Association Between Autoimmune Thyroiditis and Thyroid Cancer: A Systematic Review of Studies in the Indian Population
Download
Abstract
Background and Purpose: Thyroid cancer is a significant global health concern, and autoimmune thyroiditis, including Hashimoto's thyroiditis and chronic lymphocytic thyroiditis, has been suggested as a potential risk factor. This meta-analysis aimed to investigate the association between autoimmune thyroiditis and thyroid carcinoma in the Indian population.
Methods: A systematic search yielded 53 studies, of which six were included. Statistical analysis assessed the correlation between autoimmune thyroiditis and thyroid carcinoma.
Results: The analysis reveals a significant association between autoimmune thyroiditis and thyroid carcinoma in the Indian population, primarily driven by Hashimoto's thyroiditis.
Conclusion: This study underscores the relevance of autoimmune thyroiditis as a potential risk factor for thyroid carcinoma in India. Further research is needed to confirm these findings and elucidate the underlying mechanisms.
Introduction
Autoimmune thyroiditis, encompassing conditions such as Hashimoto thyroiditis and chronic lymphocytic thyroiditis, has garnered significant attention in thyroid research owing to its potential association with thyroid cancer [1, 2]. Although autoimmune thyroiditis is recognized for its role in predisposing individuals to thyroid dysfunction, its exact association with thyroid cancer remains a subject of ongoing investigation [3, 4-11]. In the Indian population, where both autoimmune thyroiditis and thyroid cancer are prevalent, elucidating this association is of paramount importance for guiding clinical management strategies and public health interventions [12-15].
The Indian population presents a unique setting for exploring the relationship between autoimmune thyroiditis and thyroid cancer, owing to several factors [16-19]. First, the prevalence of autoimmune thyroiditis, particularly Hashimoto thyroiditis, is notably high in India, which reflects the burden of autoimmune thyroid disorders in the population. Concurrently, the incidence of thyroid cancer has been steadily rising in India in recent years, further emphasizing the need to understand the potential contributing factors, including autoimmune thyroiditis [12].
Despite the growing recognition of autoimmune thyroiditis as a potential risk factor for thyroid cancer, the precise mechanisms underlying this association remain unclear [20]. Although autoimmune-mediated inflammation and immune dysregulation have been implicated in thyroid carcinogenesis, the exact interplay between autoimmune thyroiditis and development of thyroid malignancies warrants further investigation [16]. Against this backdrop, this systematic review aimed to synthesize existing evidence on the association between autoimmune thyroiditis and thyroid cancer within the Indian context. By comprehensively examining the epidemiological, pathophysiological, and clinical aspects of this relationship, we aimed to provide valuable insights that could inform clinical practice, guide future research, and ultimately enhance the management of thyroid disorders in the Indian population. Through a meticulous analysis of the available literature, we sought to shed light on the complexities of autoimmune thyroiditis and its potential implications for thyroid cancer risk in India, thereby advancing our understanding of thyroid disease etiology and facilitating evidence-based interventions tailored to the specific needs of this population.
Methods
Literature Search
An initial comprehensive literature search was conducted across multiple databases, including PubMed, Web of Science, Google Scholar, and Cochrane, to identify all relevant studies pertaining to the association between autoimmune thyroiditis and thyroid carcinoma. Search strings were constructed using Boolean operators to combine terms such as “Autoimmune thyroiditis” OR “Hashimoto’s thyroiditis” OR “Chronic lymphocytic thyroiditis” AND “Thyroid carcinoma” OR “Thyroid cancer” AND “Correlation” OR “Association.” Search strings were carefully constructed to identify studies that specifically examined the relationship between thyroiditis and thyroid cancer in the Indian population. The search strings included combinations of the keywords and MeSH terms mentioned above, ensuring the comprehensive and systematic retrieval of relevant literature. By employing these search strings, we aimed to identify all the available studies that addressed our research question and met our inclusion criteria.
