Understanding Chemotherapy Adherence in Breast Cancer Patients: A Multidimensional Review through the WHO Adherence Framework
Download
Abstract
Background: Breast cancer is the most prevalent cancer globally and a major public health challenge in low and middle-income countries (LMIC) like Pakistan. Despite advances in treatment, poor adherence to chemotherapy remains a concern, affecting survival, recurrence and quality of life. Adherence is influenced by individual, social, cultural and systemic factors.
Objective: This review uses the WHO-Multidimensional Adherence Model (WHO-MAM) to identify key factors influencing chemotherapy adherence among breast cancer patients in LMICs. It aims to highlight underexplored domains particularly behavioural and cultural influences and suggest directions for targeted interventions and policy development.
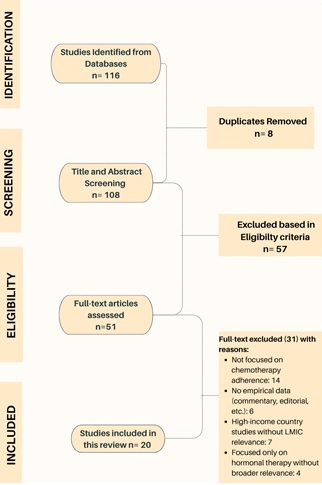
Methods: This scoping review was conducted using literature published between 2019 and 2025, sourced from PubMed, Scopus and Google Scholar. A total of 51 full-text articles were reviewed, 20 articles were included based on relevance to chemotherapy adherence and applicability to LMIC settings.
Key Findings: Chemotherapy adherence is influenced by socioeconomic barriers (e.g., financial constraints, low education), healthcare system limitations (e.g., poor provider communication, limited oncology access), and treatment-related challenges (e.g., side effects). Patient-related factors such as mental health, perceived stigma, and cultural beliefs are significant but underexplored, especially in South Asia.
Conclusion: Improving chemotherapy adherence requires patient-centred, culturally informed strategies and health system reforms. Greater attention to behavioural and cultural factors is essential for designing interventions that are both practical and effective in LMIC settings.
Introduction
Breast cancer is the most common cancer worldwide, impacting millions of people each year. It continues to be a major public health concern. The disease is more prevalent among women of all ages compared to men [1]. The World Health Organization (WHO) 2022 report states that in 2020, an estimated 2.3 million women were diagnosed with breast cancer, leading to approximately 685,000 deaths worldwide [2].
Breast cancer is the leading cause of cancer-related deaths among women, accounting for about 95% of fatalities. Nearly 70% of those occur in low and middle-income countries (LMICs) [1]. Pakistan has the highest incidence in Asia, with 1 in 9 women testing positive for breast cancer. The number of cases is rising, with increasing rates of incidence and later-stage diagnoses [3].
Adherence to chemotherapy, which is a crucial part of cancer care, remains a major challenge. The WHO highlights that adherence to long-term cancer treatment regimens is a concern globally. This leads to worse health outcomes and higher healthcare costs [4].
Despite the central role chemotherapy plays in breast cancer management, adherence rates vary greatly in studies worldwide. Estimates range from 56% to 85% in studies from different parts of the world [5-7]. Therefore, understanding the multifaceted factors that influence adherence behaviors in breast cancer patients is essential for improving treatment outcomes and disease prognosis.
Importance of Adherence in Chemotherapy
The concept of adherence has evolved, especially in the context of healthcare, as shown in Figure 1, which visually outlines the shift in terminology from obedience to patient-centered adherence.
Figure 1. Historical Progression of Terminology and Approaches to Patient Adherence in Medicine (Pre-1940s to Present).
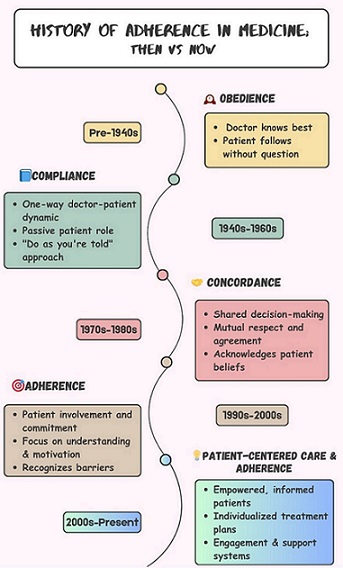
In the initial days, the term “Obedience” and “compliance” were more commonly used, implying a more passive role for patients who were expected to follow medical advice without question [8, 9]. Later, the word “concordance” was also introduced in medicine, with the meaning “agreeing with harmony” [10].
Over time, “adherence” has become a more preferred terminology as it reflects a more active role of patients, and also emphasizes a collaborative approach between patients and their primary healthcare provider [11].
