: The mean age of patient is 39.49 years (21-72). Of the 60 cases, 73.33% are benign, 8.33% borderline and 18.3% are malignant on histopathological diagnosis. The concordance rate of frozen section with histopathological diagnosis is 91.67%. The sensitivity, specificity, positive predictive value, negative predictive value and diagnostic accuracy of Frozen section in the diagnosis of Benign, Borderline and Malignant ovarian neoplasms are 95.45%, 92.73%, 97.67%, 88.24% and 88.64%; 100%, 92.16%, 55.56%, 100% and 55.56%; 72.73%, 100%, 100%, 94.23% and 72.73% respectively.
Conclusion: Frozen section of ovarian neoplasms helps to arrive at a diagnosis of whether they are benign or malignant with a high level of accuracy. Diagnosis of a benign lesion in a young patient guides the surgeon to a fertility conserving surgery. Likewise, diagnosis of a malignant lesion on table guides the surgeon to execute an extensive surgery in a single setting, saving the patient of the physical, emotional, psychological and financial strain of a second look operation.
Introduction
Frozen section is a rapid intraoperative method of tissue sectioning with the help of cryostat to arrive at a diagnosis and guide the operative procedure. Ovarian cancer is the seventh most common cancer among women. In 2018, 4.4% of entire cancer-related mortality among women was attributed to ovarian cancer [1]. Although among the gynaecological cancers, ovarian cancer ranks third after cervical and uterine cancer, it has the highest case fatality rate when presenting in advanced stage [2].The highest prevalence of ovarian cancer is seen in non-Hispanic white women (12.0 per 100,000), followed by Hispanic (10.3 per 100,000), non- Hispanic black (9.4 per 100,000), and Asian/Pacific Islander women (9.2 per 100,000) [3]. Ovarian neoplasms can be either benign, borderline or malignant. The World Health Organisation has classified ovarian neoplasms into epithelial/surface tumours, sex cord stromal tumours, germ cell tumours and secondary/metastatic tumours. Quite a few times, the pre-operative diagnostic modalities like tumour markers and radiology are inconclusive and Ultrasound guided fine needle aspiration cytology or biopsy increases risk of tumour implantation; there comes the role of frozen section which guides the operative procedure intraopearatively as the treatment modalities of ovarian neoplasms differ depending on the type of neoplasm, the category of neoplasm and also the age and the fertility preserving needs of the patient. Benign tumors are treated by cystectomy or oophorectomy. Borderline tumors are surgically treated with hysterectomy, bilateral salpingo-oophorectomy, omentectomy, and pelvic and para-aortic lymphadenectomy. A fertility sparing surgery is considered for those who desire to preserve fertility. However, for the management of malignant ovarian neoplasm, a complete surgical procedure involving hysterectomy, bilateral salpingo-oophorectomy, omentectomy, and pelvic and para-aortic lymphadenectomy is usually performed. With this background, we have undertaken this study to achieve the following aims and objectives – 1) To evaluate clinically suspected ovarian neoplastic lesions by frozen section. 2) To analyze the factors associated with difficulty in diagnoses of borderline ovarian neoplasms by Frozen section.
Materials and Methods
This is a hospital based cross-sectional study conducted for a period of 2 years from July, 2020 to June, 2022 in the Department of Pathology of Gauhati Medical College and Hospital, Guwahati. It includes 60 cases of suspected ovarian neoplasms that underwent both frozen section and subsequent histopathological examination. Ethical clearance was taken from the Institutional Ethical Comittee. Prior to the procedure of Frozen section, the Cryostat LEICA CM 1860 UV is switched on and it is ensured that all instruments, fixatives, slides, coverslip, stains are in easy accessibility in the Frozen section procedure room. A thorough work up of each case with detailed history and investigations is done. Fresh tissue is sent in clean container without any fixative or normal saline along with a proper requisition form with patient’s data and clinical details and the indication for Frozen section to the Department of Pathology. The tissue is examined for dimensions, appearance and colour. The specimen is dissected and appropriate sections taken from representative areas. The section is put onto the chuck. Tissue freezing medium used is OCT (Optimal Cutting Temperature) compound. It is poured over the section in the chuck. The chuck is then made to rest on the tissue shelf till it freezes. After that, the chuck is fixed on to the clamping lever. Clearance angle is set between 5-7°. Sections are then cut in 4-5µm thickness with the help of rotary microtome. A glass slide is then made to touch the section. No adhesive is required. The slide is immediately fixed in 95% isopropyl alcohol. Staining is done by the Rapid H & E stain. The slide is analysed by the team of frozen section pathologists and the report delivered as fast as possible either via intercom or by means of a mobile phone and the report dispatched thereafter. The specimen is then sent in formalin for histopathological examination. The frozen section results are compared with the histopathological diagnosis as the gold standard. Data is entered in an excel spreadsheet and statistical analysis (sensitivity, specificity, positive predictive value, negative predictive value, fischer’s exact test) was performed with the help of the software SPSS version 28 (IBM Corp, US).
