Targeted Oral Therapy: Utilization of Metal-Organic Frameworks
Download
Abstract
-
Intruduction
Dear Editor,
Oral cancer is considered to be sixth in rank among the major cancer types present in the world. India is the second country which has reported the highest number of oral cancer cases in the world. The current state of tobacco and alcohol consumption, along with the dental care denial, has been leading to a significant increase in the number of oral cancer cases. Oral cancer primarily affects males between the ages of 40 and 70. Earlier diagnosis and treatment of these cancers are highly recommended to increase curability chances [1, 2].
Oral Therapy
Earlier diagnosis of the cancer is essential to recognise the effective therapy for oral cancer. Oral cancer can occur in the line of lips or inside the mouth and even lead to the tongue, neck and head. Oral therapy consists of radiation therapy, chemotherapy, surgery, immunotherapy, and targeted drugs. Radiation, immunotherapy, and chemotherapy have shown several side effects, and in the case of surgery, there are chances of reoccurrence of these cells, which may follow into cancer [3]. Targeted drugs have improved treatment by reducing side effects and shortening recovery periods.
The potential of metal-organic frameworks (MOFs) in improving targeted oral therapy is a fascinating area of research. The production of hybrid nanocomposites with MOFs as a core has significantly enhanced the drug’s target acquisition. MOFs, with their excellent drug delivery capabilities, improve targeting and enhance cell uptake. Tan et al. have introduced an injectable thermosensitive hydrogel consisting of MOFs, doxorubicin, and celecoxib for oral therapy [4]. MOFs offer promise for the future of oral cancer treatment with their large pore sizes, drug encapsulation, versatility, and biodegradability. Doxorubicin and celecoxib, both effective in oral cancer, are used as an anthracycline anticancer compound [5].
Metal-Organic frameworks synthesis
MOFs are synthesized by selecting metal ions, which provide stability and biodegradability profiles. Several organic linkers, such as carboxylate-based, amino-functionalized linkers, are assisted in producing MOFs due to their strong coordination with the metal ions. Generally, the solvothermal synthesis method is followed for the production of MOFs. In this method, the metal ions and organic linkers self-assemble under high pressure and temperature. MOFs can enhance functionality through organic linker modifications, surface functionalization with polymers, or other guest molecules [6, 7].
Anticancer drugs are loaded into the porous structures of the MOFs through several methods, including impregnation, encapsulation, and covalent conjugation. In impregnation, drugs are trapped in the pores of MOF and excess drugs are removed with solvents. Encapsulation the drug is encapsulated within the framework during the production of MOF synthesis. The drugs are covalently attached to the organic linkers or functional groups within the MOF structures [8]. The MOFs with the drug are analyzed with X-ray diffraction, surface area analysis, and spectroscopic methods for their structure and drug loading capacity. The therapeutic efficacy, cellular uptake, and cytotoxicity of MOFs have been studied in vitro and in vivo.
Drug delivery
MOF has been found to possess high surface area and porosity, which helps carry the drug through the pores or by encapsulation. MOF’s unique structure enables controlled drug release at specific sites using various moieties, including antibodies, peptides, and small molecules [9]. The crystalline structure of MOF provides enhanced stability, which provides a longer shelf-life to the drug.
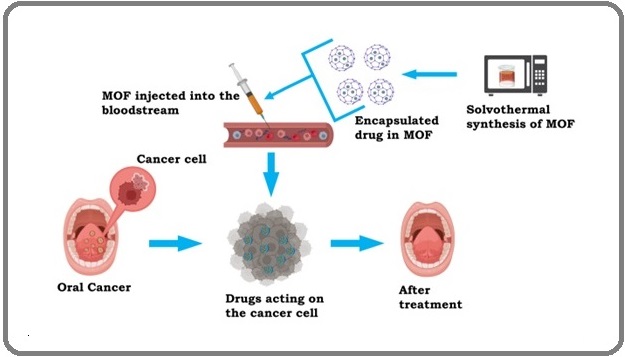
A single MOF can carry multiple therapeutic agents simultaneously, which helps deliver several drugs and imaging agents simultaneously. This multimodel MOF has shown a significant increase in therapeutic ability efficiency and aids in regulating drug release in real-time. The hydrophobic drug Dox was encapsulated in FeAu@ MIL-100. This encapsulated drug in the MOF has been utilized for imaging and cancer theranostics. These MOF has shown an efficiency in Dox release and encapsulation of 97.19%. FeAu@MOF in an invivo mouse model has shown enhanced imaging, and decreased tumor growth, and its volume. This has shown that this MOF with the ablity to enhance the survival and a potential for treatment of oral cavity cancer. MOF coated with dental mesenchymal stem cells (DPSC) with a CXCR2 which has helped in the reduction of Oral squamous cell carcinoma growth rate. This MOF induce apoptosis rate of 22.97% in CAL27 cells [7]. Linkers with biocompatible metals can help MOFs degrade slowly, releasing drugs over time and reducing drug buildup in the body [10]. Figure 1 depicts the synthesis of MOF with encapsulated drug and their action mechanism on the cancer cell.
