Association between LGR5 Expression and Overall Survival in Patients with Colorectal Cancer: A Retrospective Study from Indonesia
Download
Abstract
Background: Leucine-rich repeat-containing G-protein-coupled receptor 5 (LGR5), also known as GPR49, is a Wnt signaling target that plays an important role in colorectal carcinogenesis and is often associated with poor prognosis in patients with colorectal cancer. Aim of this study was to assess the influence of LGR5 expression and its relationship with overall survival (OS) in colorectal cancer.
Material and methods: This retrospective study assessed LGR5 expression via immunohistochemistry (IHC) in 30 archival colorectal cancer tissue samples from patients resected between 2019-2020 in Makassar, Indonesia. The association between LGR5 expression levels (high vs. low) and overall survival (OS) was analyzed.
Result: Research results were obtained from 30 samples. Overall, 8 patients with high LGR5 expression and 22 patients with low LGR5 were reported. Among the total number of patients enrolled, 22 patients had an OS of 3 years and 8 patients had an OS of 5 years. Statistical analysis showed that there was no association between LGR5 expression and the clinical profile of colorectal cancer patients (p-value > 0.05). A statistically significant association between OS and both tumor stage and histopathological grading (p-value <0.001 and 0.016, respectively) was found. However, no statistically significant association between OS and LGR5 expression was observed (p-value 0.418).
Conclusion: LGR5 expression was not associate with either OS and or clinical characteristics of CRC patients in Makassar, Indonesia. However, there was a tendency for low LGR5 expression to be associated with improved OS, although this finding was not statistically significant. Both tumor stage and histopathological grading were associated with OS.
Introduction
Colorectal cancer (CRC) is a general term that includes cancer of the colon, rectosigmoid junction, and rectum [1, 2]. According to GLOBOCAN 2022 data, the incidence of CRC in Indonesia is 35,676 out of 408,661 (8.7%), with mortality rates ranked 5th (7.9%) of all cancer types recorded in the database [3-5]. The incidence rate is higher in males than in females, (annually 21,903 versus 13,773 cases per 100,000, respectively), with males experiencing a higher mortality rate than females (15.7 versus 8.9 deaths per 100,000, respectively) [5]. These differences are increasingly apparent after the age of 50 [6, 7]. The reasons for this sex-based disparity are considered multifactorial, involving a combination of lifestyle, environmental, and biological factors. Men generally exhibit a higher prevalence of key behavioral risk factors, such as greater consumption of red and processed meats, higher alcohol intake, and a larger historical burden of smoking. From a biological standpoint, female sex hormones, particularly estrogen, are believed to have a protective effect. Estrogen may exert this protection by modulating bile acid metabolism, reducing inflammation, and potentially influencing cellular proliferation pathways. This interplay between higher exposure to risk factors in men and the protective effects of hormones in women likely contributes to the increased cumulative risk and earlier onset of CRC observed in the male population [7].
G-protein-coupled receptors (GPCRs) are the largest superfamily of cell-surface proteins that translate extracellular signals, such as hormones, into intracellular responses [8, 9]. Their critical role in physiology makes them major drug targets, while their aberrant signaling is a known driver of cancer hallmarks like proliferation and metastasis [8]. Recently, numerous studies have suggested that leucine-rich repeat-containing G-protein-coupled receptor 5 (LGR5) plays an important role in colorectal carcinogenesis and is associated with poor prognosis in patients with CRC [10, 11]. LGR5 was originally identified as a paired receptor of the protein G orphan (GPCR), which is a subfamily of glycoprotein hormone receptors and contains a large extracellular domain with 17 leucine-rich repetitions and a seven-transmembrane domain [12, 13]. LGR5 is also known as GPR49, a Wnt signaling target that is associated with carcinogenesis and tumor invasion in CRC [10, 14].