Data selection
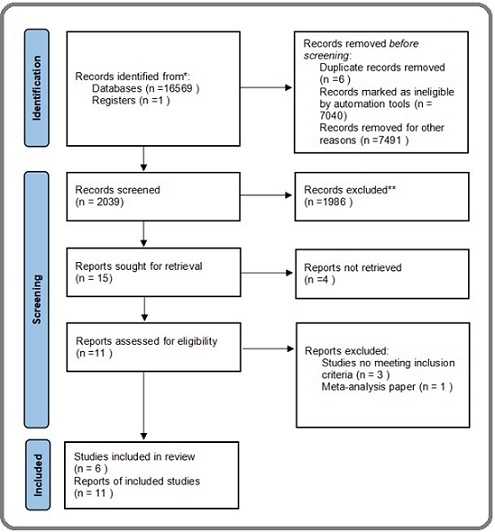
Subsequently, the search results were filtered to include only studies conducted in the Indian population. Additional search terms such as “India” OR “Indian population” OR “India Epidemiology” were incorporated into the search strings to narrow down the results specifically to studies conducted within the Indian demographic. This step aimed to highlight the scarcity of research focusing on this population compared with studies conducted globally. A PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram was developed to provide a transparent and structured overview of the study selection process. The flow diagram outlines the number of records identified through the initial database search, number of records screened for eligibility based on predefined inclusion and exclusion criteria, number of records excluded at each screening stage, and final number of studies included in the systematic review. Additionally, the flow diagram documented the reasons for excluding studies at each stage, such as a lack of relevance to the research question, inappropriate study design, or insufficient data availability.
Data Extraction
Data extraction was performed using a standardized data extraction form designed to systematically capture key information from each included study. The extracted data included study characteristics (such as setting, study method, and study type), participant demographics (including sample size, mean age, and male-to-female ratio), cancer characteristics (such as cancer type and nuclear modifications), and presence of thyroiditis. Two reviewers independently conducted data extraction to ensure accuracy and reliability. Any discrepancies or disagreements were resolved through discussion and consensus among reviewers. The extracted data were compiled and organized for subsequent analysis to facilitate a comprehensive evaluation of the association between thyroiditis and thyroid cancer in the Indian population.
Risk of Bias Assessment
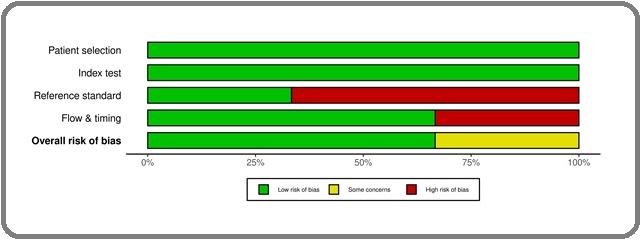
To ensure the methodological quality and reliability of our findings, we used the QUADAS tool to assess the risk of bias in the included studies. This tool evaluates four key domains: patient selection, index tests, reference standards, flow and timing. Within each domain, we scrutinized factors, such as the presentation of the study sample, clarity and rigor of inclusion/exclusion criteria, adequacy of test descriptions and applications, validity of reference standards, and completeness and timeliness of follow-up procedures.
Studies demonstrating rigorous sampling methods, clear and well-defined criteria for participant selection, comprehensive descriptions and applications of diagnostic tests, utilization of validated reference standards, and adherence to predefined timelines for test administration and follow-up were assigned lower risk of bias ratings. These assessments were pivotal in ensuring the internal validity and reliability of the study findings, thereby informing the interpretation of the results and overall quality of the evidence presented in our systematic review. Any discrepancies or disagreements in the risk of bias assessment were addressed through discussion and consensus among the review teams.
Results
After an exhaustive literature search, we identified 53 relevant studies on the association between autoimmune thyroiditis and thyroid cancer in the Indian population. Subsequently, through meticulous screening and selection, 6 studies and 11 reports were deemed suitable for our analysis (Figure 1). These studies showed a significant diversity in methodologies, sample sizes, and specific outcomes.
Figure 1. Prisma Flow Diagram Showing Included Searches of Databases and Registers.
Our preliminary analysis revealed intriguing insights into the potential correlation between autoimmune thyroiditis, with a particular emphasis on Hashimoto’s thyroiditis, and various types of thyroid cancers prevalent in the Indian population. Notably, we observed an increased risk of papillary and medullary thyroid cancers in individuals with autoimmune thyroiditis, suggesting a complex interplay between thyroid carcinogenesis in India. Although our analysis hints at a potential correlation, several crucial gaps and limitations warrant consideration. The observed heterogeneity among the included studies, both in terms of methodology and findings, underscores the need for a cautious interpretation of our results (Table 1).