Figure 1. Synthesis of MOF with Encapsulated Drug and Their Action Mechanism on the Cancer Cell is Depicted.
The large surface area and the pore volume of MOF has helped in encapsulating high concentration of drug molecules. The encapsulated drugs are released to the specific site with the help of change in pH, temperature, or specific protein. The inclusion of targeting moieties helps in the selective binding to target cells and reduces unwanted action of drugs at certain locations in the organism. Only a few has been viewed or analyzed for their biocompatibility. MIL-100 (Fe) is well known for its ability in biomedical sectors, drug delivery, and therapeutic ability. MIL-100 (Fe) abilities has been used against several cell lines such as cervical cancer lines, lung cancer lines, etc which has shown inhibition and decrease of cell viability to 67% and 45%. MIL-101 or MIL-88B, with an adequate amount, is impactful in inhibiting tumour angiogenesis in several mammals. These MOFs have also been effective in the selective inhibition of growth in certain cancer cells or tumour cells within 12 hrs when compared to the traditional tyrosine kinase inhibitor. With the current studies, the treatment of MOF is limited to in vivo experiments on mammals. These experiments were successful in laboratories and small animals, but human trials are further away as these results can vary, leading to unsuccessful trials [11].
Limitations and Future Perspectives
Despite several advantages of MOF’s ability to target deliver the drug, it is found to cause cell toxicity when seen in a certain amount to the cell. The stability of MOF in the biological environment depends on the bonds of the MOF such as metal-ligand bonds. These are influenced by pH, ionic strength, and other molecules. The mechanical stability along with the thermal stability should be maintained during the production of MOF. The degradation of MOF can be done by hydrolysis, and certain enzymes which helps in degradation of the MOF into simpler parts for easier transportation to excretion. Biomagnification can lead to improper blood circulation and several other cytotoxic effects. The physicochemical properties of the MOF are also principal determinants for the measurement of MOF toxicity. The effects of factors such as the chemistry of precursors, zeta potential, morphology and particle size. The overall toxicity of the MOF is determined by analyzing the impact of metals used for its production. The particle size of the MOF is inversely proportional to the toxic nature of the MOF. The decrease in size of MOF increases the toxic nature of the MOF. The shape, number of pore size, etc of MOF are found to be the ones which are affecting the toxicity. The Zeta potential of the MOF has been found effective in assessing and detecting the toxicity of MOF. The work on non-toxic MOF is moving through several phases, with modifications for increased functionality. The study of strategies for toxicity reduction includes green chemistry and surface modification. Altering of MOF chemistry with the introduction of green ligands, linkers, and solvents is a potential strategy to mitigate toxicity. The usage of green components contributes to the reduction of toxicity to a certain point of extent. Coating the MOF with several biomolecules has been found effective in controlling the level of MOF toxicity. The coating used for this includes lipids, chitosan, leaf extracts, etc, which has helped lower the MOF’s toxicity without any reduction in its activity [12]. The introduction of controlled biodegradation to the MOF is still being studied to decrease the side effects. Although MOFs offer advantages in drug delivery and controlled release, further research is needed to enhance their targeting efficiency. The effectiveness of the MOF can be varied with the change in each individual. Genetic information held in each individual can affect the distribution of drug carried by the MOF. To overcome this, the drug dosage should be screened according to the patient’s genetic profile. Age related changes, immune changes, and medical history should be considered before producing targeted MOF drug production. Psychological factors such as anxiety, depression, etc can also impact the effectiveness of therapies. Along these, the cost-effectiveness of the large-scale production of MOF is to be considered for a better economic society. The recovery of unreacted raw materials has increased with the increase in technology in the production facilities. This has contributed significantly to the production of MOF by lowering the cost per unit from 13.9 $/Kg to 13.2 $/Kg. Even this low impact on the price when considering the higher scale production will further decrease the production cost. In summary, introducing cost-effective production of these MOFs with non-toxic material can revolutionize the therapeutic world. The pre-clinical research, clinical trials, regulatory filings, and post-marketing surveillance are all part of an extensive procedure which goes into obtaining permission for MOF-based treatment. The detailed approach and attention to the regulation established by certain health authorities. This helps in the regulation of drug usage and improves the safety of humans before releasing it. These regulations helps in the successful commercialization of MOF-based medicines with the help of several health authorities throughout the development phase.
