Assessment of the HER2 Equivocal Cases in Breast Cancer Following Laterality
Download
Abstract
Background: Breast cancer is a leading cancer among Indian women. Approximately 15-30% of cases are linked to HER2 gene overexpression, impacting survival. Despite the advancements in HER2-targeted therapies equivocal HER2 status poses diagnostic challenges and is comparatively less studied. Breast cancer also displays a peculiar laterality, with a consistent left-sided predominance, yet the underlying factors remain unclear.
Methods: A retrospective analysis of 488 breast cancer cases with equivocal HER2 status confirmed by Fluorescent In-Situ Hybridization (FISH) was conducted. Data included age, hormone receptor status, molecular subtypes, grade, Ki67 status, and FISH scores. Statistical analysis was performed using the R language, and laterality ratios were calculated.
Results: Left-sided breast cancer prevalence was 64.95%, with a laterality ratio of 1.85. Age-related variations and significant laterality preferences were observed in Grade III tumors. Molecular subtypes, particularly Triple Negative, exhibited distinct laterality patterns. Equivocal cases displayed varied FISH scores, emphasizing molecular heterogeneity.
Conclusions: This study provides a comprehensive analysis of HER2-equivocal breast cancer cases, shedding light on laterality patterns and their associations. The observed left-sided predominance suggests potential underlying factors, including age, tumor grade, and molecular subtypes. Understanding these complexities is crucial for personalized treatment strategies and warrants further investigation into the complex interplay of clinicopathological factors influencing breast cancer laterality.
Introduction
Breast cancer is a complicated disease that ranks first in cancer prevalence among Indian women with a cumulative risk of 2.81. Globocan Data 2020 points out that Breast cancer cases in India account for 13.5% and 10.6% of all deaths [1].
Around 15-30% of Breast Cancer cases are linked to overexpression of the HER2 gene which results in increased metastasis risk, higher chances of relapse, and reduced patient survival. The HER2 oncogene, alternatively known as neu, ErbB2, or p185 is situated on the long arm of human chromosome 17(17q12). Human Epidermal Growth Factor Receptor 2 (HER2/ Neu) amplification, a well-established biomarker in breast cancer, has emerged as a critical factor guiding treatment decisions [2]. In recent years, molecular subtyping has revolutionized our understanding of breast cancer, leading to more personalized and targeted therapeutic approaches.
Despite advancements in HER2-targeted therapies, a subset of breast cancer cases remains diagnostically rigorous due to equivocal HER2/Neu status. The equivocal classification introduces a layer of uncertainty, making it necessary to investigate the underlying molecular and clinical characteristics of these cases. Moreover, the consideration of laterality, i.e., the distinction between the right and left breast, adds a new dimension to the analysis. Breast cancer, exhibits a peculiar laterality, with a higher incidence in the left breast compared to the right the published literature is limited but this came to light 80 years ago by Fellenberg et al [3]. Their work drew attention to an elevated incidence of left-sided breast cancer, a consistent observation in the following studies, women demonstrate a slightly higher probability of diagnosis in the left breast compared to the right (ratio ranging from 1.05 to 1.26) [4, 5]. Despite this enduring left-sided predominance, a thorough investigation into the underlying characteristic differences between the left and right breasts remains incomplete. While anatomical variations and inherent differences between paired organs contribute to this phenomenon, the precise factors governing breast cancer laterality remain elusive. Despite various hypotheses proposed in previous studies, such as breast size [6], handedness [7], and lactation patterns [8], a definitive understanding is lacking due to conflicting results and methodological biases.
This research paper aims to provide a thorough analysis of HER2/Neu equivocal cases in breast cancer, with a clear emphasis on laterality patterns. By delving into the complicated molecular factors of equivocal cases, we seek to unravel the underlying factors contributing to HER2/Neu uncertainty and explore the implications of laterality by exploring a comprehensive set of factors, including hormone receptor status, HER2Neu status of equivocal cases confirmed by FISH, age, molecular subtypes, grade, and Ki67 status.