WHO defines adherence as “the extent to which a person’s behavior corresponds to recommendations jointly established with the health care providers regarding medication, dietary restrictions and habits, physical activity, adequate rest and adherence to scheduled appointments” [12].
In the context of chemotherapy, adherence ensures that patients receive timely and consistent doses essential for optimal therapeutic outcomes. High adherence is associated with a reduced risk of recurrence and mortality, while poor adherence can lead to chemotherapy resistance, disease progression and worse prognosis [13].
Materials and Methods
This review aims to synthesize existing literature on chemotherapy adherence among breast cancer patients, using the WHO Multidimensional Adherence Model (WHO-MAM) as a guiding framework. It focuses on identifying key factors affecting adherence, with particular emphasis on studies from LMICs.
Search Strategy
We conducted a systematic search across academic databases, which includes PubMed, Scopus and Google Scholar. The search strategy combined Medial Subject Headings (MeSH) and free-text terms using Boolean operators (AND/OR) and truncations to create relevant search strings.
The search targeted articles published from 2019 to June 2025. Key terms included: “Chemotherapy adherence”, “breast cancer”, “low and middle income-countries”, “predictors of adherence” and “factors influencing adherence”.
Inclusion Criteria
We included studies focused on adherence to chemotherapy among women with breast cancer, particularly those receiving intravenous (IV) chemotherapy either adjuvant or neoadjuvant. We also considered studies on general cancer populations if breast cancer patients made up the majority of the sample and if the findings could be reasonably applied. Studies on adjuvant hormonal or endocrine therapy were included if they discussed factors related to adherence such as behavioral, psychological, cultural, socioeconomic and healthcare system-related determinants.
Priority was given to studies conducted in LMICs or those providing insights relevant to such settings. We accepted both quantitative and qualitative peer-reviewed studies, along with systematic reviews and conceptual papers that informed the application of the WHO Multidimensional Adherence Model. Only English-language articles published between 2019 and June 2025 were considered.
Exclusion Criteria
Studies were excluded if they did not focus behaviors related to adherence or the factors that influence these behaviors in relation to breast cancer treatment. Articles that looked only at adherence to hormonal therapy without considering chemotherapy adherence were not included. Non-peer-reviewed materials such as editorials, commentaries, letters to the editor, and news articles without empirical data were not excluded. Lastly, studies conducted in high-income countries (HIC) were mainly excluded unless they provided findings clearly relevant to LMICs or offered insights for understanding barriers and facilitators.
Study Selection Process
An initial search found 116 articles from the databases. After removing duplicates, 108 articles were left and assessed based on their title and abstract. After screening, 51 articles were chosen for full-text review. Following a thorough evaluation, 20 studies were included in the final synthesis based on their relevance to WHO-MAM domains. A PRISMA flow diagram showing the detailed study selection process is presented in Figure 2.
Figure 2. PRISMA Flow Diagram of the Study Selection Process.
Global Overview of Chemotherapy Adherence in Breast Cancer Patients
Chemotherapy adherence is a key factor affecting treatment outcome for breast cancer patients. It requires a team effort between patients and healthcare providers to follow prescribed plans regarding dosage, frequency, duration and completion of chemotherapy [12].
However, studies that specifically measure chemotherapy adherence among breast cancer patients are limited. In the literature available, differences in how adherence is measured lead to inconsistent findings. For example, a 2022 study from Ethiopia reported an adherence rate of 83.5%, based on the number of chemotherapy doses received relative to those prescribed. The data were collected through in-person and telephone interviews [13]. In contrast, a 2025 study from Ethiopia using the Morisky Medication Adherence Scale (MMAS), found that only 42.6% of patients has good adherence [14]. Despite differing methods, both studies identified similar barriers to adherence: lack of social support, financial constraints, transportation challenges and side effects [13, 14].
The severity of side effects is often noted as a significant factor. A Nigerian study revealed that 35% of breast cancer patients skipped at least one dose due to severe side effects, while 65% of those who had only mild or moderate side effects managed to comply with the chemotherapy schedule. Adherence is this study was measured by the proportion of prescribed doses received within the intended timeframe [6].
Research also indicates that receiving at least 85% of the planned intravenous (IV) chemotherapy is linked to better health outcomes. However, women with stage II breast cancer who received less than 65% of their planned dose showed higher recurrence rates within five years [15]. A study from Cameroon reported a much lower adherence rate of 56.1%, attributing this largely to the patient’s motivation and understanding of their disease and treatment [7]. A similar study from India found that 57.8% of patients had high adherence, 26.7% had intermediate adherence, and 15.6% had low adherence [16]. Both studies used the MMAS scale for measurement.