LGR5 could be a more accurate marker of cancer stem cells (CSC) in colorectal cancer (CRC) [13, 15-17]. Jiang et al (2016) reported that high expression of LGR5 was associated with poor overall survival (OS) in CRC patients (odds ratio [OR] = 2.01, 95% confidence interval [CI] 1.16–3.47, p = 0.01, random model) [10].
However, several other studies found that an increase in the expression of LGR5 was associated with improved prognosis [10, 18, 19]. In addition, a previous study showed no association between LGR5 expression and poor clinical outcomes in patients with CRC [13]. Such discrepancies across studies suggest that the prognostic and clinical value of LGR5 in CRC patients may be limited [10]. Thus, the use of LGR5 as a prognostic indicator in CRC patients has became controversial. Insufficient sample sizes, among other factors, has likely resulted in contradictory results from other clinical studies [13]. In an attempt to clarify the prognostic value of LGR5 in CRC, we designed the current study to assess the association between LGR5 expression and OS in patients with colorectal cancer.
Methods
This study was an analytical observational review with a cross-sectional research design and a retrospective approach that was conducted from August 2023 to February 2024. The samples included in the study were obtained from patients diagnosed with colorectal cancer who were admitted to Dr. Wahidin Sudirohusodo General Hospital and the Hasanuddin University hospital, Makassar, Indonesia. All participants had undergone a total resection between 2019 and 2020, and their histopathological samples were investigated for LGR5 status at the Anatomical Pathology Laboratory of the Wahidin Sudirohusodo General Hospital and Hasanuddin University networking hospital, Makassar, and were selected using the consecutive sampling method. Immunohistochemical (IHC) Detection of LGR5
Formalin- fixed, paraffin- embedded ( FFPE) tissue sections (4 μm thickness) were subjected to immunohistochemical staining to evaluate LGR5 expression. The slides were first deparaffinized in xylene and rehydrated through graded alcohols to distilled water. Antigen retrieval was performed using citrate buffer (pH 6.0) in a pressure cooker for 10 minutes. Endogenous peroxidase activity was blocked by incubating the slides in 3% hydrogen peroxide for 10 minutes at room temperature.
The sections were incubated overnight at 4°C with a rabbit polyclonal anti-LGR5 primary antibody (Abcam, catalog no. ab75850) at a dilution of 1:100. On the following day, the slides were incubated with a secondary biotinylated antibody, followed by a streptavidin– horseradish peroxidase complex. Visualization was achieved using 3,3′-diaminobenzidine (DAB) as the chromogen, and hematoxylin was used for counterstaining.
LGR5 expression was evaluated semi-quantitatively by two independent pathologists blinded to clinical data. An immunoreactivity score (IRS) was calculated by multiplying the staining intensity (0 = none, 1 = weak, 2 = moderate, 3 = strong) by the percentage of positive cells (0 = <10%, 1 = 10–25%, 2 = 26–50%, 3 = >50%).
The median IRS value was used to dichotomize cases into high or low LGR5 expression categories for subsequent statistical analysis.
Statistical Analysis
Statistical analyses were conducted using SPSS® software (version 21.0; IBM Corp., Armonk, NY). Categorical variables were analyzed using the Chi-square test or Fisher’s exact test, as appropriate. Kaplan–Meier survival curves were constructed to evaluate overall survival, and the log-rank test was used to assess differences between groups. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated. A p-value < 0.05 was considered statistically significant.
Results
Association between LGR5 and colorectal cancer
Overall, 30 colorectal cancer patients were included in the analysis. The study evaluated the relationship between LGR5 and OS based on the following parameters: age, sex, tumor location, tumor stage, and histopathological grading. Results of the association between LGR5 and colorectal cancer are shown in Table 1.