Results
The mean age of patient was 39.2 years with the minimum age as 21 years and maximum age as 72 years. On frozen section, there were 70%, 16.67% and 13.33% benign, borderline and malignant cases respectively, of which 71.67% were of epithelial origin, 20% of germ cell origin and 1.67% of sex cord stromal origin. On frozen section, there were 30% serous cystadenoma, 11.67% mucinous cystadenoma, 1.67% serous cystadenofibroma, 18.33% mature cytic teratoma, 1.67% fibroma, 16.67% borderline mucinous neoplasm,
11.67% serous cystadenocarcinoma, 1.67% yolk sac tumour, 5% endometriotic cyst and 1.67% granuloma respectively (Table 1).
| Frozen section diagnosis | Number | Percentage (%) | ||
| Benign (38) | Epithelial | Serous cystadenoma | 18 | 30 |
| Mucinous cystadenoma | 7 | 11.67 | ||
| Serous cystadenofibroma | 1 | 1.67 | ||
| Germ cell | Mature cystic teratoma | 11 | 18.33 | |
| Sex cord Stromal | Fibroma | 1 | 1.67 | |
| Borderline (10) | Epithelial | Borderline mucinous neoplasm | 10 | 16.67 |
| Malignant (8) | Epithelial | Serous cystadenocarcinoma | 7 | 11.67 |
| Germ cell | Yolk sac tumour | 1 | 1.67 | |
| Non Neoplastic (4) | Endometriotic cyst | 3 | 5 | |
| Granuloma | 1 | 1.67 |
On histopathological examination there were 73.33%, 8.33% and 18.33% benign, borderline and malignant cases respectively. There were 70% epithelial origin tumours, 21.67% germ cell tumours and 1.67% sex cord stromal tumours. Of the benign neoplasms, there were 30% serous cystadenoma, 13.33% mucinous cystadenoma, 1.67% mucinous adenofibroma, 20 % mature cystic teratoma and 1.67 % fibroma; all 5 cases of borderline neoplasms