Primary Ovarian Carcinoid Tumor Arising in a Case of Bilateral Mature Teratoma: A Rare Case Report
Download
Abstract
Primary carcinoid of ovary arising in mature solid teratoma is immensely unusual. We report a case of 51-year-old postmenopausal woman came to our emergency room with a complaint of lower abdominal pain, back pain and vomiting. On physical examination a palpable, mobile abdominal mass was noted reaching up to the pelvis. Tumor marker CA-125 was 26.0 U/ml, human chorionic gonadotropin was < 2mIU/ml, serum AFP was <1.3ng/ml, carcinoembryonic antigen level was 1.2mg/ml. Contrast enhanced computed tomographic (CECT) scan of the abdomen revealed a heterogeneously enhancing mass arising in the left adnexa measuring 13x8x15cm showing significant solid component with areas of fat and calcification. No peritoneal disease and abdominal lymphadenopathy. CT findings were suggestive of teratoma. The patient underwent hysterectomy with bilateralsalpingo-oophorectomy. Histopathological examination of left ovary revealed features of carcinoid tumor arising in a mature solid teratoma and right ovary revealed features of mature cystic teratoma.
Introduction
Carcinoid is a usual tumor in lung, gastrointestinal tract however it is infrequent in ovary. Very few cases of primary carcinoid of ovary has been reported and most of them are seen to arise in mature cystic teratoma but as in our case carcinoid arising in mature solid teratoma is immensely unusual. Frequency of occurrence of this tumor in ovary is 0.5% of all carcinoid tumors and 0.1% of all ovarian tumors [1-3]. In view of rarity we are reporting this case.
Case Presentation
A 51-year-old postmenopausal woman came to our institute with a complaint of lower abdominal pain, back pain, vomiting and weakness. The women attained menopause 17years back and presented with above symptoms since 1 year. On physical examination a palpable, mobile abdominal mass reaching up to the pelvis was noted. Hematological and serological investigation were done and it revealed hemoglobin level of 11.40 g/ dL with normal leukocyte and platelet counts, tumor marker CA-125 was 26.0 U/ml, human chorionic gonadotropin was < 2mIU/ml, serum AFP was <1.3ng/ml, carcinoembryonic antigen level was 1.2mg/ml. Contrast enhanced computed tomographic (CECT) scan of the abdomen revealed a heterogeneously enhancing mass arising in the left adnexa measuring 13x8x15cm showing significant solid component with areas of fat and calcification, however the right ovary and uterus were normal in size and not involved by tumor (Figure 1A).
Figure 1. A) CT Scan Showing the Large Predominantly Solid Left Ovarian Mass. B) Uterus and cervix with a small grossly unremarkable right ovary and large left ovarian mass which is predominantly grey yellow and solid. The external surface of left ovary is irregular with smooth glistening capsule (inset). C) Microscopic findings of the right ovary showing respiratory epithelium lining the cystic cavity with cyst wall showing focus of salivary gland acini (inset) (H and E, 10X). D) Right ovarian cyst wall with varying sized thyroid follicles filled with colloid (H and E, 40X)..
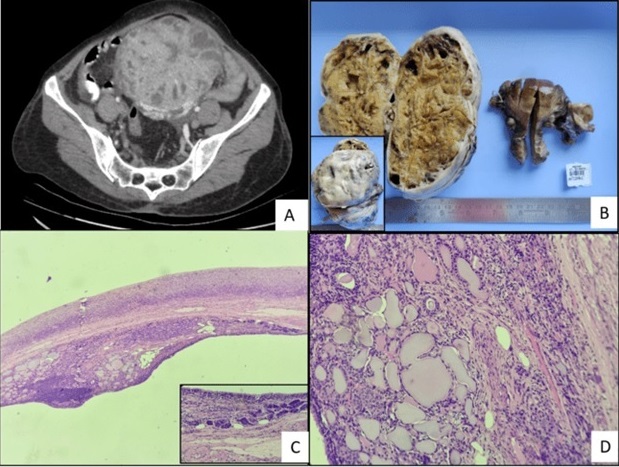
No obvious peritoneal disease and abdominal adenopathy was identified. Minimal pelvic fluid was noted in CECT scan. CT findings were suggestive of teratoma with extensive soft tissue component. Pelvic fluid cytology was reported as negative for atypical cells.
