Advancing Cancer Care Infrastructure in Cambodia: Summary of the First 100 Patients with Cervical Cancer Treated at the National Cancer Centre
Download
Abstract
Background: Cervical cancer is Cambodia’s leading cause of female malignancy in both incidence and mortality. Cambodia’s first dedicated multidisciplinary cancer center, the National Cancer Centre (NCC), opened in January 2018 in Phnom Penh, and serves as the main public referral center for the region.
Methods: This cross-sectional study retrospectively reviewed the care experience of the first 100 patients with cervical cancer treated at the NCC to collect demographic, diagnostic, and treatment characteristics.
Results: The most common FIGO Stage was IIB (T2bN0M0) (n = 17). Squamous cell carcinoma represented 85% of cases. Definitive-intent therapy was recommended for 65 patients; neoadjuvant chemotherapy followed by external beam radiotherapy (EBRT) & tandem and ovoid (T&O) brachytherapy +/- concurrent cisplatin was the most common treatment regimen (n=23). Thirty-five patients presented with recurrent (n=22) or metastatic (n=13) disease and were treated with salvage/palliative intent; neoadjuvant chemotherapy followed by EBRT +/- concurrent cisplatin was the most common treatment regimen (n=10). Of the patients treated with definitive-intent treatment, 92% were prescribed an EBRT dose of 45 Gy in 25 fractions, and the median prescribed T&O brachytherapy dose was 28 Gy in 4 fractions. Mean cumulative EQD2 HR-CTV D90 dose was 91.8 Gy, or ~69-70 Gy to Point A, depending on planning technique. Follow-up data was limited to 27 patients; of the 14 patients whose follow-up period exceeded 1 year, 13 (93%) were alive and disease-free at their last assessment.
Conclusion: With multidisciplinary partnership, the NCC has demonstrated that high quality complex cancer care can be delivered in a resource-constrained setting. This early sample of patients treated for cervical cancer is an initial step towards a better understanding of Cambodia’s patient population and an early snapshot of their cancer care delivery capacity.
Introduction
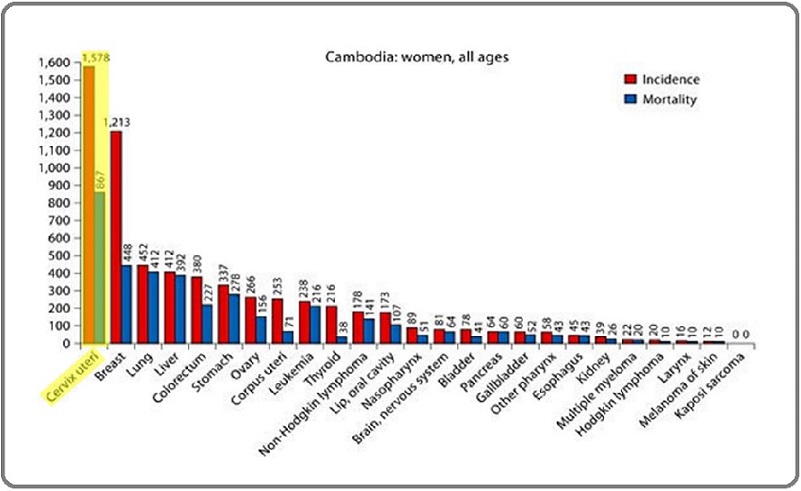
Cervical cancer is estimated to comprise at least 25% of all malignancies in Cambodian women, making it the most common cancer among females. Some reports estimate ~1500 new cases, and ~800 deaths annually (mortality-to-incidence ratio = 0.53) [1, 2]. Figure 1 illustrates the incidence and mortality of cervical cancer in Cambodia compared to other primary cancer sites in women.
Figure 1. Incidence and Mortality Rates of the Most Prevalent Primary Sites of Cancer among Cambodian women. Adapted from Eav et al. 2012.
The same authors suggest that 70% of new cervical cancer cases present with stage III/IV disease [1]. Cambodia does not yet have a comprehensive national cancer registry nor a comprehensive cervical cancer screening program, so exact epidemiological figures are difficult to determine.
Recent estimates of cervical cancer incidence come from a 2014 – 2017 pilot screening program from Cambodia’s Ministry of Health using visual inspection with acetic acid (VIA) [3]. Participation peaked in the third year (2016) with almost 60,00 women, and the number of women suspected of cancer peaked in the fourth year (2017) at 1154, approaching the aforementioned estimated incidence rate of cervical cancer [3].