Materials and Methods
Data Collection
In this study, a retrospective analysis of patients with equivocal HER2/Neu IHC status was included where their HER2 status was confirmed using the Fluorescent In-Situ Hybridization (FISH) technique by the cytogenetics department at SN Gene Laboratory Pvt. Ltd. FISH score of less than 2 was considered negative and more than 2 as positive. In total 490 patients were included in the study which were received between January 23 to November
23. We analyzed the data for 488 patients after excluding cases of bilateral breast cancer (2 patients). The clinical characteristics of the patients included were age of patients when received the samples, Status for Estrogen Receptor (ER), Progesterone Receptor (PR) and Ki67, laterality, histologic grade, and FISH result. Data on ER, PR and Ki67 expression status were retrieved from medical records of patients which were assessed using immunohistochemistry. The following variables were analyzed: laterality ratio, the association between tumor laterality and: age as on sample taken for HRE2 FISH analysis by our laboratory for analysis, Estrogen (ER) and Progesterone (PR) Hormonal Receptor Status (positive and negative), HER2 FISH status (positive and negative), molecular subtypes (Triple Negative, Triple Positive, ER+/PR+/HER2-, ER-/PR-/HER2+, ER or PR+), grade (II and III), Ki67 status, FISH Score.
Informed consent was taken from patients
Statistical Analysis
The distribution of clinicopathological factors was compared between left and right breast cancers using the chi-square test to determine the difference between left and right breast cancers concerning each factor.
In addition, the ratio of left breast cancer to right breast cancer (left-to-right LRR) for each factor was analyzed. Percentages were computed for the categorical variables. The number and ratio of left-to right-sided tumors were calculated according to different factors. Charts were used to present categorical variables. All statistical analyses were performed using the R language. P-values of <0.05 were considered statistically significant.
Results
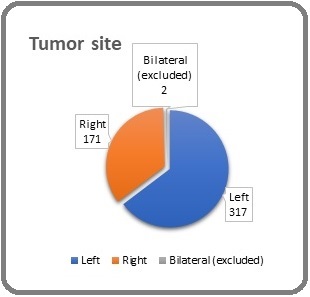
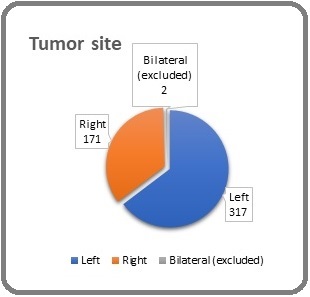
A total of 488 patients across diverse age groups underwent HER2/Neu amplification analysis at the SN Gene Laboratory for cytogenetic study. Samples with 2+ equivocal Immunohistochemistry (IHC) scores, with unilateral breast carcinoma were included in our study. The number of left-sided breast cancer patients was 317 (64.95%) and right-sided breast cancer patients was 171 (35.04%) (Laterality ratio, Lt/Rt 1.85) indicating a slight predominance in the left breast (Figure 1).
Figure 1. Location of the Tumor and the Corresponding Patient Count.
The mean age of patients accounts for 54.90 years and a standard deviation of 11.77 years. Those aged 55 and above show a higher laterality ratio of 1.99, suggesting a greater prevalence of left-sided values compared to the right with age (Table 1).
| Left | Right | Laterality Ratio | P-Value | |
| All Ages | 317 | 171 | 1.85 | 0.7657 |
| <55 | 154 | 89 | 1.73 | |
| >55 | 163 | 82 | 1.99 |
Analysis of different factors in left and right breast cancers
The data reveal variations in the number of cases across age groups, illustrating an increase in overall cases as age advances. The laterality ratio, which assesses the relative involvement of the left and right breasts, exhibits an ascending trend with age, reaching its peak in the >75 age group. Notably, the laterality ratio exceeds 1 in all age groups, indicating a tendency for one side over the other in breast cancer occurrence (Table 2). The R2 value of 0.0421 indicates that the linear regression model explains only a small proportion of the variance in the Laterality Ratio (Figure 2).