The patient underwent hysterectomy with bilateralsalpingo-oophorectomy, bilateral pelvic lymph node dissection and omentectomy. Specimen was sent to pathology department of our institute for histopathological evaluation. The patient recovered well with no complications and was discharged after two weeks.
Grossly, the left ovary showed a large, lobulated tumor measuring 16×11×7cm. There were no gross areas of capsular breach. On serial slicing the left ovary was completely replaced by the tumor, which was predominantly solid, yellow in color with very few cystic spaces. The solid component showed hair shaft. No normal ovarian tissue was identified in the left adnexal mass. Tumor was abutting the capsule. Areas of hemorrhage and necrosis were identified. A stretched fallopian tube was identified, 6cm in length and is grossly unremarkable (Figure 1B). Grossly right ovary was 2.5x1.5x1.5 cm with smooth and unremarkable external surface. Cut surface showed single hemorrhagic corpus luteal cyst measuring 2.5x2x1 cm. No tumor was identified grossly. A stretched fallopian tube was identified, 7 cm in length and unremarkable grossly.
Uterus with cervix measured 7.5x7.5x3 cm and were unremarkable grossly. A total of 17 lymph nodes identified, grossly free of tumor. Omentum was 15x7x1 cm and grossly unremarkable.
Histopathological examination of right ovary revealed a simple cyst. The cyst wall showed focus of salivary gland acini and thyroid follicles filled with colloid. Pseudostratified ciliated columnar respiratory lining epithelium was also noted. No immature component was identified. It was reported as mature cystic teratoma (Figure 1C,D).
Histopathological examination of left ovary revealed tumor cells arranged in nests, insular pattern, and in rosettoid arrangement. Individual cells are round to oval, have stippled chromatin and a moderate amount of eosinophilic cytoplasm. Areas showed stratified squamous epithelium, dermal appendages, and areas of calcification along with cartilage formation. No immature component identified. The mitotic count was 1-2mitosis/10HPF (Figure 2A-C).
Figure 2. A) Microscopic findings of the left ovary showing areas of stratified squamous epithelium, dermal appendages, and bony tissue (inset) (H and E, 10X). B) Left ovary showing tumor cells arranged in nests, insular pattern, and in rosettoid arrangement (H and E, 10X). C) Tumor cells show stippled chromatin with a moderate amount of eosinophilic cytoplasm (H and E, 40X). D) On immunohistochemistry tumor cells are diffusely positive for CD56.
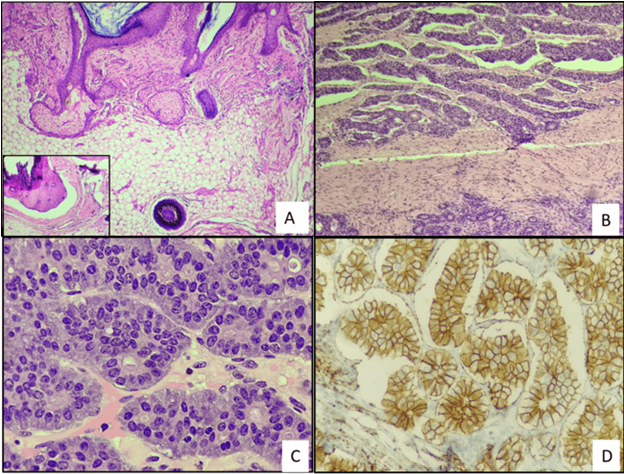
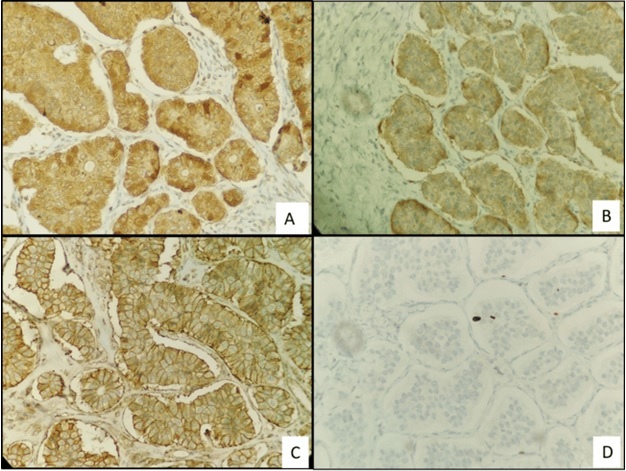
On immunohistochemistry, tumor cells were positive for CD56, Synaptophysin, CD99 while negative for P53, WT-1, Melan A, Calretinin, ER and PR. Ki-67 proliferative index was ~ 2 % (Figure 3A-D).