The history of cancer care in Cambodia was profoundly affected by the Khmer Rouge from the mid-1970s until the end of the 1990s, during which upwards of 2 million Cambodians – approximately 25% of the population at the time – were killed. The country’s healthcare infrastructure was a major casualty in the conflict; hospitals and clinics were abandoned, equipment was destroyed, and healthcare professionals were persecuted.
Cambodia’s first dedicated multidisciplinary cancer center, the National Cancer Centre (NCC), opened on January 15, 2018, in Phnom Penh at Calmette Hospital. As a public hospital, the NCC is supported by the Cambodian government, the French government, and the International Atomic Energy Agency (IAEA).
The NCC aims to fill in many gaps in cancer care and training in Cambodia. Its stated missions are to 1) provide modern multidisciplinary cancer care to the Cambodian population, and 2) provide advanced oncological training for Cambodian health care professionals. As a teaching hospital, the NCC began training its first five oncology residents in 2018 and accepts five new residents each year. Since opening, the NCC has provided thousands of Cambodians with their first access to modern cancer care. The NCC opened with one 6 & 10MV dual energy linac (only the second in the country), a 16-slice planning CT scanner, and a gamma camera donated by the IAEA. The linac and CT scanner were installed in 2017 and began operations on March 27th, 2018. The hospital installed an Ir192 HDR brachytherapy unit in July 2018 and began brachytherapy treatment in August 2018.
Here we report data on the clinical course, treatment characteristics, and outcomes of the first 100 patients with cervical cancer treated at the NCC. Recognizing that resource limitations greatly impact capacity for treatment, our hope is that a better understanding of the patient population and their oncological care experience can help promote clinical research and inform future decision making for quality improvement in similar settings.
Materials and Methods
Study Design and Population
This is a retrospective review conducted at the NCC in Phnom Penh, Cambodia. Study approval was obtained from Cambodia’s National Ethics Committee for Health Research.
The first 100 patients with cervical cancer treated at the NCC were identified by registration date in the radiation oncology electronic database. Hospital records from the gynecology, oncology, surgery, radiology, radiation oncology and pathology departments were reviewed to collect demographic, diagnostic, and treatment data for each patient. Radiotherapy data was digitized, records in other departments were paper records.
Statistical Analysis
Categorical data are presented as frequency and proportion, with patients’ missing data recorded as an additional category “unknown” rather than removing them from the denominator. Continuous data are presented as range, mean, median, and mode. All calculations were done using Microsoft Excel.
Missing data was assumed to be missing completely at random and thus excluded from analyses.
Outcomes
Clinical outcome data was limited to only 27 of these patients mostly due to the majority of patients living outside Phnom Penh and not being available for follow-up. Outcome data was collected via phone follow-up visits and review of medical records. Information was collected on the development of radiation therapy-related toxicities, locoregional recurrence, distant metastases, and overall survival.
Results
Patient & Disease Characteristics
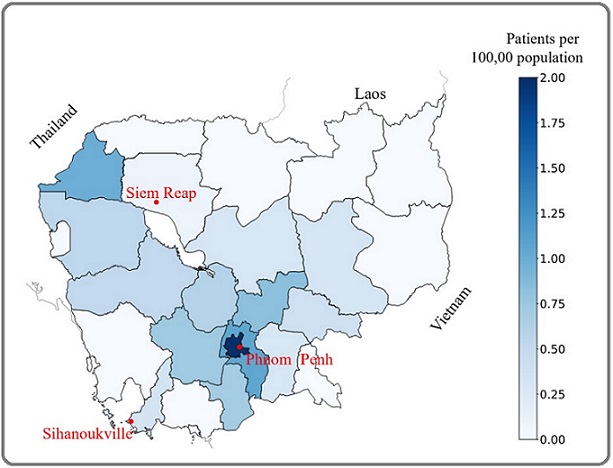
Of the first 100 patients treated at the NCC for cervical cancer, 60% resided outside Phnom Penh province. Figure 2 shows a choropleth map displaying the prevalence of cervical cancer cases treated at NCC based on the patients’ province of residence.
Figure 2. Comparative Prevalence of Cervical Cancer within Cambodia by Province.