In Brazil, an upper-middle-income country, a study used the MMAS scale and found an adherence rate of 58.7%. It pointed out that financial burden, inability to work and ovarian suppression contributed significantly to non-adherence [17]. Although Brazil has a more developed healthcare system than many LMICs, these challenges highlight ongoing systemic and socioeconomic issues common in resource-constrained settings [18]. Factors such as out-of-pocket costs despite public healthcare coverage, long waiting times, problems with drug availability, and limited communication between patients and providers contribute to difficulties with adherence [18, 19].
Moreover, low health literacy, side effects, and a lack of social support reflect barriers seen in studies from Ethiopia, Nigeria and India [6, 14, 16]. This indicates that a nation’s economic status alone does not account for patient adherence behaviors; instead, structural and social contexts in which care is provided play a significant role [19].
In contrast, data from high-income countries show relatively higher adherence levels. For example, a large U.S study among privately insured breast cancer survivors reported 84.4% one-year adherence to hormonal therapy and 62.2% adherence at five years, measured by medication possession ratio of 80% or greater. Non-adherence in this context was mainly linked with factors such as insurance type and education level rather than access to the healthcare system [20]. Although cost-related non- adherence still occurs in high-income settings, the extent is usually lower due to broader insurance coverage, patient education, and more reliable follow-up systems [19, 21]. Studies focusing specifically on IV chemotherapy adherence are particularly limited. Among those that exist, the MMAS is one of the most commonly used tools, although other methods, such as administered dose calculations, have been explored [17]. These alternative methods often rely on accurate pharmacy databases and patient records for medication management, which may not be consistently available or maintained across different healthcare systems [19]. Even with the MMAS tool, there are variations. The older version, MMAS-4, has lower reliability compared to MMAS-8 [5, 12]. The MMAS-8 is considered more robust, easier to administer and relatively cost-effective [16]. However, as a self-reported measure, it is still prone to biases, including social desirability bias, which may result in an overestimation of adherence [17]. From a LMIC perspective, adherence rates seem to fall within a similar range, highlighting common structural limitations. The barriers to adherence are complex and multidimensional, which revolve around healthcare delivery inefficiencies, financial hardship, geographic inaccessibility and gaps in resource availability [7, 18, 21]. Understanding these overlapping challenges is essential for creating context-sensitive interventions that can improve chemotherapy adherence in diverse healthcare settings.
WHO-Multidimensional Adherence Model (WHO-MAM) & Chemotherapy Adherence
The World Health Organization (WHO) has developed frameworks to understand and improve adherence to treatment regimen. One of these model is the WHO-Multidimensional Adherence Model (WHO-MAM) as shown in Figure 3.
Figure 3. WHO Multidimensional Adherence Model (WHO-MAM).
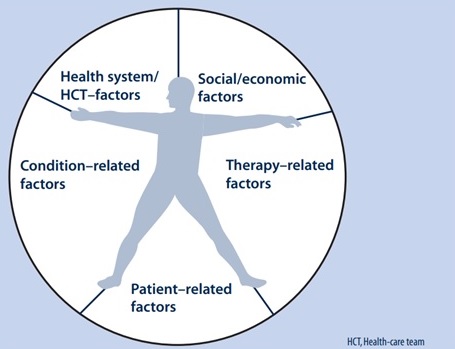
This model highlights five key dimensions influencing adherence behavior: socioeconomic factors, healthcare system-related factors, disease-related factors, treatment-related factors and patient-related factors [18]. It shows that adherence is shaped by the interplay of these domains rather than a single factor.
Chemotherapy adherence can also be viewed through this model, as illustrated in Figure 4.
Figure 4. Expanded Model of Factors Influencing Chemotherapy Adherence in Breast Cancer Care.
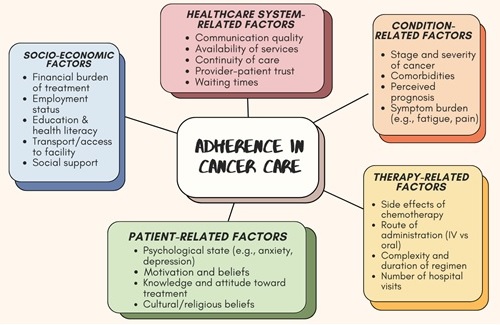
Cultural and behavioral views, which are often overlooked in research, fall under patient-related factors and are vital for understanding adherence in breast cancer care.
Factors Influencing Chemotherapy Adherence
1. Socioeconomic Factors
Higher levels of education are often associated with better health literacy, which may improve understanding of the importance of chemotherapy adherence [22]. However, some researchers argue that education level does not always translate into higher health literacy [23]. Women with less education may struggle more with adherence, often due to overlapping challenges such as limited income or lack of financial support. In LMICs, the financial burden of treatment, including lack of insurance coverage or financial aid, frequently forces patients to skip or discontinue chemotherapy [21, 24].
