Diagnostic Accuracy of Tumor Imprint Cytology for Ovarian Cancer
Download
Abstract
Background: Due to the lack of ovarian cancer screening tools, the combination of clinical findings, serum tumor markers, imaging, and tumor imprint cytology have been studied with the intention of treating the disease. Thus the aim is to determine the diagnostic accuracy of tumor cytology.
Methods: Cross-sectional prospective study carried out on surgically treated ovarian tumors. The participants enrolled from the routine surgery list of the Gynecology Department from August 2022 to June 2024. An intraoperative tumor cytology test was done and compared with the final histopathology report. Descriptive statistics were used and diagnostic accuracy was calculated.
Results: Out of 82 ovarian tumor surgeries one-third were histopathologically proven malignant tumors and the rest were benign conditions. The most common cancers were of epithelial origin followed by stromal and germ cell origin. The diagnostic accuracy of tumor cytology was 80.5% and two-thirds of cancers were correctly detected. Tumor markers could not consistently guide to characterize the tumor's nature.
Conclusion: All malignant tumors had elevated tumor markers but were not exclusive. Tumor cytology together with imaging and tumor markers could help decide the extent of surgery.
Introduction
Ovarian cancer is the second most common genital tract cancer in women next to the uterine cervix, Diagnosis is easier for the uterine cervix as it can be visualized and examined in an outdoor clinical setup and due to the availability of a proven screening method as well. Because of the anatomical location of the ovary, it is not detected early unless it becomes symptomatic or incidentally found on imaging tests. There will be a high degree of suspicion from clinical examination, imaging, and tumor markers. However, an effective screening test has not been developed yet [1, 2].
With all available diagnostic tests, it can only be predicted unless a cell or tissue is obtained for the pathological test like tumor cytology or frozen section biopsy during surgery [3, 4].
It can be utilized for deciding the extent of surgery.
Tumor cytology could be an imprint cytology or scrape cytology. However, tumor FNAC appears better than the tumor fluid cytology [5-9]. Frozen section biopsy facilities are not available in many centers limited by equipment and trained human resources. In the center where a pathologist or cytopathologist is available to instantly report tumor cytology to synchronize the surgical procedure, intra-operative tumor cytology would be the viable solution for onco-surgery. Thus, this study would fill the resource gap in addressing ovarian cancer surgery. If the cancer is diagnosed early in the first stage, the 5-year survival is 92% and in advanced stages, the overall survival is reduced to 29% only indicating the need for good predicting tools [2, 10].
Materials and Methods
A diagnostic analytical study was performed on the surgically treated ovarian tumors from August 2022 to June 2024 at Nobel Medical College Teaching Hospital, Biratnagar, Nepal. All the consecutive cases indicated and listed for the surgery were taken in research with the intention of treating the disease. Ovarian tumors were clinically evaluated by clinical examination, imaging study, tumor marker assay, and intra-operatively by tumor cytology. Complex tumor morphology, clinically suspected ovarian mass, and abnormal serum tumor markers were the inclusion criteria to include in the surgery list. The surgical procedure was followed uniformly as recommended by the updated NCCN (National Comprehensive Cancer Network) Clinical Practice Guideline along with tumor imprint-cytology [11].
Ovarian tumor surfaces or incised surfaces were scraped by a surgical knife and smeared over the glass slides – one dipped into the 95% ethyl alcohol and another slide as an air-dried smear for the Pap stain and Giemsa stain respectively. The tumor cytology report was received within 20-25 minutes and guided for the further surgical procedure. However, intraoperatively suspected cancer proceeded for complete staging surgery irrespective of the tumor cytology report. The histopathology examination report was taken as the confirmatory test received after a week. The diagnostic accuracy of tumor cytology and tumor markers in terms of sensitivity, specificity, diagnostic accuracy, and false positive and false negative rates were calculated. Descriptive statistics by frequency and percentage of cancer attributes were calculated and displayed in graphics. The Institutional Review Committee approved the study.