were mucinous (8.33%); of the malignant neoplasm, 13.33% were high grade serous cystadenocarcinoma, 1.67% each of mucinous cystadenocarcinoma, seromucinous carcinoma and yolk sac tumour; and of the non-neoplastic lesions, 5% were endometriotic cyst and 1.67% granuloma respectively (Table 2).
| Histopathological diagnosis | Number | Percentage (%) | ||
| Benign (40) | Epithelial | Serous cystadenoma | 18 | 30 |
| Mucinous cystadenoma | 8 | 13.33 | ||
| Mucinous adenofibroma | 1 | 1.67 | ||
| Germ cell | Mature cystic teratoma | 12 | 20 | |
| Sex cord Stromal | Fibroma | 1 | 1.67 | |
| Borderline (5) | Epithelial | Borderline mucinous neoplasm | 5 | 8.33 |
| malignant (11) | Epithelial | High grade Serous cystadenocarcinoma | 8 | 13.33 |
| Mucinous cystadenocarcinoma | 1 | 1.67 | ||
| Seromucinous carcinoma | 1 | 1.67 | ||
| Germ cell | Yolk sac tumour | 1 | 1.67 | |
| Non Neoplastic (4) | Endometriotic cyst | 3 | 5 | |
| Granuloma | 1 | 1.67 |
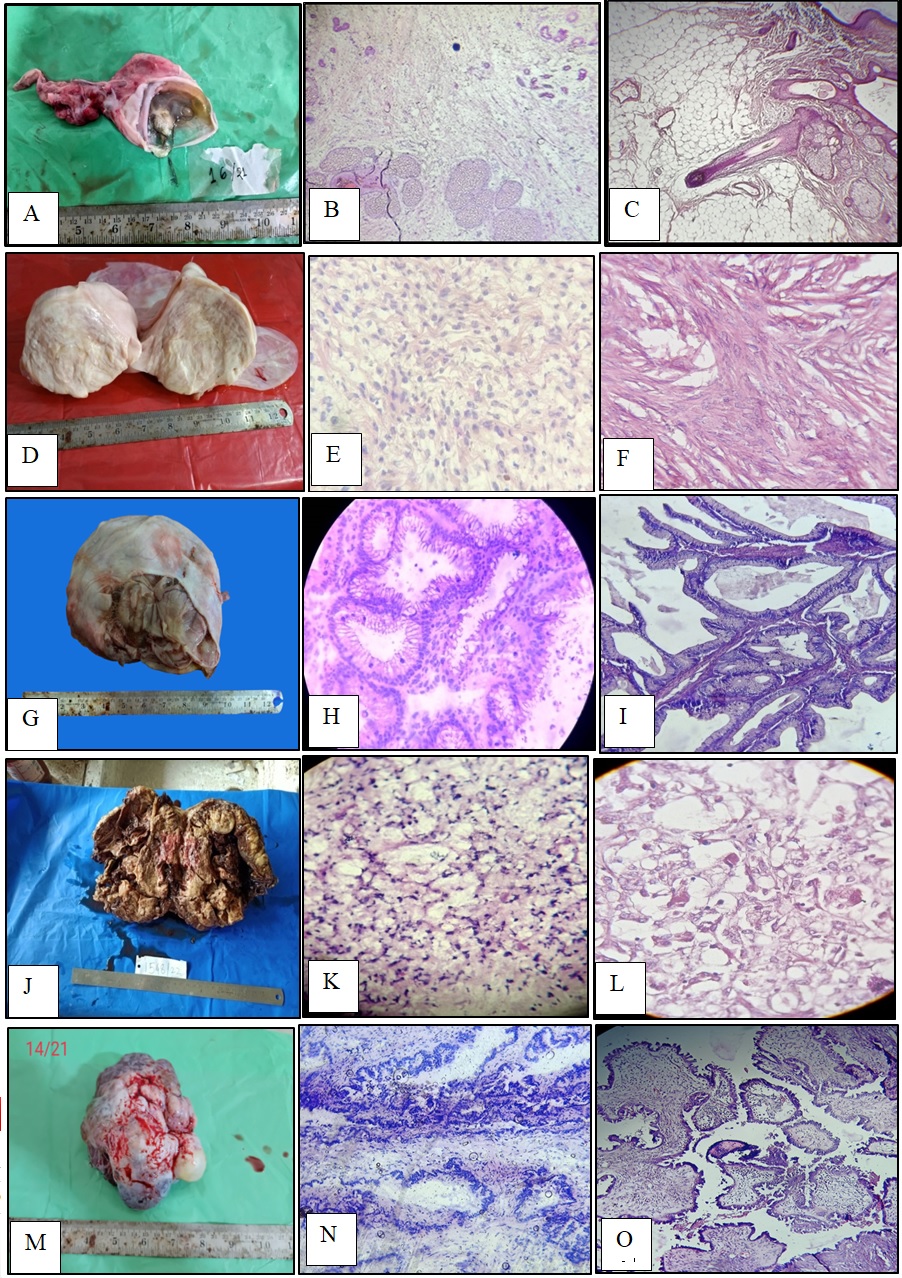
Discrepancy was noted in 5 cases with an overall diagnostic accuracy of 86.67%. Refer to Figure 1 A to O for the different concordant cases in frozen section and histopathological examination. The sensitivity of frozen section for benign, borderline and malignant ovarian neoplasms are 95.45%, 100% and 72.73%; specificity for benign, borderline and malignant ovarian neoplasms are 92.73%, 92.16% and 100%; positive predictive value for benign, borderline and malignant ovarian neoplasms are 97.67%, 55.56% and 100%; negative predictive value for benign, borderline and malignant ovarian neoplasms are 88.24%, 100% and 94.23% respectively.