2. Healthcare System-related Factors
Effective communication and patient-centered care are linked with higher satisfaction and better adherence outcomes [25]. Physical access to healthcare facilities is critical, as patients living far from treatment centers may face difficulties maintaining regular chemotherapy schedules, while routine delays in initiating or continuing treatment can undermine trust and negatively impact adherence [26]. Additional systemic challenges include limited availability of trained oncology staff, lack of continuity in care, long waiting times and frequent drug stock-outs [27, 28].
3. Condition-related factors
Different types of breast cancer respond differently to chemotherapy. For example, triple-negative breast cancer often requires a more aggressive chemotherapy regimen due to the absence of hormone receptors and HER2 protein, which can affect adherence because of increased treatment intensity and side effects [29]. Tumor location and higher-grade cancers may also require a more intensive chemotherapy regimen further influencing adherence [30].
4. Treatment-related Factors
Chemotherapy regime often involves multiple cycles, IV administration and adverse effects such as nausea, fatigue, hair loss and neuropathy. These side effects are among the leading causes of non-adherence [15]. Literature highlights that the intensity and duration of treatment, as well as the complexity of drug administration, can negatively impact adherence levels [31]. Furthermore, patients may stop or delay treatment due to perceived or experienced toxicity, fear of adverse effects or lack of perceived benefits, particularly in the absence of strong social or medical support [32].
5. Patient-related Factors
Patient’s beliefs, psychological well-being and individual experiences significantly influence chemotherapy adherence. A strong belief in the effectiveness of treatment is positively associated with adherence, while misconceptions and skepticism are linked to non-adherence [33]. Psychological distress, which includes anxiety, depression and fear of side effects, can also impair a patient’s ability to follow with treatment regimens [33, 34].
Functional aspects such as social and physical well-being also play a role. Patients with good family and social support generally show more resilience and are better equipped to manage the treatment process [24]. Those with better baseline physical health and fewer side effects are more likely to comply with chemotherapy schedules [5].
5.1 Behavioral Perspective
From a behavioral standpoint, a patient’s perception of chemotherapy and its side effects can be a major determinant of adherence [35]. Fear of adverse effects like nausea, hair loss and fatigue often leads to missed or delayed doses, ultimately reducing treatment efficacy [4, 33].
Mental health is another critical component. Higher levels of emotional distress, particularly anxiety and depression, are strongly associated with non-adherence [36]. A meta-analysis estimates that depression affects 30.2% of breast cancer patients globally, with the rate as high as 83% in Pakistan [33]. Depression can reduce motivation and energy, making it harder for patients to maintain regular treatment schedules [12].
Furthermore, there is evidence in the literature where it has been reported that patients with strong social support networks are likely to be more adherent towards treatment plans, as they receive good emotional support, encouragement and assistance from their family and friends in these vulnerable times [37, 38]. Moreover, good effective communication between patients and their healthcare providers, such as giving clear instructions, addressing concerns, and offering emotional support can also improve adherence and overall patient’s satisfaction with the treatment process, which ultimately results in positive outcomes for the patients [18, 39].
5.2 Cultural Perspective
Cultural beliefs and norms significantly shape patient’s attitudes toward illness and treatment. Pervasive stigma around cancer often leads to fear, secrecy and reluctance to adhere to chemotherapy [40]. In some communities, distrust in Western medicine and preference for traditional or alternative therapies further complicate adherence behavior [3].
The impact of cultural norms on chemotherapy adherence can also be observed in the context of gender roles and responsibilities. Some literature highlights that women from Pakistani culture are expected to prioritize caregiving responsibilities over their own health needs, which results in those women often facing challenges in adhering to their chemotherapy treatment due to these societal expectations and their gender-specific roles [3]. This pressure to sufficiently fulfil their caregiving duties can lead to delayed or interrupted treatment, which ultimately affects treatment outcomes.
The path of treatment often involves a combination of treatment modalities like chemotherapy and surgery. Unfortunately, for some patients, that path leads to mastectomy which is a surgical procedure involving the removal of the entire breast. Which is known to cause emotional distress due to fear of societal judgment, cultural expectations, personal beliefs, personal fear of rejection, or reduced self-worth, may drive a woman to avoid further medical treatment altogether [41]. They may also experience a negative self-image, feel less attractive and feminine which affects their interpersonal relationships as well as their sexual life [42]. Ultimately, it affects adherence to chemotherapy either post-surgery or before impending surgery [41, 42].
While these factors highlight the complexity of the adherence behaviors, they also help health systems, policy makers and communities to identify the areas where targeted interventions can be done to make meaningful differences.