Patient and tumor characteristics at diagnosis are summarized in Table 1.
| Median Age | 55 (25-81) | ||
| Province of Origin | Frequency (%) | ||
| Phnom Penh | 40 | ||
| Outside Phnom Penh | 60 | ||
| Comorbidities per patient | % Total (n = 100) | ||
| 0 | 47 | ||
| 1 | 35 | ||
| 2 | 9 | ||
| Unknown | 9 | ||
| Specific comorbidities | Frequency | % Total (n = 44) | |
| Hypertension | 28 | 63.64 | |
| Diabetes | 12 | 27.27 | |
| HIV | 3 | 6.82 | |
| Tuberculosis | 3 | 6.82 | |
| Hep A/B Cirrhosis | 2 | 4.55 | |
| Arthritis | 2 | 4.55 | |
| Major depressive disorder | 1 | 2.27 | |
| Hypothyroidism | 1 | 2.27 | |
| Method of Diagnosis | % Total (n = 100) | ||
| Biopsy | 82 | ||
| Surgical specimen | 9 | ||
| Pap smear | 1 | ||
| Unspecified histopathology | 8 | ||
| FIGO Stage 4 | Equivalent TNM Stage 5 | % Total (n = 100) | |
| I | T1N0M0 | 23 | |
| II | T2N0M0 | 36 | |
| III | T3N (ANY) M0 T1, 2N1M0 | 21 | |
| IV | T4N (ANY) M0 T (ANY) N (ANY) M1 | 14 | |
| Unknown | 6 | ||
| Modal Stage (n = 17) | FIGO: IIB | TNM Equivalent: T2bN0M0 | |
| Histology | % Total (n = 100) | ||
| Squamous cell carcinoma | 85 | ||
| Adenocarcinoma | 9 | ||
| Unknown | 6 |
Treatment
Patients were treated with a combination of hysterectomy, chemotherapy and/or radiation therapy. In total, 65 patients were recommended to undergo definitive intent therapy. The most common treatment course among these patients was neoadjuvant chemotherapy followed by external beam radiotherapy (EBRT) & intracavitary tandem and ovoid (T&O) brachytherapy +/- concurrent cisplatin (n=23).
An additional 35 patients presented with recurrent (n=22) or metastatic (n=13) disease and were treated with salvage/palliative intent. The most common salvage regimen prescribed was neoadjuvant chemotherapy followed by EBRT +/- concurrent cisplatin (n=10). A description of the various treatment paradigms is summarized in Table 2.
| Treatment Paradigms | ||
| Definitive intent (n = 65) | Frequency | % of Total (n = 65) |
| NACT → EBRT +/- cis + BT | 23 | 35 |
| EBRT +/- cis + BT | 17 | 26 |
| Sx → EBRT +/- cis +/- VBT | 9 | 14 |
| Sx → CT → EBRT +/- cis +/- VBT | 7 | 11 |
| NACT → Sx → EBRT +/- cis +/- VBT | 5 | 8 |
| NACT → EBRT +/- cis → Sx | 2 | 3 |
| EBRT +/- cis → Sx | 1 | 2 |
| NACT → EBRT +/- cis + BT →ACT | 1 | 2 |
| Salvage/Palliative intent (n = 35) | Frequency | % Total (n = 35) |
| NACT → EBRT +/- cis | 10 | 29 |
| EBRT +/- cis +/- VBT | 6 | 17 |
| CT → EBRT +/- cis +/- VBT | 4 | 11 |
| EBRT +/- cis | 3 | 9 |
| CT → EBRT +/- cis + BT | 2 | 6 |
| EBRT +/- cis + BT | 2 | 6 |
| EBRT +/- cis +/- VBT → ACT | 2 | 6 |
| CT → EBRT +/- cis | 1 | 3 |
| CT → EBRT +/- cis → Sx | 1 | 3 |
| CT → EBRT +/- cis +/- VBT → ACT | 1 | 3 |
| CT → EBRT +/- cis +/- VBT → Sx | 1 | 3 |
| EBRT +/- cis | 1 | 3 |
| EBRT +/- cis + BT → ACT | 1 | 3 |
CT, chemotherapy; NACT, neoadjuvant chemotherapy; Cis, concurrent chemotherapy w/ cisplatin; ACT, adjuvant chemotherapy; Sx, definitive surgical therapy; EBRT, external beam radiotherapy; BT, T&O brachytherapy; VBT, vaginal cuff (segmented cylinder) brachytherapy
Of the 26 patients who underwent surgical therapy, 25 had hysterectomies: 3 radical; 2 modified radical;
13 simple; and 7 unspecified. The remaining 1 patient underwent a subtotal exenteration. Ten patients (38.5%) underwent lymph node dissection, with a median of 8.5 nodes retrieved (2 – 15). Twenty patients (77%) were treated for FIGO stage I or II disease (TNM stage T1N0M0 - T2N0M0) [4, 5].