Figure 2. A Linear Regression Model was Employed to Examine the Relationship between the Laterality of Unilat- eral Breast Cancer and Age, as Depicted in Table 2.
We carefully assessed the laterality ratios and statistical significance associated with Estrogen Receptor (ER), Progesterone Receptor (PR), and Human Epidermal Growth Factor Receptor 2 (HER2) statuses. For ER, the distribution showed a laterality ratio of 1.86 for negative cases and 1.85 for positive cases, indicating asymmetry that lacked statistical significance.
(P = 0.9989). An assessment of PR status showcased a potential laterality preference for PR-negative tumors without reaching statistical significance (P = 0.3671). Exploring HER2 status, indicated higher HER2 negative cases on the left side with a left-to-right ratio 2.01 (Table 2).
| Left (%) | Right (%) | Overall (%) | Laterality Ratio | P- value | |
| N % | 317 (64.95) | 171 (35.04) | 488 (100) | 1.85 | |
| Age | |||||
| <35 | 10 (3.15) | 3 (1.75) | 13 (2.66) | 3.33 | 0.4255 |
| 35-45 | 49 (15.45) | 39 (22.80) | 88 (18.03) | 1.26 | |
| 45-55 | 95 (29.96) | 47 (27.48) | 142 (29.09) | 2.02 | |
| 55-65 | 86 (27.13) | 46 (26.90) | 132 (27.05) | 1.87 | |
| 65-75 | 63 (19.87) | 30 (17.54) | 93 (19.06) | 2.1 | |
| >75 | 14 (4.41) | 6 (3.50) | 20 (4.09) | 2.33 | |
| ER | |||||
| Negative | 149 (47.00) | 80 (46.78) | 229 (46.93) | 1.86 | 0.9989 |
| Positive | 168 (52.99) | 91 (53.21) | 259 (53.07) | 1.85 | |
| PR | |||||
| Negative | 154 (48.58) | 75 (43.85) | 229 (46.93) | 2.05 | 0.3671 |
| Positive | 163 (51.42) | 96 (56.14) | 259 (53.07) | 1.7 | |
| HER2 | |||||
| Negative | 227 (71.61) | 113 (66.08) | 340 (69.67) | 2.01 | 0.2444 |
| Positive | 90 (28.39) | 58 (33.92) | 148 (30.33) | 1.55 | |
| Molecular Subtype | |||||
| Triple Negative | 103 (32.49) | 46 (26.90) | 149 (30.53) | 2.24 | 0.4532 |
| Triple Positive | 49 (15.46) | 30 (17.54) | 79 (16.19) | 1.63 | |
| ER+/PR+/HER2- | 103 (32.49) | 58 (33.82) | 161 (32.99) | 1.78 | |
| ER-/PR-/HER2+ | 35 (11.04) | 26 (15.20) | 61 (12.50) | 1.35 | |
| ER or PR+ | 27 (8.52) | 11 (6.43) | 38 (7.79) | 2.45 | |
| Grade * | |||||
| II | 108 (34.73) | 82 (48.52) | 190 (39.58) | 1.32 | 0.0043 |
| III | 203 (65.27) | 87 (51.48) | 290 (60.42) | 2.33 | |
| Ki 67** | |||||
| <20% | 13 (4.42) | 4 (2.55) | 17 (3.77) | 3.25 | 0.4618 |
| >20% | 281 (95.58) | 153 (97.45) | 434 (96.23) | 1.84 |
*Data Not Available For 8 Patients, **Data Not Available For 37 Patients
Investigation of distribution and laterality patterns across molecular subtypes. Notably, the Triple Negative subtype exhibited a laterality ratio of 2.24, indicating a higher prevalence in the left breast. Conversely, the Triple Positive subtype demonstrated a laterality ratio of 1.63, reflecting a less pronounced asymmetry between the left and right breasts. The ER+/PR+/HER2- subtype showed a laterality ratio of 1.78, suggesting a modest preference for the left breast. Similarly, the ER-/PR-/HER2+ subtype displayed a laterality ratio of 1.35. Interestingly, the ER or PR+ subtype exhibited a more notable laterality ratio of 2.45, implying a potential inclination for the left breast, though these differences lacked statistical significance (P = 0.4532) (Table 2).