Proposed Interventions to Improve Chemotherapy Adherence
Improving adherence to chemotherapy in LMICs requires a combination of health system strengthening, culturally appropriate patient support and policy-level reforms. Based on the WHO-MAM model, targeted interventions can be developed for all five dimensions.
1. Socio-economic Interventions
Financial barriers are one of the most common reasons for missed or delayed chemotherapy cycles in LMICs [31]. Programs that offer subsidized cancer treatment, cash transfer and transportation vouchers have shown promise in improving adherence [43]. For example, in Brazil’s Unified Health System provides free chemotherapy based on national cancer guidelines [44]. Likewise, countries such as India and the Philippines have started government- funded health insurance schemes that lower out-of-pocket cost for cancer patients [45, 46]. Pakistan could think about expanding current initiatives like the Sehat Card to offer comprehensive oncology coverage with adherence monitoring components [47].
2. Healthcare System Strengthening
A major reason for poor adherence is fragmented and overburdened health systems [40]. LMICs can benefit from adopting task-shifting models where community health workers conduct follow-up, provide counselling and monitor symptoms. This method has been successful in improving adherence to HIV treatment and can be adapted for oncology care [19].
Telemedicine, electronic reminders, and patient navigation services can also enhance continuity of care [48]. A pilot mHealth program in Kenya used SMS reminders and nurse-led phone consultations to boost appointment attendance among cancer patients [49].
3. Condition and Treatment-Related Interventions
Complex chemotherapy regimens and severe side effects often lead to treatment discontinuation [7]. Simplifying the regimen, when medically possible and using proactive side effect management protocols can improve adherence [16]. Integrating palliative care early in treatment, as done in Uganda’s cancer centers, has helped reduce symptom burden and increase treatment completion [50]. Pain management, nutritional counselling, and managing nausea or fatigue can make chemotherapy more tolerable [34].
4. Patient Support and Behavioral Interventions
Patient beliefs, mental health and family support are crucial for adherence [14, 36]. Support groups, peer mentoring and psychosocial counselling are effective but often underused strategies. In Ghana, a hospital-based psychosocial support program for breast cancer patients led to better adherence to chemotherapy schedules [38]. Interventions that include culturally relevant education materials, story-based learning and family involvement have also shown potential. Addressing fatalistic attitudes through community health discussions and involving religious leaders can help reduce stigma and fear [36].
5. Policy-Level and Structural Reforms
On a larger scale, national cancer control programs should include adherence as a standard outcome to measure.
Routine data collection through cancer registries, patient-reported outcomes, and digital health platforms is necessary to track progress. Twining programs, i.e. partnership between LMIC and High Income Countries (HIC), can help effectively share knowledge and skills while increasing access to essential chemotherapy drugs and diagnostics [19]. Moreover, adding adherence modules to oncology nursing courses and ongoing training programs for healthcare providers can improve communications between providers and patients [51].
In conclusion, chemotherapy adherence among breast cancer patients is a complex issue, especially in LMICs where structural, socio-economic, and cultural barriers often hinder treatment continuity. This review emphasized that adherence is influenced not only by clinical or treatment-related factors, but also by broader issues like health literacy, access to care, financial burden, and cultural norms.
Understanding adherence through the WHO-MAM framework helped identify actionable intervention opportunities across the individual, health system and community levels. Despite global efforts to improve adherence, there is still a significant lack of context-specific evidence from LMICs, particularly in countries like Pakistan. Behavioral and cultural aspects such as stigma, fatalism and mistrust in the healthcare system, along with reliance on informal caregivers, remain underexplored in existing literature, even though they significantly impact a patient’s behavior and decision-making.
The policy implications from this review highlights the urgent need to strengthen public health infrastructure for long-term cancer care. Increasing access to universal health coverage for chemotherapy, integrating adherence counselling into routine oncology care, and investing in community support programs can enhance adherence rates. Furthermore, policymakers should review and reform cancer care financing models and health insurance plans to lower out-of-pocket costs and ensure reliable treatment access for vulnerable populations.
Future research should focus on qualitative studies to explore patient experiences, beliefs and barriers to adherence. Interventional studies can help access how effective culturally tailored counselling, community support, and reminder systems are in improving adherence. Lastly, locally relevant and culturally sensitive public health education campaigns can raise awareness, reduce stigma, and enhance patient engagement in breast cancer care.
By combining evidence-based interventions with community engagement and supportive health policies, LMICs can strengthen adherence support systems and improve long-term outcomes for breast cancer patients.
List of Abbreviations
WHO, World Health Organization; LMIC, Low and Middle Income Country; WHO-MAM, World Health Organization Multi-dimensional Adherence Model; 4. MeSH, Medical Subject Headings; IV, Intravenous (Route of medicine administration); MMAS, Morisky Medication Adherence Scale; HER2, Human Epidermal Growth Factor Receptor 2; HIC, High Income Countries ;
Declarations
Ethics approval and consent to participate: Not applicable. This is a review article and does not involve human participants or data collection.