| Variable | LGR-5 Expression (%) | p-value | ||
| High (n=8) | Low (n=22) | |||
| Sex | 1 | |||
| Male | 6 (75.0) | 15 (68.2) | ||
| Female | 2 (25.0) | 7 (31.8) | ||
| Age (years) | 1 | |||
| < 40 | 1 (12.5) | 4 (18.2) | ||
| > 40 | 7 (87.5) | 18 (81.8) | ||
| Tumor Stage | 0.914 | |||
| Stage II | 1 (12.5) | 2 (9.1) | ||
| Stage III | 4 (50.0) | 10 (45.5) | ||
| Stage IV | 3 (37.5) | 10 (45.5) | ||
| Histopathological Grade | 0.25 | |||
| Well-differentiated | 2 (25.0) | 1 (4.5) | ||
| Moderate differentiated | 4 (50.0) | 15 (68.2) | ||
| Poorly differentiated | 2 (25.0) | 6 (27.3) | ||
| Tumor Location | 0.667 | |||
| Ascending | 1 (12.5) | 6 (27.3) | ||
| Transverse | 1 (12.5) | 4 (18.2) | ||
| Descending | 4 (13.3) | 7 (31.8) | ||
| Sigmoid | 2 (50.0) | 3 (13.6) | ||
| Rectum | 0 (0.0) | 2 (9.1) |
Note: LGR5 expression was categorized as "High" or "Low" based on the median immunoreactivity score obtained through IHC analysis.
A summary of the results in Table 1 are shown in Table 2.
| Variable | p-value |
| Sex | 1 |
| Age | 1 |
| Tumor Stage | 0.001 |
| Histopathological Grade | 0.194 |
| Tumor Location | 0.212 |
From the summary of the outputs shown in Table 2, it can be concluded that no association between LGR5 (high and low expression) to age, sex, tumor location, tumor stage, and histopathological grading was observed (all p-values > 0.05).
Association between OS of patients with colorectal cancer and LGR5 expression.
The Kaplan–Meier survival plot shows the overall survival probability of colorectal cancer patients stratified by LGR5 expression (Figure 1).
Figure 1. Kaplan–Meier Curve of Overall Survival Based on LGR5 Expression.
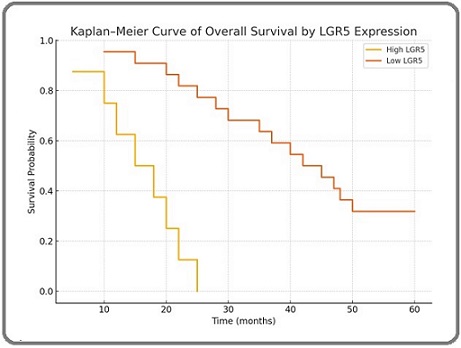
Patients with low LGR5 expression (n=22) exhibited a longer survival trend compared to those with high LGR5 expression (n=8), although the difference did not reach statistical significance (log-rank p = 0.418).
A summary of the test results described above are provided in Table 3.
| Variable | p-value |
| Sex | 1 |
| Age | 1 |
| Tumor Stage | 0.001 |
| Histopathological Grade | 0.194 |
| Tumor Location | 0.212 |
| LGR5 | 0.643 |
Note: Statistical significance was assessed using chi-square or Fisher’s exact test
The analysis revealed a statistically significant association between tumor stage and overall survival (OS) in colorectal cancer patients (p = 0.0011), with early-stage patients demonstrating better 5-year survival outcomes. In contrast, no significant associations were observed between OS and other variables, including sex, age, histopathological grade, tumor location, or LGR5 expression (all p > 0.05). Although patients with low LGR5 expression showed a trend toward better survival, the difference was not statistically significant (Table 3).
Discussion
CRC represents a major global health burden and is among the leading causes of cancer-related mortality worldwide [20, 21]. In Indonesia, the burden of CRC continues to rise, with increasing incidence and mortality particularly among older adults. Despite progress in early detection and therapeutic strategies, long-term survival outcomes remain suboptimal, especially in patients with advanced disease [22]. This reality underscores the urgent need for novel prognostic biomarkers that can better stratify risk and guide personalized therapeutic approaches.
