Cost Analysis of Oral Cancer Treatment in a Tertiary Care Referral Center in India
Download
Abstract
Introduction: As much as the number of oral cancer patients is a heavy burden to the health care system in India, so much is the economic burden to the patient and the relatives, especially in India where most do not have any financial cover for their medical expenditure. Objectives: To find out the approximate cost of treatment of oral cancer through various modalities, and calculate the proportion of direct and indirect expenses, and then identify the factors which would increase the indirect expenses so as to come up with recommendations which will reduce the indirect cost thereby reducing the financial burden to the patient.
Methods: A retrospective observational study was done in a tertiary care center for cancer treatment and the direct cost (medical expense), indirect cost (non-medical expense) incurred by the patients, their economic status and source of fund for payment of the expenses were obtained.
Results: The proportion of indirect cost was about 38.72% of the total cost for patients who underwent a single modality treatment with surgery, around 34.73% for a combination treatment with surgery and RT (Radiotherapy), about 79.63% for treatment with conventional Radiotherapy without surgery and about 49.61% for treatment with IMRT (Intensity Modulated Radio Therapy) without surgery. Availability of financial aid or cover is abysmally poor. The rate of discontinuance of treatment is also very high according to this study.
Conclusion: The proportion of the indirect cost is very high and the total expenditure can be reduced by approximately 30% by following measures discussed in this article.
Introduction
Oral cancers usually tobacco-related are one of the most common malignancies(Subramanian et al. 2009) prevalent in India for which patients travel long distances for treatment(Nair et al. 2013). The disease negatively impacts the quantity and quality of life, and the financial burden is too much to bear for most of the patients. This financial burden is more cumbersome in India as the proportion of the indirect cost related to it is very high and needs to be brought down for the effective availability of treatment to the socioeconomically underprivileged group.
Materials and Methods
This was done as a retrospective observational study. The proposal for this study was sent to Heads of all the departments involved and ethical approval was obtained.
Patients who underwent a biopsy in this tertiary care center for a lesion in the oral cavity and reported as malignancy were included in the study. The period of study was 8 months from Oct 2012 to May 2013.
The boundaries of Oral cavity was defined as all structures behind the vermilion border of lip to the line of circumvallate papillae on the dorsum of the tongue posteriorly (the anatomical landmark separating the anterior 2/3rd and the posterior 1/3rd of the tongue), the pterygoid mandibular raphe laterally, and junction of hard and soft palate on the superior aspect.
Information regarding non-medical expenses was gathered from the patients or their relatives through phone calls. They were asked as to how much they had spent on travel, what was the cost of their lodging and boarding for a day, how many days they had to stay in lodges around the hospital for treatment and how many persons accompanied the patient. Information regarding their economic status like the nature of the job, their monthly income and means by which the treatment expense was met were also collected. The medical expenses of the patients were collected from the accounts department of the institution.
Results
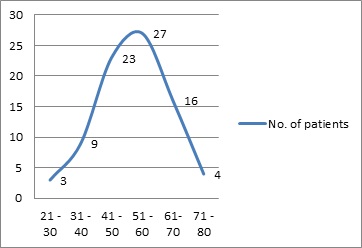
The number of patients in the study was 82. At the time of presentation, the patients were in their third decade to the eight decades of life and the number of patients in each decade is given in (Fig. 1), with the almost equal proportion of male and female patients.
Figure 1 :Distribution across decades
Distribution
Patients had traveled a very long distance to be treated. There were 27 patients from Tamil Nadu (the state in which the institution is present) and Pondicherry, 3 from Kerala and 6 from Andhra Pradesh which are the neighboring states. There were 20 from West Bengal, 10 from Jharkhand, 2 from Madhyapradesh, 1 each from Bihar and Uttarpradesh. From the northeastern states, there were 6 from Assam, 2 from Tripura and 1 each from Meghalaya and Nagaland. There were 2 patients from the neighboring country Bangladesh. The patients who sought treatment from Tamil Nadu and surrounding states made up 47.5% and the other 52.5 % were from the northern and northeastern states.
Dropouts
Out of the 82 patients who underwent biopsy and were diagnosed with oral carcinoma, only 45 patients completed their treatment. Single modality treatment was done for 25 patients of whom 12 underwent surgery and 13 patients received radiotherapy and 18 patients underwent a combined treatment of surgery and radiotherapy as given in Tabl 1. Out of the 37 patients who discontinued treatment through the process, 12 of them dropped out of the treatment process after biopsy and 25 patients discontinued treatment after multidisciplinary tumor board treatment planning. The sad finding that we noted in this study was that 6 patients among the dropouts who underwent biopsy did not even report back to collect their biopsy reports.
| Modality of treatment | Surgery | Radiotherapy | Surgery and Radiotherapy | Palliative treatment |
| No of patients out of 45 | 12 | 13 | 18 | 2 |
Cost
The total expenditure of each of the 45 patients who completed the treatment was categorized under two categories, as a medical expense or direct cost and non-medical expense or indirect cost.