Results
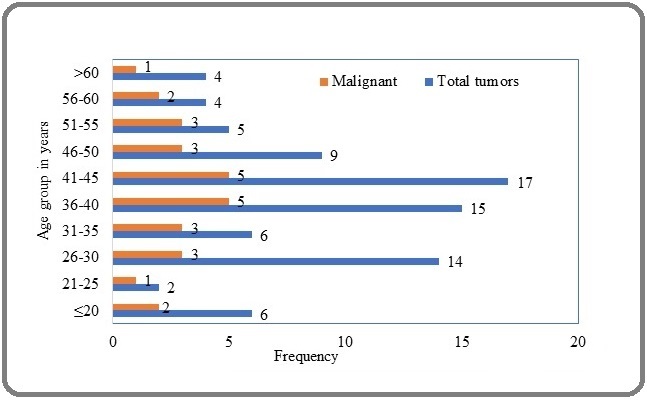
Out of 82 ovarian tumor surgery cases enrolled in the study, three-fourths (74.4%) were between 26 and 50 years of age with a median age of 40 years ranging from 8 to 78 years. Likewise, two-thirds (19 out of 28) of malignant cases fell under the 26-50 years age group (Figure 1).
Figure 1. Ovarian Tumor Distribution by Age Group.
Out of 82 ovarian tumor surgeries enrolled in the study, 28 (One-Third) were proven malignant by final histopathological examination. Epithelial origin of cancer was the most common (3/4th) followed by stromal and germ cell origin. The rest of the tumors were benign like cystadenoma, endometrioma, teratoma, and fibroma (Table 1).
| Tissue of origin | Types of neoplasm | Frequency (n=28) | Tumor Cytology Negative (n=9) |
| Epithelial (21) | Serous | 10 | 1 |
| Mucinous | 9 | 4 | |
| Endometrioid | 2 | ||
| Stromal (4) | Granulosa | 2 | 1 |
| Sertoli-Leidig | 1 | 2 | |
| Steroid cell | 1 | 0 | |
| Germ cell (3) | Yolk sac | 2 | 0 |
| Squamous (Teratoma) | 1 | 1 |
Forty-five had a complex type of adnexal tumor in imaging with 100% sensitivity but poor specificity.
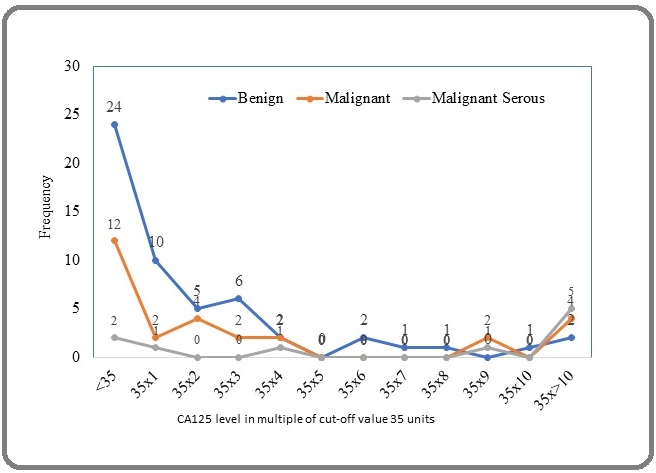
Seven out of ten serous cystadenocarcinoma had raised CA125 and more than half of the benign tumors (55.5%, 30 out of 54) had raised value as well. Serum CA125 level has not differentiated the benign or malignant nature of the tumor in any multiple of its value in blood as a tumor marker considering 35 units as the cut-off. Diagnostic accuracy (51.2%), sensitivity (60.7%), and specificity (46.3%) of CA125 alone to predict malignancy are low. Even in the mucinous type of ovarian cancers, only one-third had raised tumor marker CEA; not correlating with the tumor nature. However, Yolk sac tumors were correctly identified by the tumor marker, alfa-feto-protein in both cases (Figure 2).
Figure 2. Distribution of Benign and Malignant Tumors by CA125 Level (Benign=54, Malignant=28 with 10 serous type).
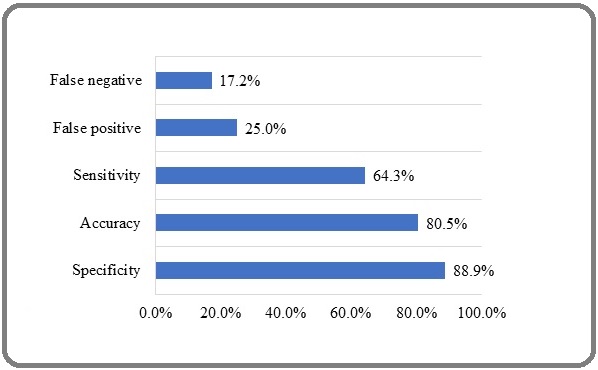
The diagnostic accuracy of imprint tumor cytology was 80.5%. Two-thirds of ovarian cancers were correctly identified by intra-operative tumor cytology. Three cases of endometriosis out of 13 had positive cytology reports due to reactive changes like increased nuclear-cytoplasmic volume, mild pleomorphism, and prominent nucleoli. Thus, 77% of endometriosis was correctly diagnosed in tumor cytology. If endometriosis was excluded, the diagnostic accuracy reached 83.5% and around 16% of false positive or false negative rates (Figure 3).