Consent for publication
Not applicable
Availability of data and materials
Not applicable
Competing interest
The author declares that there are no competing interests.
Funding
The author received no external funding for the development of this review.
Author’s contributions
The author, Lamha Saleem Sayani, conceived, researched and wrote the review article independently.
Acknowledgements
The author gratefully acknowledges the use of Grammarly to assist in grammar and language refinement during the manuscript preparation process. The author also acknowledges the World Health Organization for granting permission to reproduce Figure 1 from Adherence to Long-Term Therapies: Evidence for Action (© WHO 2003. All rights reserved)
Author’s information
L.S is a 2024 graduate of the inaugural batch of Master of Science in Public Health (MSPH) program at Aga Khan University. She holds a background in oncology nursing from Aga Khan University Hospital and has a strong research interest in breast cancer, patient well-being and public health systems in LMICs.
References
- Breast cancer Factsheet: World Health Organization; 2023 [Available from: https://www.who.int/news-room/fact-sheets/detail/breast-cancer?gclid=Cj0KCQiA4Y-sBhC6ARIsAGXF1g4K7UTu6jLDhOVZ646_3hyOUb8svd0g_kD2dZ3RaxHES8-8B500y08aAmEoEALw_wcB .
- World health ranking life expectancy: World Health Organization; 2020 [Available from: https://www.worldlifeexpectancy.com/pakistan-breast-cancer .
- Fears and barriers: problems in breast cancer diagnosis and treatment in Pakistan Saeed S, Asim M, Sohail MM . BMC women's health.2021;21(1). CrossRef
- Factors influencing five-year adherence to adjuvant endocrine therapy in breast cancer patients: A systematic review Yussof I, Mohd Tahir NA , Hatah E, Mohamed Shah N. Breast (Edinburgh, Scotland).2022;62. CrossRef
- Adherence to Adjuvant Hormonal Therapy and Associated Factors Among Women with Breast Cancer Attending the Tikur Anbessa Specialized Hospital, Addis Ababa Ethiopia, 2019: A Cross-sectional Study Wako Z, Mengistu D, Dinegde NG , Asefa T, Wassie M. Breast Cancer (Dove Medical Press).2021;13. CrossRef
- Evaluation of side effects and compliance to chemotherapy in breast cancer patients at a Nigerian tertiary hospital Folorunso SA , Abiodun OO , Abdus-Salam AA , Wuraola FO . Ecancermedicalscience.2023;17. CrossRef
- Characterizing factors influencing adherence to surgery and chemotherapy amongst women suffering from breast cancer in Mbingo Baptist Hospital Cameroon Nkenu NG , Nsoh M, Paul AJ , Nkondjock A. The Pan African Medical Journal.2022;43. CrossRef
- Patient compliance: A concept analysis Thummak S, Uppor W, Wannarit L. Belitung Nursing Journal.2023;9(5). CrossRef
- The evolution of the doctor-patient relationship Keslar L. 2023;100.
- Obedience to collaboration: compliance, adherence and concordance Rae B. Journal of Prescribing Practice.2021;3(6). CrossRef
- Medication Adherence in Cancer Patients: A Comprehensive Review Reshma V, Chacko AM , Abdulla N, Annamalai M, Kandi V. Cureus.2024;16(1). CrossRef
- Adherence to Chemotherapy and Associated Factors Among Patients With Cancer in Amhara Region, Northeastern Ethiopia, 2022. A Cross-Sectional Study Bekalu YE , Wudu MA , Gashu AW . Cancer Control: Journal of the Moffitt Cancer Center.2023;30. CrossRef
- Adherence to Chemotherapy among Women with Breast Cancer Treated at Tikur Anbessa Specialized and Teaching Hospital, Addis Ababa, Ethiopia Hassen F, Enquselassie F, Ali A, Addissie A, Taye G, Assefa M, Tsegaye A. Asian Pacific journal of cancer prevention: APJCP.2022;23(9). CrossRef
- Adherence to intravenous chemotherapy and associated factors among patients with cancer at Hawassa University Comprehensive Specialized Hospital Cancer Treatment Center, Sidama Region, Southern Ethiopia Balta B, Delelegn Al, Demissie G, Deribe B. PloS One.2025;20(4). CrossRef
- Patterns of Anthracycline-Based Chemotherapy-Induced Adverse Drug Reactions and Their Impact on Relative Dose Intensity among Women with Breast Cancer in Ethiopia: A Prospective Observational Study Gadisa DA , Assefa M, Tefera GA , Yimer G. Journal of Oncology.2020;2020. CrossRef