In our in-depth examination of 480 breast cancer cases with available grade data, the investigation into grade distribution revealed intriguing laterality patterns. Grade II tumors exhibited a laterality ratio of 1.32, indicating a moderate affection for the left breast. Conversely, Grade III tumors demonstrated a significant laterality ratio of 2.33, suggesting a marked preference for the left breast, and this finding was statistically significant with a P-value of 0.0043 (Table 2).
The analysis revealed distinctive laterality patterns in our investigation of 451 breast cancer cases with available Ki-67 expression data. Notably, tumors with Ki-67 expression below 20% demonstrated a substantial laterality ratio of 3.25, suggesting a notable tendency for the left breast. Conversely, tumors with Ki-67 expression above 20% displayed a laterality ratio of 1.84, indicating a more balanced distribution between the left and right breasts. However, these differences did not reach statistical significance (P = 0.4618) (Table 2).
In our scrutiny of 147 breast cancer cases with positive Fluorescence In Situ Hybridization (FISH) results, the investigation into FISH scores revealed distinctive laterality patterns. Tumors with a FISH score in the range of 2- 4 exhibited a laterality ratio of 1.33, indicative of a slight predilection for the left breast. Similarly, tumors with a FISH score in the range of 4-6 displayed a laterality ratio of 1.92, signifying a more pronounced predilection for the left breast. Tumors with a FISH score exceeding 6 exhibited a laterality ratio of 1.80, denoting a noteworthy predilection for the left breast (Table 3).
| Fish Score | Left | Right | Laterality Ratio | Remark | Overall |
| 2>x>4 | 48 | 36 | 1.33 | Positive | 84 |
| 4>x>6 | 23 | 12 | 1.92 | Positive | 35 |
| >6 | 18 | 10 | 1.8 | Positive | 28 |
Analysis of Equivocal Cases for FISH Score
The distribution of HER2Neu status in breast cancer cases is illustrated in Table 4 showcasing associations with age, Ki67 expression, and grade.
| Positive | Negative | |
| AGE | ||
| <35 | 5 | 8 |
| 35-45 | 28 | 60 |
| 45-55 | 42 | 100 |
| 55-65 | 46 | 86 |
| 65-75 | 21 | 72 |
| >75 | 6 | 14 |
| Ki67 | ||
| <20% | 4 | 13 |
| >20% | 135 | 299 |
| Grade | ||
| II | 51 | 139 |
| III | 93 | 197 |
Across age groups, the prevalence of HER2Neu-positive cases tends to vary, with notable frequencies in the 35-45 and 45-55 age brackets. Regarding Ki67 expression, a substantial number of cases with HER2Neu positivity are observed in both <20% and >20% expression categories. Notably, in the grade analysis, HER2Neu-positive cases are distributed across Grade II and Grade III tumors, reflecting the diverse molecular landscape within these grades.
Among cases with Ki67 expression below 20%, there are 3 instances with a FISH score in the range of 2-4 and 1 case with a FISH score exceeding 6. In contrast, cases with Ki67 expression above 20% exhibit a varied distribution across FISH scores, with 78 cases in the 2-4 range, 32 cases in the 4-6 range, and 24 cases with a FISH score exceeding 6. This Table, elucidates the intricate relationship between Ki67 expression and FISH scores, shedding light on potential molecular heterogeneity within distinct Ki67 expression levels in the examined breast cancer cohort.