Figure 1. (A), Gross Image of Mature Cystic Teratoma: Cut Section is Showing Hair and Sebaceous Material. (B), Frozen image (100X) of Mature cystic teratoma showing sebaceous glands, hair follicle and glands. (C), H and E (100X) of Mature cystic teratoma showing hair follicle, sebaceous glands, adipose tissue and stratified squamous epithelium. (D), Gross image of fibroma showing an encapsulated, gray white solid mass covered by an intact glistening ovarian serosa. (E), Frozen image (400X) of Fibroma showing fibroblasts with intersecting bundles of spindle cells. (F), H and E (400X) of Fibroma showing fibroblasts with intersecting bundles of spindle cells. (G), Gross image of Borderline mucinous neoplasm of ovary: cut section showing multiloculation and mucinous content. (H), Frozen image (400X) of Borderline mucinous neoplasm of ovary showing cysts lined by 3-6 layered columnar epithelial lining with apical mucin. (I), H and E (100X) of Borderline mucinous neoplasm of ovary showing 3-5 layer stratification of the columnar lining of the cysts with apical mucin content. (J), Cut section of Yolk sac tumour of ovary showing fleshy gray yellow solid mass with areas of haemorrhage and necrosis.(K), Frozen section image (400X) of Yolk sac tumour showing loose anastomosing channels and variable sized cysts lined by tumour cells. (L), H and E (400X) of Yolk sac tumour of ovary showing variable sized cysts lined by tumour cells with scant cytoplasm, increased nucleo-cytoplasmic ratio, vesicular nucleus and prominent nucleoli and extracellular hyaline globules (eosinophilic). (M), Gross image of Serous cystadenocarcinoma showing multinodular outer surface. (N), Frozen section image (100X) of Serous cystadenocarcinoma showing more than 6 layer epithelial stratification with infiltration of tumour cells into the stroma. (O), H and E (100X) of Serous cystadenocarcinoma showing papillae lined by tumour cells with scant cytoplasm, increased nucleocytoplasmic ratio, hyperchromatic nuclei and prominent nucleoli.
p value is <0.0001, considered to be statistically significant. The average turnaround time of Frozen section is calculated to be 17.92 minutes.
Discussion
The sensitivity, specificity, positive predictive value, negative predictive value of Frozen section in diagnosis of ovarian neoplastic lesions of our study are similar to those of Maheshwari A et al., (2006) [4], Dechsukhum C. et al., (2006) [5], Ilker Arikan et al., (2011) [6], Abdelghany A M et al., (2015) [7], Yazdani Shahla et al., (2015) [8], Utami Tofan W et al., (2015) [9], Jena Madhusmita et al., (2017) [10], Fatemeh Nili et al., (2017) [11], Maheshwari, Dr P (2017) [12], Arshad Nur Zaiti Md et al., (2018) [13], Muruthapongsatorn Piyanat et al., (2019) [14] and Palakkan Saphina et al., (2020) [15].
In our study, Frozen section showed compatibility with histopathological diagnosis in 55 cases with only 5 cases being discordant. 80% of the discordant cases were borderline mucinous neoplasms (Table 3).
| Frozen section diagnosis | Paraffin diagnosis | Type of error | Surgical management | |
| 3/21 | Borderline mucinous cystadenoma | Seromucinous carcinoma | Sampling error | Complete Surgical staging |
| 1/22 | Borderline mucinous tumour | Mucinous cystadenoma | Interpretation error | Complete surgical staging |
| 2/22 | Mucinous cystadenoma with foci of borderline change | Mucinous adenofibroma | Interpretation error | Salpingo-oophorectomy |
| 3/22 | Borderline Mucinous cystadenoma | Papillary serous cystadenocarcinoma | Sampling error | Salpingo-oophorectomy |
| 17/22 | Borderline mucinous neoplasm | Mucinous cystadenocarcinoma | Sampling error | Complete surgical staging |
Out of the 5 discordant cases,3 cases of borderline mucinous neoplasms on frozen section were upgraded to seromucinous carcinoma (Figure 2 A, B & C), mucinous cystadenocarcinoma (Figure 2 J & K) and papillary serous cystadenocarcinoma (Figure 2 H & I) 1 each respectively.