Recent attention has focused on the role of cancer stem cells (CSCs) in driving tumorigenesis, treatment resistance, recurrence, and metastasis [11]. One such marker, LGR5, has emerged as a putative CSC biomarker in colorectal cancer [23, 24]. LGR5 is a known downstream target of the Wnt/β-catenin signaling pathway, which is pivotal in regulating stemness, cell proliferation, and tumor progression [23, 25]. Although LGR5 has shown promise as a prognostic and therapeutic target in experimental studies, clinical evidence regarding its prognostic value remains inconsistent and controversial.
In this retrospective study of 30 patients with histologically confirmed colorectal adenocarcinoma, we assessed LGR5 expression using IHC and categorized patients into high and low expression groups based on a median IRS threshold. The survival outcome was measured using the Kaplan–Meier method, and associations were statistically analyzed using chi-square or Fisher’s exact tests.
The findings demonstrated no statistically significant association between LGR5 expression and overall survival (p = 0.418). Similarly, no significant associations were observed between LGR5 expression and clinicopathological characteristics such as age, sex, tumor location, histological grade, or cancer stage (all p > 0.05). However, a significant correlation was found between tumor stage and OS (p = 0.0011), suggesting that advanced stage disease strongly predicts poor prognosis, as expected. Histological grade also showed a trend toward significance but did not reach statistical threshold (p = 0.1943).
Our results suggest that LGR5 expression may not be an independent prognostic marker in colorectal cancer within this study population. These findings are consistent with a retrospective study by Kim et al. (2018) [26], who reported no significant association between LGR5 expression and survival outcomes in 337 patients with CRC. Additionally, de Sousa e Melo et al. (2017) [27] observed that LGR5+ cell ablation reduced tumor growth in experimental models but did not lead to complete regression, supporting the notion that LGR5 expression alone may not fully account for tumor aggressiveness or patient outcome.
Conversely, multiple studies have shown conflicting results. A meta-analysis by Jiang et al. (2016) [10] involving over 2,600 CRC patients found that high LGR5 expression was significantly associated with poor OS and disease-free survival (DFS), as well as with adverse clinicopathological features such as lymph node metastasis and distant spread. Chen et al. (2014)
[13] also concluded that elevated LGR5 levels correlate with worse survival outcomes. These discrepancies may arise from differences in study design, ethnicity, IHC scoring systems, antibody specificity, sample sizes, or the biological heterogeneity of colorectal cancer itself.
Interestingly, although our findings did not reach statistical significance, we observed a non-significant trend in which patients with low LGR5 expression had longer survival compared to those with high expression. This trend is biologically plausible, as LGR5-positive CSCs have been implicated in promoting chemoresistance and tumor regeneration following therapy. Thus, it remains possible that LGR5 plays a role in modulating long-term outcomes, but larger prospective studies are needed to confirm this hypothesis.
The only variable that demonstrated a significant association with overall survival was tumor stage, which aligns with existing evidence that advanced stage at diagnosis is the most powerful predictor of CRC prognosis. Our results support continued emphasis on early detection and stage-based stratification in clinical practice.
Limitations of this study. First, the sample size was relatively small (n = 30), which may limit the statistical power to detect subtle but clinically meaningful associations. Second, the retrospective design introduces inherent selection and information biases. Third, IHC analysis is semi-quantitative and may be influenced by inter-observer variability, despite the use of blinded pathologists. Fourth, the follow-up period was limited, and OS was assessed in binary categories (3-year vs 5-year), which may not fully capture survival dynamics over time.
Lastly, we did not perform functional analyses of LGR5-positive versus LGR5-negative cell populations to directly assess their biological behavior, such as proliferation, chemoresistance, or metastatic potential. These limitations warrant caution in interpreting the findings and highlight the need for larger, multicenter prospective studies, ideally incorporating molecular and functional validation of CSC markers like LGR5.