Discussion
The presented study provides a comprehensive analysis of 2+ equivocal IHC cases which were received by the laboratory for further FISH confirmation from different parts of India, HER2/Neu amplification and its association with various factors in a cohort of 488 breast cancer patients. The findings offer valuable insights into the laterality patterns of breast cancer, considering factors such as age, hormone receptor status (ER and PR), HER2 status, molecular subtypes, tumour grade, Ki-67 expression, and Fluorescence In Situ Hybridization (FISH) scores. There is a lack of research regarding the laterality of breast cancer in India. This study explored the issue of laterality in Indian female patients.
Early findings suggested a somewhat poorer outlook for breast cancers on the left side, attributed to the impact of radiotherapy on the myocardium in the left hemithorax [9-11]. However, subsequent reports did not universally support this observation, and advancements in radiotherapy techniques contributed to a reduced incidence of radiotherapy-related cardio toxicity overall [12].
One of the key observations is the predominance of left-sided breast cancer, with a laterality ratio (Lt/Rt) of 1.85 across the entire cohort. Sughue et al. conducted a study in the USA, examining 1.2 million breast cancer cases spanning from 1973 to 2010. Their findings indicated that the laterality ratio is influenced by the country of birth rather than race. Individuals born in Japan (l/r = 1.14, p = 0.997), the Ryukyu Islands (l/r = 2.6, p = 0.998), Laos (l/r = 1.62, p = 0.9999), and Algeria (l/r = 2.1, p = 0.9959) exhibited significantly larger laterality ratios compared to the overall SEER population (l/r = 1.04). Conversely, those born in Poland (l/r = 0.92, p = 0.997) demonstrated a laterality ratio significantly lower than expected [13].
Additionally, the study observed a statistically significant rise in the laterality ratio with advancing age [13], Consistent with these results, the laterality ratio tends to increase with age, reaching its peak in the >75 age group. This suggests a potential age-related influence on the laterality of breast cancer occurrence. The hypothesis posits that right-handed individuals tend to scrutinize their left-side breast and axilla more meticulously than their right-side counterparts. Consequently, this heightened attention may facilitate the earlier detection of smaller breast lesions in the left-side breast compared to the right-side breast [14, 15, 4]. Another suggestion is that this phenomenon may be attributed to a potentially stronger cell-mediated immune activity in the left side of the human body [16].
The total mean age of the patients in the study was 54.90 years. Left-sided breast cancer was more prevalent in all age groups. In contrast, a study conducted in North India by Kakkar et al. reported a higher ratio of left-sided breast cancer among pre-menopausal patients, whereas the incidence of right-sided breast cancer was elevated in the postmenopausal group. The study proposed a potential explanation for this pattern, suggesting that differences in estrogen hormone levels between the two groups could play a role [17].
The study further explores the association between laterality ratios and hormone receptor status. The molecular subtyping of breast cancer has emerged as a crucial determinant in forecasting prognosis and customizing treatment strategies [18], While ER and PR status do not show statistically significant laterality preferences, there is a notable predilection for HER2-negative cases in the left breast. The analysis of molecular subtypes reveals intriguing patterns, with the Triple Negative subtype exhibiting a higher prevalence in the left breast. Additionally, the study highlights laterality preferences in different tumor grades and Ki-67 expression levels.
The significant laterality ratio observed in Grade III tumors suggests a marked preference for the left breast, emphasizing the potential importance of tumor grade in understanding laterality patterns. The association between Ki-67 expression and laterality patterns adds another layer of complexity, with tumors below 20% expression showing a substantial left-sided predilection.
The investigation into FISH scores further elucidates the laterality patterns, with varying degrees of predilection for the left breast across different FISH score ranges. The analysis of equivocal cases concerning FISH score emphasizes the need for a nuanced understanding of molecular heterogeneity within distinct Ki-67 expression levels.