- Parallel Assessment of Chemotherapy Adherence and Supportive Therapy Adherence on Occurrence and Minimization of Adverse Drug Reactions Among Cancer Patients: A Clinical-Based Observational Study Kumar J, Gudhoor M, Ganachari MS . The Journal of Pharmacy Technology: jPT: Official Publication of the Association of Pharmacy Technicians.2020;36(2). CrossRef
- Adherence to Adjuvant Endocrine Therapy in Patients With Nonmetastatic Estrogen Receptor-Positive Breast Cancer: A Comprehensive Brazilian Real-World Data Study Assad-Suzuki D, Laperche-Santos D, Resende H, Moura FC , Oliveira SCS , Shimada AK , Arakelian R, et al . JCO global oncology.2025;11. CrossRef
- An Adaptable Framework for Factors Contributing to Medication Adherence: Results from a Systematic Review of 102 Conceptual Frameworks Peh KQE , Kwan YH , Goh H, Ramchandani H, Phang JK , Lim ZY , Loh DHF , et al . Journal of General Internal Medicine.2021;36(9). CrossRef
- Barriers to cancer treatment for people experiencing socioeconomic disadvantage in high-income countries: a scoping review Bourgeois A, Horrill T, Mollison A, Stringer E, Lambert LK , Stajduhar K. BMC health services research.2024;24(1). CrossRef
- Prescription Patterns, Initiation, and 5-Year Adherence to Adjuvant Hormonal Therapy Among Commercially Insured Patients With Breast Cancer Zhao H, Lei X, Niu J, Zhang N, Duan Z, Chavez-MacGregor M, Giordano SH . JCO oncology practice.2021;17(6). CrossRef
- Adherence to breast cancer guidelines is associated with better survival outcomes: a systematic review and meta-analysis of observational studies in EU countries Ricci-Cabello I, Vásquez-Mejía A, Canelo-Aybar C, Niño de Guzman E, Pérez-Bracchiglione J, Rabassa M, Rigau D, et al . BMC health services research.2020;20(1). CrossRef
- Social Characteristics and Adherence to Adjuvant Endocrine Therapy in Premenopausal Women With Breast Cancer Schmidt JA , Woolpert KM , Hjorth CF C, Farkas DK , Ejlertsen B, Cronin-Fenton D. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2024;42(28). CrossRef
- Factors influencing chemotherapy knowledge in women with breast cancer Parker PD , Heiney SP , Adams SA , Friedman DB , Dawson RM . Applied nursing research: ANR.2020;56. CrossRef
- Factors influencing non–adherence to chemotherapy: Perspective of Nigerian breast cancer survivors Ingwu J, J, Idoko C, C, Israel C, C, Maduakolam I, I, Madu O O. Journal of Health Science Research.. CrossRef
- Investigation of Factors Affecting Adherence to Adjuvant Hormone Therapy in Early-Stage Breast Cancer Patients: A Comprehensive Systematic Review Yang S, Park SW , Bae SJ , Ahn SG , Jeong J, Park K. Journal of Breast Cancer.2023;26(4). CrossRef
- Patient delay in initiating treatment after breast cancer diagnosis: A cause for concern Olaogun J, Agodirin O, Idowu D. Journal of Health Science Research.2024;9:1-5.
- Reducing Chemotherapy Waiting Times in the Ambulatory Setting of a Tertiary Cancer Centre Using a Design Thinking Approach Jen W, Chan ZY , Lee YM , Ng N, Tan B, Teo C, Wong YP , Chee CE , Chee Y. Cancers.2023;15(18). CrossRef
- Distribution of the workforce involved in cancer care: a systematic review of the literature Trapani D., Murthy S. S., Boniol M., Booth C., Simensen V. C., Kasumba M. K., Giuliani R., Curigliano G., Ilbawi A. M.. ESMO open.2021;6(6). CrossRef
- Triple Negative Breast Cancer Treatment Options and Limitations: Future Outlook Obidiro O, Battogtokh G, Akala EO . Pharmaceutics.2023;15(7). CrossRef
- Breast Cancer-Epidemiology, Classification, Pathogenesis and Treatment (Review of Literature) Smolarz B, Nowak AZ , Romanowicz H. Cancers.2022;14(10). CrossRef
- Overcoming barriers to patient adherence: the case for developing innovative drug delivery systems Baryakova TH , Pogostin BH , Langer R, McHugh KJ . Nature Reviews. Drug Discovery.2023;22(5). CrossRef
- Causes and Consequences of Chemotherapy Delays in Ambulatory Oncology Practices: A Multisite Qualitative Study Lafferty M, Fauer A, Wright N, Manojlovich M, Friese CR . Oncology Nursing Forum.2020;47(4). CrossRef
- Global depression in breast cancer patients: Systematic review and meta-analysis Javan Biparva A, Raoofi S, Rafiei S, Masoumi M, Doustmehraban M, Bagheribayati F, Vaziri Shahrebabak ES , et al . PloS One.2023;18(7). CrossRef