Declaration of competing interest
The authors declare no competing financial interest in the work reported.
References
- Oral cancer diagnosis and perspectives in India Borse V, Konwar AN , Buragohain P. Sensors International.2020;1. CrossRef
- Oral cancer in India, a growing problem: Is limiting the exposure to avoidable risk factors the only way to reduce the disease burden? Subash A, Bylapudi B, Thakur S, Rao V. Oral Oncology.2022;125. CrossRef
- Emerging targeted therapies in oral oncology: Focus on EGFR inhibition Veeraraghavan VP , Daniel S, Dasari AK , Aileni KR , Patil C, Patil SR . 2024;11. CrossRef
- A multifunctional MOF-based nanohybrid as injectable implant platform for drug synergistic oral cancer therapy Tan G, Zhong Y, Yang L, Jiang Y, Liu J, Ren F. Chemical Engineering Journal.2020;390. CrossRef
- Current Trends of Targeted Drug Delivery for Oral Cancer Therapy Zhang M, Liang J, Yang Y, Liang H, Jia H, Li D. Frontiers in Bioengineering and Biotechnology.2020;8. CrossRef
- Modification of Metal-Organic Framework Nanoparticles Using Dental Pulp Mesenchymal Stem Cell Membranes to Target Oral Squamous Cell Carcinoma Zhou D, Chen Y, Bu W, Meng L, Wang C, Jin N, Chen Y, Ren C, Zhang K, Sun H. Journal of Colloid and Interface Science.2021;601. CrossRef
- Innovative Metal-Organic Frameworks for Targeted Oral Cancer Therapy: A Review Mousavi SM , Hashemi SA , Fallahi Nezhad F, Binazadeh M, Dehdashtijahromi M, Omidifar N, Ghahramani Y, Lai CW , Chiang W, Gholami A. Materials (Basel, Switzerland).2023;16(13). CrossRef
- Synthesis of hollow nanocages MOF-5 as drug delivery vehicle to solve the load-bearing problem of insoluble antitumor drug oleanolic acid (OA) Zhang L, Chen Y, Shi R, Kang T, Pang G, Wang B, Zhao Y, et al . Inorganic Chemistry Communications.2018;96. CrossRef
- Metal-Organic Framework Nanocarriers for Drug Delivery in Biomedical Applications Sun Y, Zheng L, Yang Y, Qian X, Fu T, Li X, Yang Z, et al . Nano-Micro Letters.2020;12(1). CrossRef
- Application of MOF materials as drug delivery systems for cancer therapy and dermal treatment Mallakpour S, Nikkhoo E, Hussain CM . Coordination Chemistry Reviews.2022;451. CrossRef
- Functional MOF-Based Materials for Environmental and Biomedical Applications: A Critical Review Gatou M, Vagena I, Lagopati N, Pippa N, Gazouli M, Pavlatou EA . Nanomaterials (Basel, Switzerland).2023;13(15). CrossRef
- Mitigating Metal-organic framework (MOF) toxicity for biomedical applications Wiśniewska Pa, Haponiuk J, Saeb M, Rabiee N, Bencherif S. Chemical Engineering Journal.2023;471. CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2024
Author Details