Of the 100 patients who were evaluated for radiotherapy at the NCC, 96 started treatment and 87 patients completed their radiotherapy course as planned. Three patients discontinued their radiotherapy course due to deteriorating health, four patients due to unknown reasons, and two patients passed away during their course. Additionally, 15 patients began their EBRT course before the launch of the brachytherapy program, leading to a delay between the end of their EBRT and the start of brachytherapy, thus prolonging their total treatment time. Duration of treatments are summarized in Table 3.
| Median duration of all radiotherapy courses (EBRT+/-BT) (days) (n=96) | 71 (7-275) | |
| Median duration of definitive intent EBRT + BT (days) (n=42) | 71 (47 - 275) | |
| Median duration from NCC consultation to initiation of definitive intent RT (days) (n=41) | 42 (0 - 317) | |
| Pelvic EBRT (n=100) | 45 (29.6 - 50.4) | |
| Parametrial Boost (n=29) | 5.4 (5.4 - 14.8) | |
| Median Prescribed Dose (Gy) | Nodal Boost (n=4) | 7.2 (5.4 - 9) |
| T&O brachytherapy (n=42) | 28 in 4 fractions (18-28) | |
| Cylinder VBT (n=21) | 18 in 3 fractions (18) | |
| Median Cumulative dose (EQD2): | HRCTV D90 | 91.8 (71.2 - 117.1) |
| EBRT + T&O brachytherapy | Bladder D2cc | 77.8 (58 – 90.9) |
| (Gy) (n = 42) | Rectum D2cc | 69.7 (53.8 – 78.2) |
| Median Total Dose to Point A | Left | 68.8 (57.9 - 79.6) |
| (Gy) (n=42) | Right | 69.6 (58.7 - 79.9) |
100% of patients treated with EBRT underwent CT simulation, and were treated with a 3D conformal (92%) or 4-field box technique (8%). Organs at risk were contoured in 44% of cases. A combination of 3D conformal, 4-field box, and parallel opposed field planning was used for EBRT boosts. The planning target volume (PTV) margin was 5mm for all patients. A pelvic field was used for all patients receiving EBRT, with 19% treated with an additional paraaortic field. EBRT dose ranged from 29.6- 50.4 Gy, with 92% prescribed 45 Gy in 25 fractions.
Prescribed RT regimens are listed in Table 3, along with cumulative EQD2 doses, Point A doses, and treatment duration. 5 patients had initial intake at the NCC before the Centre began its EBRT operations in March 2018, causing a delay in their treatment start and possibly inflating this value artificially.
Of the 65 patients receiving definitive intent treatment, 58 (89.2%) received chemotherapy as a part of their care. Thirty-eight (58.5%) patients received at least 1 cycle of neoadjuvant chemotherapy, often with the goal of starting tumor-directed therapy while radiotherapy could be planned, scheduled and initiated. Combination gemcitabine/cisplatin was the most common regimen used (n=10) for the 17 of these patients for whom chemotherapy drug data was available. The median number of neoadjuvant chemotherapy cycles was 6, for the 23 of these patients for whom chemotherapy cycle data was available. Thirty-one of the 65 (47.7%) patients receiving definitive intent treatment had at least one cycle of chemotherapy delivered concurrently with radiotherapy, with cisplatin being the most commonly used agent.
Among the 35 patients receiving palliative/salvage therapy, 27 (77.1%) received chemotherapy as part of their care, and all were prescribed EBRT with doses ranging from 30 - 50 Gy.
Outcomes
Clinical outcome data was only available for 27 patients; 22 treated with definitive intent chemoradiotherapy and 5 treated with palliative/salvage therapy. The median duration between the end of treatment and last follow-up was 12.7 months (range 0 - 15.9). Treatment-related toxicities were assessed at each patient’s last follow-up.