Figure 3. Accuracy Parameters of Tumor Imprint Cytology to Predict Ovarian Malignancy.
Positive tumor cytology with an elevation of any tumor marker detects more malignancy (50%; 14 out of 28) than the positive tumor cytology with elevated CA125 (39.3%; 11 out of 28). It shows a 1.3 times higher detection rate while doing all three tumor markers (CA125, CEA, and AFP) (Tables 2 and 3).
| Tumor cytology | Tumor markers | Malignant | Benign | Total |
| Positive | High | 14 | 5 | 19 |
| Normal | 4 | 1 | 5 | |
| Negative | High | 7 | 26 | 33 |
| Normal | 3 | 22 | 25 | |
| Total | 28 | 54 | 82 |
| Tumor cytology | CA125 | Malignant | Benign | Total |
| Positive | High | 11 | 4 | 15 |
| Normal | 7 | 2 | 9 | |
| Negative | High | 6 | 23 | 29 |
| Normal | 4 | 25 | 29 | |
| Total | 28 | 54 | 82 |
Few selected cases (n=7; 8.5%) underwent uterine conservative surgery for future fertility. Ovarian cancer of the high-grade category, more than stage 1, and with cytology-positive peritoneal fluid received adjuvant chemotherapy from the centers of patients’ choice, and the rest of the cancers and endometriomas were kept on follow-up.
Discussion
The median age of 40 concerns the productive life that needs public health intervention besides clinical management. Epidemiological factors like reproductive, hormonal, behavioral, and genetic conditions would be the areas to focus on. Epithelial ovarian cancers are the most common ovarian cancers by 3/4th in bulk like in Reid BM et al where more than 90% were reported as the epithelial origin in developing countries [10, 12, 13]. That’s why epithelial cell markers like CA125 are used to screen ovarian tumors despite its borderline accuracy of 51.2% in this study. The combination of tumor markers increases the diagnostic accuracy by 1.3 times to include other types of tumors as well [1, 14, 15].
Non-malignant conditions like endometriosis mimics ovarian cancer in its clinical presentation like ovarian mass and raised CA125. Its diagnostic accuracy to predict endometriosis is high if other conditions are excluded in the symptomatic patients. Vise versa is true by increased diagnostic accuracy of 83.5% in this study to predict ovarian cancer once endometriosis was excluded [16]. Endometriosis is also considered as a potential for the development of ovarian cancer due to its estrogen-primed condition requiring intervention like cancer [17].
A combination of imaging findings, CA125, and menstrual status further increases the predictability like in the Risk of Malignancy Index [18]. Even the frozen section biopsy interpretation requires clinical parameters to come to a conclusion [19].
These are the indirect ways of predicting ovarian cancer without surgical intervention. Once the point of care intervention is required for the cancer victims, a definite means of cancer prediction is required like cell or tissue diagnosis. Tumor cytology or frozen section biopsy during surgery would help to decide the extent of surgical treatment as a single setting intervention. The diagnostic accuracy of imprint cytology in this study is over 80% obtained during surgery. Though the frozen section biopsy has more diagnostic accuracy, tumor cytology also has a supplementary role to it. Thus, this cost-effective test would be the better option where there is no frozen section facility [3].
The diagnostic accuracy of imprint cytology was found promising in two centers in Nepal and India which may represent the applicability in developing countries [3, 9, 20].
Thus, the diagnostic accuracy of tumor imprint cytology is 80.5%. Together with three tumor markers (CA125, CEA, and AFP) have a 1.3 times higher detection rate of ovarian malignancy than the CA125 only. Combining all three parameters such as serum tumor markers, imaging, and tumor imprint cytology yields a better predictivity rate for ovarian cancer.
Acknowledgments
Sincere thanks to the post-graduate residents for assisting me while performing surgery and maintaining data.
Funding statement
There is no funding source.
Approval
Ethical approval taken from the Nepal Health Research Council.
Conflict of interest
There is no competing interest from the author and co-authors.
Author contribution
Principal author contributed from conceptualization to the final manuscript preparation. Co-authors had contributed in review of manuscript.