In conclusion, the study contributes valuable information about the laterality patterns of breast cancer and their association with various clinicopathological factors. The findings underscore the intricate relationships between age, hormone receptor status, molecular subtypes, tumor grade, and molecular markers, providing a foundation for further research into the underlying mechanisms influencing the laterality of breast cancer
Acknowledgments
Statement of Transparency and Principals:
· Author declares no conflict of interest
· Study was approved by Research Ethic Committee of author affiliated Institute.
· Study’s data is available upon a reasonable request.
· All authors have contributed to implementation of this research.
References
- Breast cancer in India: Present scenario and the challenges ahead Mehro R, Yadav k. World Journal of Clinical Oncology.2022;13(3). CrossRef
- Human Epidermal Growth Factor Receptor 2 (HER2) in Cancers: Overexpression and Therapeutic Implications Iqbal N, Iqbal N. Molecular Biology International.2014;2014. CrossRef
- Schweiz. Erhebung Fiber Maligne Tumoren [Switzerland Survey of malignant tumors]. Bull Eidgenoss Gesundheitsamt. 1940 Von Fellenberg R. .
- Breast cancer laterality and molecular subtype likely share a common risk factor Cheng S, Liang L, Liang Q, Huang Z, Peng X, Hong X, Luo X, et al . Cancer Management and Research.2018;10. CrossRef
- Left sided breast cancer is associated with aggressive biology and worse outcomes than right sided breast cancer Abdou Y, Gupta M, Asaoka M, Attwood K, Mateusz O, Gandhi S, Takabe K. Scientific Reports.2022;12(1). CrossRef
- The side and size of breast tumours Hartveit F. Clinical Oncology.1983;9(2).
- Handedness and breast cancer characteristics Altundag K, Isik M, Sever AR . Journal of B.U.ON.: official journal of the Balkan Union of Oncology.2016;21(3).
- Unilateral breast-feeding and breast cancer Ing R, Petrakis NL, Ho JH. Lancet (London, England).1977;2(8029). CrossRef
- The Effect of Laterality and Primary Tumor Site on Cancer-Specific Mortality in Breast Cancer: A SEER Population-Based Study Bao J, Yu K, Jiang Y, Shao Z, Di G. PLoS ONE.2014;9(4). CrossRef
- Lower incidence but more aggressive behavior of right sided breast cancer in Pakistani women: does right deserve more respect? Fatima N, Zaman MU , Maqbool A, Khan SH , Riaz N. Asian Pacific journal of cancer prevention: APJCP.2013;14(1). CrossRef
- Breast cancer laterality among Egyptian patients and its association with treatments and survival Zeeneldin AA , Ramadan M, Elmashad N, Fakhr I, Diaa A, Mosaad E. Journal of the Egyptian National Cancer Institute.2013;25(4). CrossRef
- Breast cancer laterality does not influence survival in a large modern cohort: implications for radiation-related cardiac mortality Rutter CE , Chagpar AB , Evans SB . International Journal of Radiation Oncology, Biology, Physics.2014;90(2). CrossRef
- Breast tumor laterality in the United States depends upon the country of birth, but not race Sughrue T, Brody JP . PloS One.2014;9(8). CrossRef
- Laterality of Breast Cancer - is it true? Badru F, Chianakwalam C, Stevenson V. European Journal of Surgical Oncology.2011;37(11). CrossRef
- Epidemiology of breast carcinoma II: factors related to the predominance of left-sided disease Senie RT , Rosen PP , Lesser ML , Snyder RE , Schottenfeld D, Duthie K. Cancer.1980;46(7). CrossRef
- Asymmetries in breast cancer lateralization and both axillary lymph node number and metastatic involvement Dane S, Yildirim S, Koc M, Aktan M, Gundogdu C. Lymphology.2008;41(2).
- Trends of breast tumour laterality and age-wise incidence rates in North Indian population Kakkar V, Sharma R, Singh K, Randhawa A. International Surgery Journal.2020;7(8). CrossRef
- Prognostic models for breast cancer: a systematic review Phung MT , Tin Tin S, Elwood JM . BMC cancer.2019;19(1). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2024
Author Details