Figure 2. Frozen Section Image (100X) of a Case Misdiagnosed as Borderline Mucinous Neoplasm. Pools of mucin can be noted in the upper left and upper right of the image. Focal areas of nuclear stratification noted at places. (B and C) - H and E (400X) of the same case diagnosed as Seromucinous carcinoma. (B), Section shows multiple cysts with columnar lining epithelium and mucin in the cysts. (C), Section shows more than 6 layered serous linining with hyperchromatic enlarged nuclei and prominent nucleoli. (D), Frozen section image (100X) of a case misdiagnosed as Borderline mucinous neoplasm. (E), H and E (100X) of the same case diagnosed as Mucinous cystadenoma. (F), Frozen section image (100X) of a case misdiagnosed as mucinous cystadenoma with foci of borderline change. (G), H and E (100X) of the same case diagnosed as Mucinous adenofibroma. (H), Frozen section image (400X) of a case misdiagnosed as Borderline Mucinous cystadenoma with foci of microinvasion. (I), H and E (400X) of the same case diagnosed as Papillary serous cystadenocarcinoma of ovary with papillae lined by bizarre tumour cells with increased nucleocytoplasmic ratio, hyperchromatic nuclei,vesicular chromatin and prominent nucleoli (J), Frozen section image (400X) misdiagnosed as Borderline mucinous neoplasm of ovary. Section shows pool of mucin in the lower left and tumour cell nests with hyperchromatic nuclei and apical mucin infiltrating into the ovarian stroma. (K), H and E (400X) of the same case diagnosed as Mucinous cystadenocarcinoma of ovary showing tumour cells with enlarged vesicular nuclei, prominent nucleoli and apical cytoplasmic mucin lining the cysts containing abundant mucinous material.
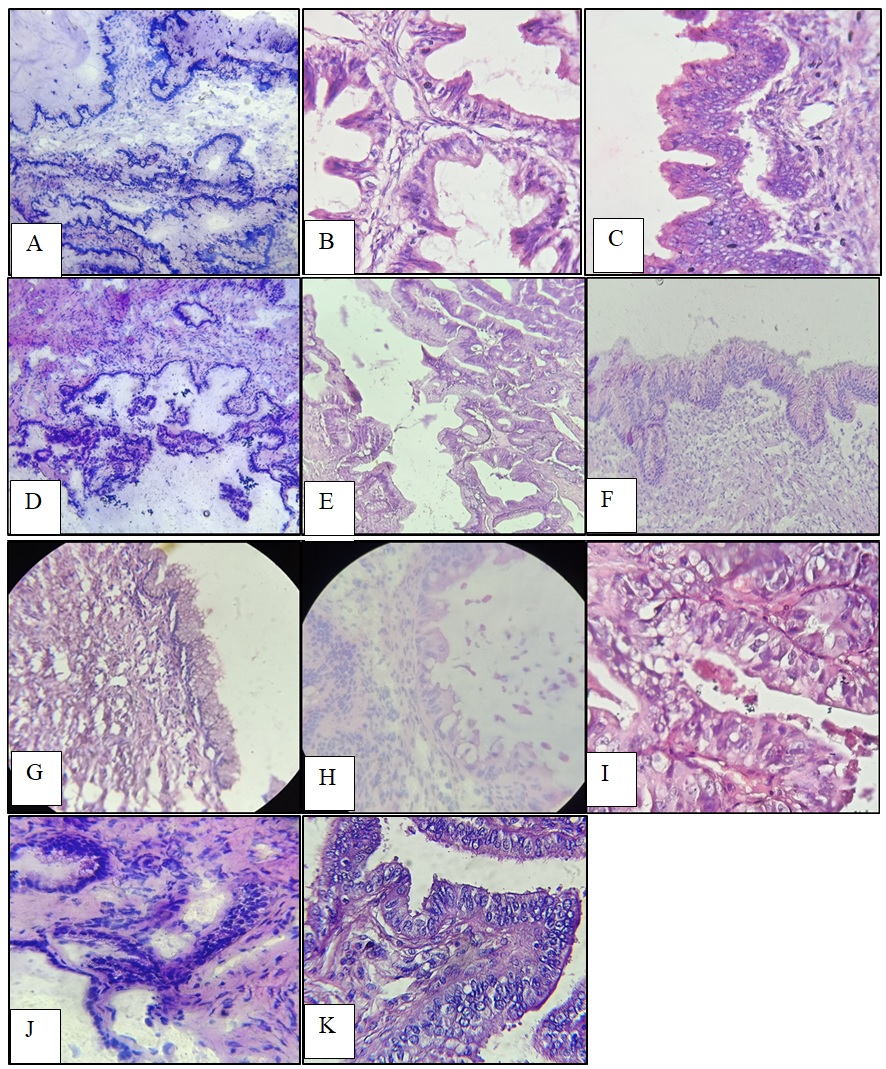
1 case of mucinous cystadenoma with foci of borderline change was downgraded to mucinous adenofibroma on histopathology (Figure 2 F & G) and 1 case of borderline mucinous neoplasm was downgraded to mucinous cystadenoma on histopathology (Figure 2 D & E). There was overdiagnosis in 3.33% cases and underdiagnosis in 5% of the cases. This is largely attributed to the heterogenous nature and the multilocularity of borderline mucinous neoplasms. In 1 case, revision surgery had to be performed after the final histopathological diagnosis as the case of Papillary serous cystadenocarcinoma was misdiagnosed as Borderline Mucinous cystadenoma on frozen section. In the remaining 4 discordant cases, the discrepancy between frozen and routine histopathological diagnoses did not affect the surgical outcome as it also depends on the age of the patient. Of the 5 discordant cases, 60% was due to sampling error and 40% was due to interpretation error. Sampling error occurred due to limited sampling and missing the representative site owing to time restraint. Sampling error can be corrected to a great extent by careful selection of the representative site (areas with solid consistency or papillary configuration) during grossing. However, limited number of sections during frozen section due to the associated time constraint as it is an intraoperative procedure and the pressure on the