In conclusion, in this study, no statistically significant association was found between LGR5 expression levels and overall survival or major clinicopathological features in CRC patients. Although a trend toward improved survival in patients with low LGR5 expression was observed, this did not reach statistical significance. Importantly, this study did not include healthy controls; therefore, conclusions regarding whether LGR5 is differentially expressed between colorectal cancer and non-cancerous tissue cannot be drawn. Our findings are limited to evaluating the prognostic value of LGR5 expression within colorectal cancer cases and should not be interpreted as evidence of LGR5’s irrelevance in colorectal tumorigenesis. Further studies incorporating non-cancerous control tissues and mechanistic analyses are warranted to clarify the diagnostic and biological significance of LGR5 in CRC.
Acknowledgments
None.
Conflicts of interest
The authors declare no conflict of interest.
Informed consent
Informed consent was obtained from all participants in the study.
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Hasanuddin University, Faculty of Medicine accepted this study following a review of the protocol (Reference Number: 120/UN4.6.5.31/PP36/2021).
Authors’ contributions
EJS, WS, MIK, MP, PRI, JH, and MF wrote the manuscript and participated in the study design. EJS, WS, MIK, and MP drafted and revised the manuscript. MP, PRI, JH, and MF critically reviewed the manuscript. EJS and JH performed bioinformatics analyses and revised the manuscript. All authors contributed equally to the manuscript, read and approved the final version of the manuscript.
Availability of data and materials
Data and materials are available from the corresponding author upon request.
References
- IARC Working Group on the Evaluation of Cancer-Preventive Interventions. Colorectal cancer screening. Lyon (FR) 2019.
- The Relationship Between Histopathological Grading and Metastasis in Colorectal Carcinoma Patients Minhajat R, Benyamin , Miskad . Nusantara Medical Science Journal .2021;:51-60. CrossRef
- Correlation of interleukin-6 and C-reactive protein levels in plasma with the stage and differentiation of colorectal cancer: A cross-sectional study in East Indonesia Hidayat F, Labeda I, Sampetoding S, Pattelongi IJ , Lusikooy RE , Dani MI , Kusuma MI , et al . Annals of Medicine and Surgery.2021;62. CrossRef
- Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL , Soerjomataram I, Jemal A. CA: A Cancer Journal for Clinicians.2024;74(3). CrossRef
- Global Cancer Observatory. Indonesia, Lyon, France: International Agency for Research on Cancer 2022.
- Sex Differences in Colorectal Cancer Survival: Population-Based Analysis of 164,996 Colorectal Cancer Patients in Germany Majek O, Gondos A, Jansen L, Emrich K, Holleczek B, Katalinic A, et al . PLoS ONE.2013;8(7). CrossRef
- A review of sex-related differences in colorectal cancer incidence, screening uptake, routes to diagnosis, cancer stage and survival in the UK White Al, Ironmonger L, Steele RJC , Ormiston-Smith N, Crawford C, Seims A. BMC Cancer.2018;18(1). CrossRef
- G protein-coupled receptors (GPCRs): advances in structures, mechanisms and drug discovery Zhang M, Chen T, Lu X, Lan X, Chen Z, Lu S. Signal Transduction and Targeted Therapy.2024;9(1). CrossRef
- GPCRs in Intracellular Compartments: New Targets for Drug Discovery Fasciani I, Carli M, Petragnano F, Colaianni F, Aloisi G, Maggio R, Scarselli M, Rossi M. Biomolecules.2022;12(10). CrossRef
- Lgr5 expression is a valuable prognostic factor for colorectal cancer: evidence from a meta-analysis Jiang Y, Li W, He X, Zhang H, Jiang F, Chen Z. BMC Cancer.2015;15(1). CrossRef