Late Grade 1 bladder toxicity was observed in 100% of patients for whom it was assessed (n=25). Late Grade 1 rectal toxicity was observed in 84% of assessed patients (n=21), and late Grade 2 rectal toxicity was observed in 16% of assessed patients (n=4). Two patients passed away from their disease during their EBRT treatment, and two more passed away 6 & 7 months after completion of their treatment. The longest period of time post-treatment in which all surviving patients were confirmed alive was approximately 9 months. For the 14 patients who had a follow-up period of over 1 year, 13 (93%) were still alive and disease-free.
Discussion
As of 2024, The NCC at Calmette Hospital is one of three radiation therapy centers in Cambodia, and the only center offering brachytherapy in the country. This study reviewed the presenting characteristics and treatment paradigms of the first 100 patients with cervical cancer presenting for care at the NCC in order to gain a better understanding of the population the cancer center is serving.
Previous estimates suggest 70% of cases in Cambodia present with late-stage disease [1], whereas only 35% of the first 100 patients at NCC presented with stage III/IV disease, and most commonly presented in stage IIB.
(T2bN0M0) (17%). This may be due to access disparity, as patients with more advanced disease may not have been referred for specialty care, or perhaps lacked resources to access care as the majority of patients originated from outside Phnom Penh (Table 1).
In addition to describing patient demographics, this study is the first to our knowledge to describe the complex care now available at a public hospital for patients with cervical cancer in Cambodia. Patients treated with radiotherapy received 45-50 Gy of pelvic EBRT in 1.8-2 Gy fractions, in line with the 2016 American Society of Clinical Oncology (ASCO) guidelines for management of invasive cervical cancer [6]. Additionally, patients treated with tandem and ovoid brachytherapy received a mean cumulative EQD2 HR-CTV D90 doses of 91.8 Gy, or ~69-70 Gy to Point A, depending on planning technique, in line with American Brachytherapy Society guidelines for treatment planning.
Roughly one quarter of our patients (26%) were treated with surgical therapy, 77% of whom were treated for early-stage disease. This also aligns with ASCO guidelines, which recommends reserving hysterectomy for early-stage disease and utilizing chemoradiotherapy for advanced stage disease [6]. Accordingly, extending chemoradiation capabilities is the highest priority for this hospital as 77% of its patients present beyond FIGO stage 1 (T1N0M0). Hopefully with increased screening, more cases will be detected at an earlier stage when amenable curative surgery. This approach is especially preferable for young patients as it preserves ovarian function and avoids premature menopause as well as other late gastrointestinal and genitourinary complications. A plan for developing this surgical workforce is needed, however the rate of lymph node dissections (38.5%) among patients treated with hysterectomy suggests that the NCC has existing surgical capacity to perform some of these more advanced procedures.
There were several challenges and external factors leading to prolonged treatment courses: 1) EBRT courses initiated prior to the launch of the brachytherapy program, 2) chemotherapy initiated prior to the start of radiotherapy, 3) chemotherapy or surgical care initiated at a local facility prior to referral to NCC, and 4) likely socioeconomic factors beyond what our review was able to measure. These factors also contribute to the large variability in treatment paradigms noted in this cohort. Neoadjuvant chemotherapy was administered to 38/65 (58.5%) patients treated with definitive intent. This practice is endorsed by ASCO as a means to reduce tumor burden to enable surgical therapy, and is the topic of current investigation; in this series it was more commonly prescribed prior to RT (n=33) [6]. The intent was to start cancer-directed therapy while radiotherapy could be planned, scheduled and initiated; many patients began their chemotherapy the same day as their initial consultation. NCC physicians have noted that in the time since data collection for this study has ended, they have reduced the consultation-to- RT wait time down to 2-5 days, and as such neoadjuvant chemotherapy is no longer regularly prescribed.
Importantly, at least one cycle of chemotherapy, most commonly cisplatin, was delivered concurrently with radiotherapy for 31/65 (47.7%) patients receiving definitive intent treatment, in line with ASCO guideline for concurrent chemoradiation in the treatment of stage IB to IVA cervical cancer (T1bN0M0 - T4N(ANY) M0) [6]. The combined modality rate observed in this study compares favorably to published data from other low-middle-income countries (LMIC); 9.1% in Ethiopia [7], 44.4% in India [8], and 64% in Ghana [9]. The 47.7% rate of concurrent chemoradiation observed at the NCC could be viewed as a marker of improved access to care in Cambodia, as a 2011 survey estimated that only 15% of patients in LMIC in Southeast Asia had access to an index of cancer pharmaceuticals [10].