References
- Ovarian cancer: screening and future directions Gupta KK , Gupta VK , Naumann RW . International Journal of Gynecological Cancer: Official Journal of the International Gynecological Cancer Society.2019;29(1). CrossRef
- Current and Emerging Methods for Ovarian Cancer Screening and Diagnostics: A Comprehensive Review Liberto JM , Chen S, Shih I, Wang T, Wang T, Pisanic TR . Cancers.2022;14(12). CrossRef
- Value of cytology in the intraoperative assessment of ovarian tumors: a review of 402 cases and comparison with frozen section diagnosis Stewart CJR , Brennan BA , Koay E, Naran A, Ruba S. Cancer Cytopathology.2010;118(3). CrossRef
- The accuracy of frozen section diagnosis of ovarian tumors Twaalfhoven F. C. M., Peters A. A. W., Trimbos J. B., Hermans J., Fleuren G. J.. Gynecologic Oncology.1991;41(3). CrossRef
- Intraoperative Cytology of Ovarian Neoplasms with an Attempt to Grade Epithelial Tumors Bohara S, Jain S, Khurana N, Shangpliang DM , Agarwal S, Gandhi G. Journal of Cytology.2018;35(1). CrossRef
- Neoplastic and nonneoplastic ovarian masses: Diagnosis on cytology Khan N, Afroz N, Aqil B, Khan T, Ahmad I. Journal of Cytology.2009;26(4). CrossRef
- Cytologic examination of ovarian cyst fluid for the distinction between benign and malignant tumors Moran O., Menczer J., Ben-Baruch G., Lipitz S., Goor E.. Obstetrics and Gynecology.1993;82(3).
- Contribution of intraoperative cytology to the diagnosis of ovarian lesions Alvarez Santín C, Sica A, Melesi S, Feijó A, Garrido G, Rodríguez Alvarez C. Acta Cytologica.2011;55(1). CrossRef
- Evaluating intraoperative cytology with histopathology diagnosis and its importance in ovarian tumors Vaidya K, Shrestha B, Jha R, Shrestha B, Rajbhandari A, Joshi R, Subedi K. Journal of Pathology of Nepal.2020;10. CrossRef
- Epidemiology of ovarian cancer: a review Reid BM , Permuth JB , Sellers TA . Cancer Biology & Medicine.2017;14(1). CrossRef
- NCCN Clinical Practice Guidelines in Oncology. Treatment by Cancer Type. 2024. https://www.nccn.org/guidelines/category_1 .
- Distribution of various histopathological types of ovarian tumors: A study of 212 cases from a tertiary care center of Eastern Uttar Pradesh Gupta N, Yadav M, Gupta V, Chaudhary D, Patne SCU . Journal of Laboratory Physicians.2019;11(1). CrossRef
- Study of histopathological spectrum of ovarian lesions Patel K, Parmar R, Patel J, Sharma B, Patel B, Patel N. IP Archives of Cytology and Histopathology Research.2021;6. CrossRef
- CA125 and Ovarian Cancer: A Comprehensive Review Charkhchi P, Cybulski C, Gronwald J, Wong FC , Narod SA , Akbari MR . Cancers.2020;12(12). CrossRef
- Future Screening Prospects for Ovarian Cancer Žilovič D, Čiurlienė R, Sabaliauskaitė R, Jarmalaitė S. Cancers.2021;13(15). CrossRef
- Diagnostic accuracy of Cancer Antigen 125 (CA125) for endometriosis in symptomatic women: A multi-center study Hirsch M, Duffy JMN , Deguara CS , Davis CJ , Khan KS . European Journal of Obstetrics, Gynecology, and Reproductive Biology.2017;210. CrossRef
- Endometriosis and Ovarian Cancer: an Integrative Review (Endometriosis and Ovarian Cancer) Brilhante AVM , Augusto KL , Portela MC , Sucupira LCG , Oliveira LAF , Pouchaim AJMV , Nóbrega LRM , Magalhães TF , Sobreira LRP . Asian Pacific journal of cancer prevention: APJCP.2017;18(1). CrossRef
- Diagnostic Accuracy of Risk of Malignancy Indices in Ovarian Tumor Baral G, Joshi R, Pandit B. Journal of Nepal Health Research Council.2020;18(2). CrossRef
- Frozen Section Diagnosis of Ovarian Epithelial Tumors: Diagnostic Pearls and Pitfalls Buza N. Archives of Pathology & Laboratory Medicine.2019;143(1). CrossRef
- Intraoperative Cytological Diagnosis of Ovarian Cancer Rady HA , Mohammed NE , Farag M. Indian Journal of Gynecologic Oncology.2019;17(2). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2024
Author Details