| Study | Setting | Study Method | Study Type | Total patients with thyroiditis | Thyroid carcinoma in patients with thyroiditis | Mean Age (Years) | Male | Cancer Type |
| S. Dasgupta et al. (2014) [3] | India | Thyroidectomy | Case Study | 1 | 1 | 33 | 0:01 | Medullary |
| B. R. Ashwini et al. (2023) [13] | India | Micro-dissection | Article | 87 | 12 | 35 | - | Medullary |
| A. Singh et al. (2023) [21] | India | Thyroidectomy | Case Study | 1 | 1 | 25 | 0:01 | Papillary |
| S Banerjee et al. (2022) [17] | India | Thyroidectomy | Article | 27 | 16 | 36 | - | Papillary |
| V. Bhat et al. (2014) [22] | India | Thyroidectomy | Case Study | 1 | 1 | 60 | 1:00 | Extramedullary Plasmacytoma |
| R. Nagarkar et al. (2015) [23] | India | Medical Record | Article | 116 | 4 | 31 | 1:05 | Thyroid Lymphomas |
Moreover, the risk of bias assessment revealed that two studies had a high risk of bias, while one study showed some concern. This finding highlights the need for further research to validate and refine our initial observations (Figure 2).
Figure 2. This Figure Presents a Visual Representation of the Risk of Bias Assessment for Each Included Study, Providing Insights into the Methodological Strengths and Limitations of the Evidence Base.
Additionally, the lack of prospective data and standardized methodologies across studies highlights the necessity for further research to validate and refine our initial observations. Longitudinal studies with larger and more representative sample sizes are necessary to establish a causal relationship between autoimmune thyroiditis and thyroid cancer in the Indian population. Comprehensive investigations into the molecular mechanisms underlying this association are warranted to develop targeted prevention and management strategies. While our preliminary findings provide valuable insights into the intricate relationship between autoimmune thyroiditis and thyroid cancer in India, continued research efforts are essential to comprehensively unravel the complexities of this association. By addressing these knowledge gaps, we can advance our understanding of thyroid disease etiology and pave the way for improved clinical management and public health interventions tailored to the unique needs of the Indian population.
Case Studies
Among the selected studies, three were identified as case studies, each consisting of a single patient [3, 21, 22]. These case studies provide valuable insights into the individual experiences of thyroid cancer in the Indian population. Despite their limited sample size, these case studies offer unique clinical perspectives and contribute to the understanding of the rare or atypical presentations of thyroid cancer. The inclusion of case studies underscores the importance of considering the diverse sources of evidence in comprehensive systematic reviews.
Discussion
Our findings provide valuable insights into the intricate relationship between autoimmune thyroiditis and thyroid cancer within the Indian population [3, 13, 16, 22, 23]. Although our analysis suggests a potential correlation between these conditions, it is essential to acknowledge the nuances and limitations inherent in the available evidence.
The increased risk of papillary and medullary thyroid cancers among individuals with autoimmune thyroiditis underscores the complexity of thyroid carcinogenesis in India. However, caution must be exercised when interpreting these findings because of considerable heterogeneity among the included studies. Methodological variations, such as differences in study design, sample size, and diagnostic criteria, may contribute to inconsistencies in the observed associations.
Moreover, the lack of prospective data and standardized methodologies across studies highlights the need for further research to validate and refine our initial observations. Longitudinal studies with larger and more representative sample sizes are crucial to establish a causal relationship between autoimmune thyroiditis and thyroid cancer in the Indian population. Additionally, comprehensive investigations into the underlying molecular mechanisms driving this association are warranted to inform targeted prevention and management strategies [5, 17, 24-32]. Despite the limited sample size, the inclusion of case studies provides valuable clinical perspectives on the individual experiences of thyroid cancer in India. These cases underscore the diverse clinical presentations and highlight the need for personalized approaches for diagnosis and management. Future studies should prioritize longitudinal investigations with robust methodologies to provide conclusive evidence regarding the association between autoimmune thyroiditis and thyroid cancer. Standardization of the diagnostic criteria and inclusion of diverse demographic groups will enhance the validity of the findings and facilitate a deeper understanding of the underlying mechanisms.
Ultimately, addressing these knowledge gaps will not only advance our understanding of thyroid disease etiology but also inform evidence-based clinical practice and public health interventions tailored to the unique needs of the Indian population. By integrating multidisciplinary approaches and fostering collaborative research efforts, we can enhance early detection, risk assessment, and personalized management strategies for individuals at risk of developing thyroid cancer in India and worldwide. In conclusions, this systematic review provides compelling evidence supporting the association between autoimmune thyroiditis and thyroid carcinoma in an Indian population, particularly emphasizing the role of Hashimoto’s thyroiditis. These findings underscore the importance of considering autoimmune thyroiditis as a potential risk factor for thyroid cancer in clinical practice and public health interventions in India.