- Comprehensive Review of Breast Cancer Consequences for the Patients and Their Coping Strategies: A Systematic Review Kasgri KA , Abazari M, Badeleh SM , Badeleh KM , Peyman N. Cancer Control: Journal of the Moffitt Cancer Center.2024;31. CrossRef
- Adherence to adjuvant tamoxifen and associated factors in breast cancer survivors Uslu Y, Kocatepe V, Sezgin DS , Uras C. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer.2023;31(5). CrossRef
- Quality of life and wellbeing among breast cancer patients in Lahore, Pakistan Ayub F, Khan TM , Baig MR , Amin MU , Tahir H. Frontiers in Oncology.2023;13. CrossRef
- The Impact of Unsupportive Social Support on the Injured Self in Breast Cancer Patients Sebri V, Mazzoni D, Triberti S, Pravettoni G. Frontiers in Psychology.2021;12. CrossRef
- Availability, accessibility, and impact of social support on breast cancer treatment among breast cancer patients in Kumasi, Ghana: A qualitative study Adam A, Koranteng F. PloS One.2020;15(4). CrossRef
- Adherence to oral anticancer hormonal therapy in breast cancer patients and its relationship with treatment satisfaction: an important insight from a developing country Koni AA , Suwan BA , Nazzal MA , Sleem A, Daifallah A, Allah MH , Odeh RY , Zyoud SH . BMC women's health.2023;23(1). CrossRef
- Challenges in Access to New Therapeutic Agents: Marginalized Patients With Cancer in Pakistan and the Need for New Guidelines Aziz Z, Naseer H, Altaf A. JCO global oncology.2022;8. CrossRef
- Beyond the scars: a qualitative study on the experiences of mastectomy among young women with breast cancer in a country with crisis Hasan S, Chew KS , Balang RV , Wong SSL . BMC women's health.2023;23(1). CrossRef
- The Impact of a Breast Cancer Diagnosis on the Social Interaction Patterns of Young Omani Women: A Qualitative Study Approach Al-Azri M, Al-Kiyumi Z, Al-Bimani K, Al-Awaisi H. Current Oncology (Toronto, Ont.).2024;31(12). CrossRef
- Interventions to address cancer-related financial toxicity: Recommendations from the field Edward J, Petermann VM , Eberth JM , Zahnd WE , Vanderpool RC , Askelson N, Rohweder CL , et al . The Journal of Rural Health: Official Journal of the American Rural Health Association and the National Rural Health Care Association.2022;38(4). CrossRef
- Geographic accessibility to cancer treatment in Brazil: A network analysis Fonseca BDP , Albuquerque PC , Saldanha RDF , Zicker F. Lancet Regional Health. Americas.2022;7. CrossRef
- Cancer prevention and control in India can get a boost through primary health care-based approach: A review Lohiya A, Daniel RA , Smith RD , Nagar M, Shankar A, Lahariya C. Journal of Family Medicine and Primary Care.2022;11(8). CrossRef
- DOH, WHO launch 2024-2028 National Integrated Cancer Control Program (NICCP) Strategic Framework: World Health Organization; 2024 [Available from: https://www.who.int/philippines/news/detail/14-02-2024-doh--who-launch-2024-2028-national-integrated-cancer-control-program-(niccp)-strategic-framework .
- Pakistan's Healthcare System: A Review of Major Challenges and the First Comprehensive Universal Health Coverage Initiative Khan SJ , Asif M, Aslam S, Khan WJ , Hamza SA . Cureus.2023;15(9). CrossRef
- Telemedicine for healthcare: Capabilities, features, barriers, and applications Haleem A, Javaid M, Singh RP , Suman R. Sensors International.2021;2. CrossRef
- Current Evidence on the Use of mHealth Approaches in Sub-Saharan Africa: A Scoping Review Aboye GT , Vande Walle M, Simegn GL , Aerts JM . Health Policy and Technology.. CrossRef
- Why and How to Integrate Early Palliative Care Into Cutting-Edge Personalized Cancer Care Petrillo LA , Jones KF , El-Jawahri A, Sanders J, Greer JA , Temel JS . American Society of Clinical Oncology Educational Book. American Society of Clinical Oncology. Annual Meeting.2024;44(3). CrossRef
- Patient-centered interprofessional education in cancer care: a systematic scoping review Fragner T, Hama H, Šerifović A, Kirchheiner K, Grabovac I. BMC medical education.2024;24(1). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2025
Author Details