pathologist to deliver a diagnosis adds to the outcome. Interpretation error can be checked by having a team of expert pathologist review the case and arrive at a diagnosis. This has been found to significantly affect the diagnosis as shown in the study of Brun J L et al [16]. The highest rate of discordant diagnoses was in the case of borderline mucinous neoplasms (4/10) 40%. It may be attributed to the heterogeneity of borderline and malignant tumours and hence the greater chance of missing the representative area in few sections given during frozen section. This is in consistency with the study of Yermez et al [17]. The concordance was found to be higher in the study of Tempfer et al. 62.8% [18]. This may be due to the greater sample size of 317 in their study compared to only 60 in our study. Patients should be counselled before the operative procedure about the importance of Frozen section and the pitfalls associated if there was either a false positive or false negative diagnosis. As well established in our study, sampling of the representative site by both the surgeon and the pathologist is of prime importance to avoid misdiagnosis. Hence, training of pathologists and smooth communication between the surgical team and the frozen section team is crucial to enhance the frozen section report. The limitations of the study are firstly, it was carried out in a relatively small sample size for a period of only 2 years. Secondly, this study was not blinded as the histopathological team was well aware of the frozen section diagnosis before giving their diagnosis.
In conclusion, frozen section of ovarian neoplasms is of great value to the patient as well the surgeon. It helps to arrive at a diagnosis of whether benign or malignant with a high level of accuracy. Borderline neoplasms are associated with the greatest discordance rate. Sampling error is a major cause of discrepancy in frozen section diagnoses. Diagnosis of a benign lesion in a young patient guides the surgeon to a fertility conserving surgery. Likewise, diagnosis of a malignant lesion on table guides the surgeon to execute an extensive surgery in a single setting, saving the patient of the physical, emotional, psychological and financial strain of a second look operation. Diagnosis of a borderline neoplasm in a young patient can guide the surgeon to conduct as conservative a surgery as possible. However, in an elderly patient or when fertility conservation is not indicated, a complete staging surgery should be performed. Hence, especially in such cases, a team of pathologists with experience and expertise should evaluate the case to avoid false diagnoses. Lastly, Frozen section should be made a necessary posting for post graduates as training of young pathologist in intraoperative frozen section would add to the quality of pathologists coming up each year.
Acknowledgements
1) Dr. D J Gharphalia, Professor of Obstetrics and Gynaecology, Gauhati Medical College and Hospital.
2) Mr. Sarafuddin Ahmed, Frozen section technician.
3) Mr. Abdul Hai, Histopathology technician.
4) Mr. Dilip Ranjan Dutta, Histopathology technician.