As a catchment center for patients living outside Phnom Penh, follow-up data at the NCC was limited in this cohort, thus prohibiting a comprehensive review of outcomes. Of the 14 patients whose follow-up period exceeded 1 year, 13 (93%) were still alive and disease-free at the time of their last assessment. This provides a hopeful measure of disease control under the NCC’s current treatment protocols, however the small number of patients prohibits statistically significant conclusions. Treatment-related toxicities were assessed in all 25 patients with follow-up data available; at a median follow-up of 12.7 months, there were no Grade 3 or greater toxicities observed. While this too represents a limited dataset, the minimal toxicity observed suggests a high quality of treatment delivery and warrants further measure and follow-up.
As life expectancy in Cambodia continues to increase, so too will its burden of cancer - and accordingly, the requirement for radiation therapy. The current estimated optimal radiation therapy utilization rate in Cambodia is 42% [11]. The capability of a country to fulfill radiotherapy demand can be quantified using the radiotherapy fulfillment rate (RFR = (available fractions)/ (required fractions)); Cambodia’s RFR in 2015 ranged from 0.16-0.25 [12]. Since then, two more LINACs have been installed. Still, it has been estimated that in 2025, over 9000 patients in Cambodia will require radiotherapy, increasing to over 13,000 patients by 2035 [12]. To meet this demand, Cambodia would need between 12-20 LINACs by 2025 and between 18-28 LINACs by 2035 [12]. The NCC has two additional bunkers available to be fitted with LINACs in the near future, and the Cambodian government is currently in the process of converting the Nokor Tep Women’s Hospital in Phnom Penh into what will become the country’s largest cancer center. If this demand for LINACs is met and radiation therapy is delivered across the country in accordance with current guidelines, expected 5-year improvements in population rates of local control and survival have been estimated at 9.6% and 4.9%, respectively, compared with no radiotherapy use [13].
Perhaps unsurprisingly, a country’s RFR correlates significantly with its GDP per capita [12]. This relationship speaks to the core issue that Cambodia faces in expanding access to radiation therapy. Roughly 70% of the population is not covered by health insurance [14]. Public insurance is provided via two systems; the Health Equity Fund provides free access to healthcare for the country’s poorest, while the National Social Security Fund (NSSF) provides insurance to civil servants and formally employed workers. The ~3.1 million Cambodians under the NSSF receive 100% coverage for radiotherapy, but all others are left to either pay out of pocket or deny treatment altogether. Indeed, payment issues prevented at least three of our patients from receiving their recommended treatment.
These findings are mirrored by the sentiments of physicians at the NCC. When surveyed informally, they reported that the most pressing challenges impeding patient care at their hospital revolve around limited training and quantity of staff, as well as treatment availability issues stemming from high costs coupled with gaps in health insurance coverage.
Limitations in this study include the aforementioned difficulties obtaining outcome data, as well as the systems of recordkeeping. Currently, radiation therapy records are digitized, but other departments use paper records in Khmer, French and/or English.
The NCC of Phnom Penh has demonstrated that, with multidisciplinary partnership, complex cancer care can be delivered in a resource-constrained setting. This early sample of the first 100 patients treated for cervical cancer is an initial step towards a better understanding of Cambodia’s patient population and a snapshot of their cancer care delivery capacity. Findings presented here illustrate the challenges the NCC will face as it expands its scope and capacity to provide high quality cancer care. Looking forward, clinical outcomes need to be assessed such as locoregional control, long-term survival, and short/long-term treatment related toxicities. Establishing a cancer registry and electronic medical record will aid in this endeavor. Local and national partnership will be important to grow and support national protocols reflective of this experience.
Competing Interests
None
Funding Statement
This work was supported by Varian Medical Systems, Inc. and investigator A. Berchuck. Investigator J. Gardner received the Research Scholar Award funded by the James and Ruth Levitan Cancer Research Endowment.
Data Availability
Deidentified participant are stored in an institutional repository and will be shared upon request to the corresponding author.