Figure 3. A) On Immunohistochemistry tumor cells are diffusely positive for chromogranin. B) Tumor cells are positive for synaptophysin. C) CD99 shows diffuse membranous staining of the tumor cells. D) Ki-67 proliferative index is 2 %.
It was reported as features are suggestive of a Carcinoid tumor arising in a mature teratoma.
Section from myometrium, bilateral fallopian tubes, bilateral parametrium showed unremarkable histology. Cervix showed features of chronic cervicitis. Endometrium showed features of an atrophic endometrium. A total of 17 regional lymph nodes identified all of which were free of tumor (0/17).
Discussion
Primary carcinoid of ovary is a well-differentiated neuroendocrine neoplasm resembling carcinoid of gastrointestinal tract. Carcinoid tumors are frequently found in gastrointestinal tract and lung however, primary ovarian carcinoid is a rare event. It has a wide range of age distribution from 14-79 years, mostly occurs in postmenopausal or perimenopausal women (mean, 53 years) [4] in contrast to teratoma which occur in younger age group. More commonly, it is an incidental finding. However, some cases despite absence of metastasis are associated with symptoms of carcinoid syndrome such as lower abdominal pain and vomiting as in our case [5]. Bilateral carcinoid tumoris a rare entity, most carcinoid tumor are unilteral [6,7]. Grossly it is either uniformly solid or represented as nodule/mass within a dermoid cyst, rarely in a mucinous cystic tumor [8]. Histopathology and immunohistochemistry are the gold standard for the diagnosis of carcinoid ovary. Primary carcinoids are subdivided into four histological types insular, trabecular, stromal and mucinous. In insular carcinoid tumor cells are arranged in acini and solid nests whereas trabecular carcinoid shows wavy ribbons or parallel trabeculae of cells surrounded by fibrous stroma. Individual tumor cells have eosinophilic cytoplasm containing red to brown argentaffin granules and round regular nuclei with stippled chromatin [9]. Approximately 40% of carcinoid cases (insular or trabecular) are admixed with struma ovarii, these cases are referred as strumal carcinoid [10]. Primary ovarian mucinous carcinoid tumor characterized by presence of variable number of goblet cells and unlike other types, it has an aggressive course [11]. About 30% of these tumor secrets neurohumoral substances such as serotonin, histamine and bradykinin which leads to carcinoid syndrome [12]. Since it mostly occurs in postmenopausal or perimenopausal women, so treatment of choice is bilateral salpingo-oophorectomy and hysterectomy. However, fertility-sparing surgeries are done in young women [13]. In case of mucinous variant of the ovarian carcinoid, omentectomy and para - aortic lymph node dissection may also be done, since it has an aggressive clinical course [14]. Cinico-radiological preoperative diagnosis of primary ovarian carcinoids arise in mature teratoma is difficult hence, most cases have been diagnosed on postoperative pathology findings [15].
In conclusion, primary carcinoid of the ovary arising from mature solid teratoma is a very rare tumor and most cases are diagnosed after histopathological and the immunohistochemical evaluation, which made us report this case so that surgeon and pathologists are aware of this. With this case report, we have tried to highlight the importance of preoperative clinical and radiological assessment along with postoperative histopathological evaluation of the tumor.