Statement of Transparency and Principals:
· Author declares no conflict of interest
References
- Ovarian cancer in the world: epidemiology and risk factors Momenimovahed Z, Tiznobaik A, Taheri S, Salehiniya H. International Journal of Women's Health.2019;11. CrossRef
- Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries Bray F, Ferlay J, Soerjomataram I, Siegel RL , Torre LA , Jemal A. CA: a cancer journal for clinicians.2018;68(6). CrossRef
- Ovarian cancer statistics, 2018 Torre LA , Trabert B, DeSantis CE , Miller KD , Samimi G, Runowicz CD , Gaudet MM , Jemal A, Siegel RL . CA: a cancer journal for clinicians.2018;68(4). CrossRef
- Accuracy of intraoperative frozen section in the diagnosis of ovarian neoplasms: Experience at a tertiary oncology center Maheshwari A, Gupta S, Kane S, Kulkarni Y, Goyal LCBK , Tongaonkar HB . World Journal of Surgical Oncology.2006;4. CrossRef
- Accuracy of intraoperative frozen section in diagnosis of ovarian tumors Wootipoom V., Dechsukhum C., Hanprasertpong J., Lim A.. Journal of the Medical Association of Thailand = Chotmaihet Thangphaet.2006;89(5).
- Accuracy of intra-operative frozen section in the diagnosis of ovarian tumours Ilker A, Aykut B, Muge H, Ibrahim HM , Ulku OB , Sener G, Suna S. JPMA. The Journal of the Pakistan Medical Association.2011;61(9).
- Accuracy of Intraoperative Frozen Section in the Diagnosis of Ovarian Neoplasms Abdelghany AM , Arafa EM , Madkour NM , Nossair WS , Mohamed EA , Abdelsalam WA , Salem AA . Open Journal of Obstetrics and Gynecology.2014;5(1). CrossRef
- Accuracy of intra-operative frozen section in the diagnosis of ovarian mass Yazdani S, Bouzari Z, Abedi Samakoosh M, Sharbatdaran M. Caspian Journal of Reproductive Medicine.2015;1(3).
- Accuracy of Intraoperative Frozen Section in Diagnosing Malignancy of Ovarian Neoplasm Utami Tofan W, Iskandar Jasmine , Tanamas Gregorius , Jamtani Mona , Nuranna Laila , Nuryanto Kartiwa H. Indones J Obstet Gynecol.2015;3(3):161-164.
- Role of Frozen Section in the Diagnosis of Ovarian Masses: An Institutional Experience Jena M, Burela S. Journal of Medical Sciences and Health.2017;3(1). CrossRef
- Diagnostic Accuracy of Intraoperative Frozen Section and Causes of Error in Ovarian Epithelial Tumors: An Institutional Experience Original Article Nili F, Soleimani V, Jahanbin B, Jalal-Alhoseini S, Ghanadan A. Middle East Journal of Cancer.2017;8:155-160.
- Role of Frozen Section in the Intra operative management of Ovarian Neoplasms and Comparing with Final Histopathological Diagnosis – A Prospective Study Maheshwari, Dr P. Journal of Medical Science And clinical Research.2017;5(1):15620-15624.
- Intra-Operative Frozen Sections for Ovarian Tumors – A Tertiary Center Experience Arshad NZM , Ng BK , Paiman NAM , Mahdy ZA , Noor RM . Asian Pacific Journal of Cancer Prevention : APJCP.2018;19(1). CrossRef
- The Evaluation of Intra-Operative Frozen Section Diagnosis Accuracy of Ovarian Tumors; Old Fashioned Not Out of Fashion Muruthapongsatorn P, Inploy N, Prommas S, Smanchat B, Bhamarapravatana K, Suwannarurk K. Asian Pacific Journal of Cancer Prevention : APJCP.2019;20(12). CrossRef
- Role of Frozen Section in Surgical Management of Ovarian Neoplasm Palakkan S, Augestine T, Valsan MK , Vahab KPA , Nair LK . Gynecology and Minimally Invasive Therapy.2020;9(1). CrossRef
- Factors influencing the use and accuracy of frozen section diagnosis of epithelial ovarian tumors Brun JL , Cortez A, Rouzier R, Callard P, Bazot M, Uzan S, Daraï E. American Journal of Obstetrics and Gynecology.2008;199(3). CrossRef
- Permanent histological results of ovarian tumors with borderline frozen section result Yermez E, Ata N, Seku I, Balsak D, Sanci M, Ispahi C. Turkiye Klin J Gynecol Obstet.2006;16:165-159.
- Accuracy of intraoperative frozen section analysis in borderline tumors of the ovary: a retrospective analysis of 96 cases and review of the literature Tempfer CB , Polterauer S, Bentz EK , Reinthaller A, Hefler LA . Gynecologic Oncology.2007;107(2). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2023
Author Details