Ethics Approval
Study approval was obtained from Cambodia’s National Ethics Committee for Health Research (approval #146). The committee judged that participant consent was not required due to the retrospective nature of the study.
Contributorship
SE and TS conceptualized this study and provided supervision of research activities along with AB. From the initial conceptualization, parameters of the study were refined by all authors. JG performed the bulk of the chart review and data collection with assistance from BR, PB, MM, VA, ST, and OL. PB collected all of the outcome data separately and provided it for use in this study. JG performed all statistical analyses of collected data. JG wrote the initial draft of this manuscript and all authors collaborated to finalize it. Guarantor is BR.
Acknowledgements
Special thanks to Anil Srivastava and Open Health Systems Laboratory for facilitating the funding of this research.
References
- Oncology in Cambodia Eav S., Schraub S., Dufour P., Taisant D., Ra C., Bunda P.. Oncology.2012;82(5). CrossRef
- Cambodia Gavi HPV Vaccine Demonstration Program Coverage Survey Report Chhea C, Vong W, Yong V, et al . Cambodia National Institutes of Public Health; Cambodia Ministry of Health; US Centers for Disease Control and Prevention.2018.
- Cancer Burden in Cambodia. Presented at: Cancer Registry Meeting; September 5, 2018; Calmette Hospital, Phnom Penh, Cambodia Eav S. .
- Revised FIGO staging for carcinoma of the cervix uteri Bhatla N, Berek JS , Cuello Fredes M, Denny LA , Grenman S, Karunaratne K, Kehoe ST , et al . International Journal of Gynaecology and Obstetrics: The Official Organ of the International Federation of Gynaecology and Obstetrics.2019;145(1). CrossRef
- TNM classification of malignant tumours Brierley JD , Gospodarowicz MK , Wittekind C. (Eds.) . John Wiley and Sons.2017.
- Management and Care of Women With Invasive Cervical Cancer: American Society of Clinical Oncology Resource-Stratified Clinical Practice Guideline Chuang LT Linus T., Temin S, Camacho R, Dueñas-Gonzalez A, Feldman S, Gultekin M, Gupta V, et al . Journal of Global Oncology.2016;2(5). CrossRef
- Cervical cancer in Ethiopia: survival of 1,059 patients who received oncologic therapy Kantelhardt EJ , Moelle U, Begoihn M, Addissie A, Trocchi P, Yonas B, Hezkiel P, et al . The Oncologist.2014;19(7). CrossRef
- Concurrent Chemoradiation for Cancer of the Cervix: Results of a Multi-Institutional Study From the Setting of a Developing Country (India) Nandakumar A, Kishor Rath G, Chandra Kataki A, Poonamalle Bapsy PC , Gupta PC , Gangadharan P, Mahajan RC , et al . Journal of Global Oncology.2015;1(1). CrossRef
- External Beam Radiation Therapy and Brachytherapy for Cervical Cancer: The Experience of the National Centre for Radiotherapy in Accra, Ghana Vulpe H, Asamoah FA , Maganti M, Vanderpuye V, Fyles A, Yarney J. International Journal of Radiation Oncology, Biology, Physics.2018;100(5). CrossRef
- Access to cancer medications in low- and middle-income countries Lopes GDL , Souza JA , Barrios C. Nature Reviews. Clinical Oncology.2013;10(6). CrossRef
- The Modernization of Radiation Therapy Services in Cambodia: A Model of International Collaboration Eav S, Mel M, Ath V, Shelton N, Rogl K, Newman G, Ward I, Yap ML . International Journal of Radiation Oncology, Biology, Physics.2021;111(1). CrossRef
- Estimating radiotherapy demands in South East Asia countries in 2025 and 2035 using evidence-based optimal radiotherapy fractions Yahya N, Roslan N. Asia-Pacific Journal of Clinical Oncology.2018;14(5). CrossRef
- The Benefits of Providing External Beam Radiotherapy in Low- and Middle-income Countries Yap M. L., Hanna T. P., Shafiq J., Ferlay J., Bray F., Delaney G. P., Barton M.. Clinical Oncology (Royal College of Radiologists (Great Britain)).2017;29(2). CrossRef
- Expanding social health protection in Cambodia: An assessment of the current coverage potential and gaps, and social equity considerations Kolesar RJ , Pheakdey S, Jacobs B, Chan N, Yok S, Audibert M. International Social Security Review.2020;73(1). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2024
Author Details