Acknowledgments
Statement of Transparency and Principals:
· Author declares no conflict of interest
· Study was approved by Research Ethic Committee of author affiliated Institute.
· Study’s data is available upon a reasonable request.
· All authors have contributed to implementation of this research.
References
- Ovarian Strumal Carcinoid Tumour: Case Report Antovska VS , Trajanova M, Krstevska I, Gosheva I, Chelebieva J, Prodanova I. Open Access Macedonian Journal of Medical Sciences.2018;6(3). CrossRef
- A 5-decade analysis of 13,715 carcinoid tumors Modlin IM , Lye KD , Kidd M. Cancer.2003;97(4). CrossRef
- An analysis of 8305 cases of carcinoid tumors Modlin IM , Sandor A. Cancer.1997;79(4). CrossRef
- Insular carcinoid primary in the ovary. A clinicopathologic analysis of 48 cases Robboy SJ , Norris HJ , Scully RE . Cancer.1975;36(2). CrossRef
- Peptide YY producing strumal carcinoid tumor of the ovary in a postmenopausal woman: a rare cause of chronic constipation Noh HK , Kwon BS , Kim YH , Lee NK , Choi KU , Suh DS , Lee DH , Kim KH . Obstetrics & Gynecology Science.2017;60(6). CrossRef
- Strumal carcinoid of the ovary: an analysis of 50 cases of a distinctive tumor composed of thyroid tissue and carcinoid Robboy SJ , Scully RE . Cancer.1980;46(9). CrossRef
- [Primary carcinoid of ovary: a clinicopathologic analysis of 17 cases] Zhu R, Xue XW , Luo YF , Wu HW , Huo Z. Zhonghua Bing Li Xue Za Zhi = Chinese Journal of Pathology.2018;47(5). CrossRef
- A strumal carcinoid primary in the ovary De Wilde R, Raas P, Zubke W, Trapp M, Weidenhammer HG , Luis W. European Journal of Obstetrics, Gynecology, and Reproductive Biology.1986;21(4). CrossRef
- Pathology of Neuroendocrine Tumours of the Female Genital Tract Howitt BE , Kelly P P, McCluggage WG . Current Oncology Reports.2017;19(9). CrossRef
- Ovarian strumal carcinoid - case report Ciobanu Apostol DG , BuŢureanu TA , Socolov DG , Scripcaru DC , Rosin OL , Lozneanu L. Romanian Journal of Morphology and Embryology = Revue Roumaine De Morphologie Et Embryologie.2017;58(3).
- Primary ovarian mucinous carcinoid tumor: A case report and review of literature Hsu W, Mao T, Chen C. Taiwanese Journal of Obstetrics & Gynecology.2019;58(4). CrossRef
- Carcinoid Heart Disease in a Primary Ovarian Carcinoid Kolouch T, Linkova H, Lang O, Ciprova V, Brunerova L. Acta Cardiologica Sinica.2016;32(1). CrossRef
- Gynecologic Cancer InterGroup (GCIG) consensus review for carcinoid tumors of the ovary Reed NS , Gomez-Garcia E, Gallardo-Rincon D, Barrette B, Baumann K, Friedlander M, Kichenadasse G, et al . International Journal of Gynecological Cancer: Official Journal of the International Gynecological Cancer Society.2014;24(9 Suppl 3). CrossRef
- Rare case of primary trabecular carcinoid tumor of the ovary with unusual presentation Sharma A, Bhardwaj M, Ahuja A. Taiwanese Journal of Obstetrics & Gynecology.2016;55(5). CrossRef
- An Ovarian Carcinoid Tumor With Peptide YY-Positive Insular Component: A Case Report and Review of the Literature Erdenebaatar C, Yamaguchi M, Saito F, Motooka C, Tashiro H, Katabuchi H. International Journal of Gynecological Pathology: Official Journal of the International Society of Gynecological Pathologists.2016;35(4). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2023
Author Details