- The prognostic value of leucine-rich repeat-containing G-protein (Lgr5) and its impact on clinicopathological features of colorectal cancer Gzil A, Zarębska I, Jaworski D, Antosik P, Durślewicz J, Maciejewska J, et al . Journal of Cancer Research and Clinical Oncology.2020;146(10). CrossRef
- Lgr5 in cancer biology: functional identification of Lgr5 in cancer progression and potential opportunities for novel therapy Xu L, Lin W, Wen L, Li G. Stem Cell Research & Therapy.2019;10(1). CrossRef
- Prognostic Value of LGR5 in Colorectal Cancer: A Meta-Analysis Chen Q, Zhang X, Li W, Ji Y, Cao H, Zheng P. PLoS ONE.2014;9(9). CrossRef
- Identification of overexpression of orphan G protein-coupled receptor GPR49 in human colon and ovarian primary tumors McClanahan T, Koseoglu S, Smith K, Grein J, Gustafson E, Black S, Kirschmeier P, Samatar AA . Cancer Biology & Therapy.2006;5(4). CrossRef
- Lgr5 is a potential marker of colorectal carcinoma stem cells that correlates with patient survival Wu X, Xi H, Chen L. World Journal of Surgical Oncology.2012;10(1). CrossRef
- Lgr5+CD44+EpCAM+ Strictly Defines Cancer Stem Cells in Human Colorectal Cancer Leng Z, Xia Q, Chen J, Li Y, Xu J, Zhao E, Zheng H, Ai W, Dong J. Cellular Physiology and Biochemistry.2018;46(2). CrossRef
- Emerging role for leucine-rich repeat-containing G-protein-coupled receptors LGR5 and LGR4 in cancer stem cells Goidts V, Nakata S, Phillips E. Cancer Management and Research.2014. CrossRef
- Leucine‑rich repeat‑containing G protein‑coupled receptor 5 and CD133 expression is associated with tumor progression and resistance to preoperative chemoradiotherapy in low rectal cancer Harada Y, Kazama S, Morikawa T, Murono K, Yasuda K, Otani K, Nishikawa T, et al . Oncology Letters.2017. CrossRef
- Leucine-rich repeat-containing G-protein-coupled receptor 5 is associated with invasion, metastasis, and could be a potential therapeutic target in human gastric cancer Xi H Q, Cai A Z, Wu X S, Cui J X, Shen W S, Bian S B, Wang N, et al . British Journal of Cancer.2014;110(8). CrossRef
- Colorectal Cancer: Epidemiology, Risk Factors, and Public Health Strategies Matsuda T, Fujimoto A, Igarashi Y. Digestion.2025;106(2). CrossRef
- Colorectal cancer: A health and economic problem Klimeck L, Heisser T, Hoffmeister M, Brenner H. Best Practice & Research Clinical Gastroenterology.2023;66. CrossRef
- Colorectal cancer: Recent advances in management and treatment Fadlallah H, El Masri J, Fakhereddine H, Youssef J, Chemaly C, Doughan S, Abou-Kheir W. World Journal of Clinical Oncology.2024;15(9). CrossRef
- LGR5: An emerging therapeutic target for cancer metastasis and chemotherapy resistance Wang W, Lokman NA , Barry SC , Oehler MK , Ricciardelli C. Cancer and Metastasis Reviews.2025;44(1). CrossRef
- Colonic Stem Cells Expression of Lgr5 and CD133 Proteins as Predictive Markers in Colorectal Cancer among Egyptian Patients Rosiq S, Hammam O, Abdelalim A, Anas A, Khalil H, Amer M. Open Access Macedonian Journal of Medical Sciences.2018;6(6). CrossRef
- LGR5 regulates gastric adenocarcinoma cell proliferation and invasion via activating Wnt signaling pathway Wang X, Wang X, Liu Y, Dong Y, Wang Y, Kassab MA , Fan W, Yu X, Wu C. Oncogenesis.2018;7(8). CrossRef
- Clinical relevance of Lgr5 expression in colorectal cancer patients Kim YJ , Kang DH , Song GJ , Ahn TS , Son MW , Lee MS , Baek M. Korean Journal of Clinical Oncology.2018;14(2). CrossRef
- A distinct role for Lgr5+ stem cells in primary and metastatic colon cancer De Sousa E Melo F, Kurtova AV , Harnoss JM , Kljavin N, Hoeck JD , Hung J, Anderson JE , et al . Nature.2017;543(7647). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2025
Author Details