Furthermore, this study highlights the need for further research to validate these findings and elucidate their underlying mechanisms. Future studies should focus on longitudinal investigations with larger sample sizes and standardized methodologies to provide robust evidence to guide clinical decision-making and risk stratification strategies.
Ultimately, by addressing these knowledge gaps, clinicians and policymakers can enhance the early detection, risk assessment, and personalized management of individuals with autoimmune thyroiditis at risk of developing thyroid cancer in India and globally.
Acknowledgments
Statement of Transparency and Principals:
• Author declares no conflict of interest
• Study’s data is available upon a reasonable request.
• All authors have contributed to implementation of this research.
References
- Is Hashimoto thyroiditis associated with increasing risk of thyroid malignancies? A systematic review and meta-analysis Abbasgholizadeh P, Naseri A, Nasiri E, Sadra V. Thyroid Research.2021;14(1). CrossRef
- Hashimoto's Thyroiditis and Papillary Cancer Thyroid Coexistence Exerts a Protective Effect: a Single Centre Experience Battistella E, Pomba L, Costantini A, Scapinello A, Toniato A. Indian Journal of Surgical Oncology.2022;13(1). CrossRef
- Hashimoto's Thyroiditis and Medullary Carcinoma of Thyroid Dasgupta S, Chakrabarti S, Mandal P. K., Das S.. JNMA; journal of the Nepal Medical Association.2014;52(194).
- Hashimoto's Thyroiditis Effects on Papillary Thyroid Carcinoma Outcomes: A Systematic Review Osborne D, Choudhary R, Vyas A, Kampa P, Abbas LF , Chigurupati HD , Alfonso M. Cureus.2022;14(8). CrossRef
- Relation of thyroid neoplasms to Hashimoto disease of the thyroid gland Dailey M. E., Lindsay S., Skahen R.. A.M.A. Archives of Surgery.1955;70(2). CrossRef
- Concurrent Presence of Hashimoto’s Thyroiditis with Papillary Carcinoma of Thyroid- A Retrospective Study Aramani A, Lasrado S, Hegde A, Kumar S. Journal Of Clinical And Diagnostic Research.2022;16. CrossRef
- Incidence trends for papillary thyroid carcinoma and their correlation with thyroid surgery and thyroid fine-needle aspirate cytology Burgess JR , Tucker P. Thyroid: Official Journal of the American Thyroid Association.2006;16(1). CrossRef
- Is Hashimoto's thyroiditis a risk factor for papillary thyroid cancer? Repplinger D, Bargren A, Zhang Y, Adler JT , Haymart M, Chen H. The Journal of Surgical Research.2008;150(1). CrossRef
- Medullary carcinoma arising in a thyroid with Hashimoto's disease Weiss L. M., Weinberg D. S., Warhol M. J.. American Journal of Clinical Pathology.1983;80(4). CrossRef
- Association between Hashimoto's thyroiditis and papillary thyroid carcinoma: a retrospective analysis of 305 patients Graceffa G, Patrone R, Vieni S, Campanella S, Calamia S, Laise I, Conzo G, Latteri M, Cipolla C. BMC endocrine disorders.2019;19(Suppl 1). CrossRef
- Coexistence of Histologically Proven Chronic Lymphocytic Thyroiditis with Other Thyroid Disorders: A Retrospective Study Gejoe G., Yadev I. P., Kumaran A, Swasthik K. S., Chisthi MM . Surgery Journal (New York, N.Y.).2022;8(2). CrossRef
- Thyroid disorders in India: An epidemiological perspective Unnikrishnan AG , Menon UV . Indian Journal of Endocrinology and Metabolism.2011;15(Suppl 2). CrossRef
- A study to evaluate association of nuclear grooving in benign thyroid lesions with RET/PTC1 and RET/PTC3 gene translocation Ashwini BR , Nirmala C, Natarajan M, Biligi DS . Thyroid Research.2023;16(1). CrossRef
- Association between Hashimoto's Thyroiditis and Thyroid Cancer in 64,628 Patients Resende de Paiva C, Grønhøj C, Feldt-Rasmussen U, Buchwald C. Frontiers in Oncology.2017;7. CrossRef
- Coexistence of Hashimoto's thyroiditis with papillary thyroid carcinoma. A retrospective study Mazokopakis EE , Tzortzinis AA , Dalieraki-Ott EI , Tsartsalis AN , Syros PK , Karefilakis CM , Papadomanolaki MG , Starakis IK . Hormones (Athens, Greece).2010;9(4). CrossRef
- IL-17 A correlates with disease progression in papillary thyroid carcinoma Banerjee S, Nahar U, Dahiya D, Gupta R, Mukherjee S, Sachdeva N, Sood A, Dey P, Radotra B, Bhansali A. Diagnostic Pathology.2023;18(1). CrossRef
- Role of cytotoxic T cells and PD-1 immune checkpoint pathway in papillary thyroid carcinoma Banerjee S, Nahar U, Dahiya D, Mukherjee S, Dey P, Gupta R, Radotra B, et al . Frontiers in Endocrinology.2022;13. CrossRef
- Medullary thyroid carcinoma co-existent with Hashimoto's thyroiditis diagnosed by a comprehensive cytological approach Malpani S, Tandon A, Panwar H, Khurana U, Kapoor N, Behera G, Gupta V. Diagnostic Cytopathology.2020;48(4). CrossRef
- Hashimoto’s thyroiditis-a tertiary level hospital based study Manikantan G, Chisthi M. International Journal of Research in Medical Sciences.2017. CrossRef
- Papillary Thyroid Cancer and Hashimoto's Thyroiditis: An Association Less Understood Anand A, Singh KR , Kushwaha JK , Hussain N, Sonkar AA . Indian Journal of Surgical Oncology.2014;5(3). CrossRef
- An Autobiographical Case Report on Papillary Thyroid Carcinoma with Positive Antithyroid Antibodies: Coincidence or Correlated? Singh A, Rao S, Rana DY , Choudhary M, Singh R. Cureus.2023;15(9). CrossRef
- Extramedullary plasmacytoma of thyroid - a mimicker of medullary carcinoma at fine needle aspiration cytology: A case report Bhat V, Shariff S, Reddy RAN . Journal of Cytology.2014;31(1). CrossRef
- Incidence of Thyroid Disorders in India: An Institutional Retrospective Analysis Nagarkar R, Roy S, Akheel M, Palwe V, Kulkarni N, Pandit P. International Journal of Dental and Medical Specialty.2015;2. CrossRef
- Prevalence of Antithyroid Antibodies in Histologically Proven Autoimmune Thyroid Diseases and Correlation with Thyroid Dysfunction in South India Shinto AS , Pachen L, Sreekanth TK , George D. Thyroid Sci.2010;5:1-5. www.ThyroidScience.com.
- Vitamin D, Thyroid Autoimmunity and Cancer: An Interplay of Different Factors Dutta D, Sharma M, Aggarwal S, Mohindra R, Bhattacharya S, Kalra S. Indian Journal of Endocrinology and Metabolism.2019;23(5). CrossRef
- Is Hashimoto's thyroiditis a risk factor for medullary thyroid carcinoma? Our experience and a literature review Zayed AA , Ali MKM , Jaber OI , Suleiman MJ , Ashhab AA , Al Shweiat WM , Momani MS , Shomaf M, AbuRuz SM . Endocrine.2015;48(2). CrossRef
- Follicular thyroid lesions coexisting with Hashimoto's thyroiditis: incidence and possible sources of diagnostic errors Kollur SM , El Sayed S, El Hag IA . Diagnostic Cytopathology.2003;28(1). CrossRef
- Warthin-like papillary carcinoma thyroid Kalantri SH , D'Cruze L, Barathi G., Singh BK . Journal of Cancer Research and Therapeutics.2023;19(5). CrossRef
- Is only Thyroid Peroxidase Antibody Sufficient for Diagnosing Chronic Lymphocytic Thyroiditis? Saygılı ES , Özgüven BY , Öztürk FY , Oğuzsoy T, Çakır SD , Basmaz SE , Batman A, Altuntaş Y. Sisli Etfal Hastanesi Tip Bulteni.2018;52(2). CrossRef
- Importance of combined approach of investigations for detection of asymptomatic Hashimoto Thyroiditis in early stage Saraf SR , Gadgil NM , Yadav S, Kalgutkar AD . Journal of Laboratory Physicians.2018;10(3). CrossRef
- Diagnostic accuracy of fine needle aspiration cytology of the thyroid: impact of ultrasonography and ultrasonographically guided aspiration Solymosi T., Toth G. L., Bodo M.. Acta Cytologica.2001;45(5). CrossRef
- Clinical, biochemical & cytomorphologic study on Hashimoto's thyroiditis Thomas T, Sreedharan S, Khadilkar UM , Deviprasad D, Kamath MP , Bhojwani KM , Alva A. The Indian Journal of Medical Research.2014;140(6).
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2025
Author Details