Medical expense (Direct cost) involved the total amount that a patient had spent within the hospital for investigations, medicines, treatment charges, and inpatient charges The amount each patient had spent on investigations like radiographs, blood investigations, biopsies, and pre-treatment clearance was about 13,303Rupees. In this study, we found that some patients who never underwent any kind of treatment for their malignancy had spent about 7832Rs on investigations alone. Patients who underwent surgery alone as the modality of treatment had spent around 1, 37,525Rupees, and if it was followed by radiotherapy (RT) as the second modality, then the expenditure rose to around 2, 37,357Rupees, excluding non-medical expenses. Patients who had only radiotherapy (RT) as the treatment modality, had spent around 29,782Rupees for conventional RT and for those who opted for three dimensional (3D) or Intensity Modulated Radiotherapy (IMRT) the cost was around 1,18,245Rupees, excluding non-medical expenses. (Tabl 2).
| Modality of Treatment | Surgery | Conventional Radiotherapy | 3D or IMRT | Surgery with Radiotherapy |
| Average total Cost in Rupees | 2,10,765 | 1,46,182 | 2,34,645 | 3,87,357 |
| Average Direct cost | 1,37,565 | 29,782 | 1,18,245 | 2,37,357 |
| Average Indirect cost | 73,200 | 1,16,400 | 1,16,400 | 1,50,000 |
| The proportion of the Indirect cost | 34.73% | 79.63% | 49.61% | 38.72% |
Non-medical expense (Indirect cost) is the money spent for purposes other than treatment but indirectly related to treatment like travel, boarding, and lodging including the amount spent for the accompanying persons. Though indirect cost is a much broader entity, which also includes the loss of income to the accompanying persons due to their absence from work, this has not been included in the indirect cost in this study.
In our study, we found that the average travel cost was about 2000 rupees per person. Almost every patient had been accompanied by 2 persons so calculating for three persons the travel cost amounted to about 6000 rupees. Food and lodging had cost about 420 rupees for a person every day which amounted to about 1200 rupees including those who had accompanied the patient. The duration of staying away from home for the patients who had been treated by Surgery alone was approximately 56 days, for patients who had received Radiotherapy alone was about 92 days and for patients who underwent Surgery and Radiotherapy, it was around 120 days. With the above available data of the cost of travel, cost of living per day and the duration of stay, we calculated the average indirect cost for the various modalities of treatment and found that it was an abnormally huge proportion as given in Tabl 2.
Socioeconomic background
The nature of employment of the patients who had completed treatment covered the entire spectrum. There were patients who were unemployed, self-employed, patients with private jobs, government jobs and a very few wealthy businessmen. (Tabl 3). About 54% of the patients had a monthly family income of less than 10,000Rs, around 48.5% of the patients had income between 10,000 – 20,000Rs and about 1.5% had more than 20,000Rs. Considering their income the cost of treatment is unaffordable for most the patients. This study reveals that 45% of the patients had met the expense themselves from their earnings and savings or by selling, mortgaging their properties and 38% had borrowed to meet the expenses (Tabl 4).
| Nature of employment | Daily Wages | Farmer | Self-employed | Private sector | Government employed | Retired | Business | Unemployed |
| No. of patients | 12 | 9 | 1 | 7 | 4 | 8 | 2 | 2 |
| Source of fund | Self-paying/ Selling or mortgaging properties | Borrowing | Government schemes | Medical Insurance | NGO funds/ Institution’s funds |
| Percentage of patients | 45% | 38% | 10% | 3% | 4% |
Discussion
The number of patients who had not completed treatment, which was 37 out 82 (45.12%), is quite a large proportion. In this group, 25 out of 37 had attended the MDT (multi-disciplinary tumor board) planning but had not commenced the planned treatment. When they were inquired about the reasons for not starting the treatment most of them said that “it was due to the prolonged waiting period for surgery”, and some said that they “could not afford the treatment cost” and a few patients replied that they had “wanted to go to a center close to their home for radiotherapy, as the expected period of stay away from home would have been a prolonged one.” All these three reasons had one thing in common which was financial restraint and further analysis revealed that it was the indirect cost or non-medical expense that these patients were not able to bear.
In India, the medical expenses are often met either by self-payment or borrowings(Nair et al. 2013; Wani et al. 2013). In our study, 83% of the patients had met the expenses by this method as seen in (Tabl 4). The profession of many of these patients was daily wage workers, farmers or some kind of self-employment. Their long duration of staying away from home translated to an increased proportion of indirect expenses and had also resulted in the loss of income for the patients and as well for the accompanying persons for as many days.
For a patient who underwent surgery as the only treatment modality, the first 37 days of stay had been spent for investigations, clearance, and Multi-Disciplinary Tumour board treatment planning and it also included a few days which was spent as the waiting period for Surgery. (Song et al. 2017) About 52.5% of the patients in this study were from locations very far away from the treating center. If these patients had done the preliminary investigations at a health care center close to their homes, had attended the Multi-Disciplinary Tumour board planning via teleconference and then had reached the tertiary care cancer center in time for treatment, on an average they could have saved 1200 Rupees (cost of living per day), for a minimum of 30 days which is about 36,000Rupees out of their non-medical expenses. This amount is about 17% of the total expenditure that they had spent, and in addition, the accompanying persons could have earned their daily wages for at least half those many days. But the above-said kind of treatment planning requires a centralized cancer registry where investigations and reports are updated real-time which is accessible all over India.
The cost of cancer treatment is a huge burden considering the prevailing economic status of patients in India(Wani et al. 2013). The investigations, various treatment modalities, and drugs are too costly for a common man and spending from their own pocket is impossible for many which often lead to discontinuance or dropouts from the treatment. Some kind of funding or medical insurance is the dire need for cancer treatment in India(Magrath et al. 2010). In our study, we found that only 17% of the patients had financial support from Government schemes and other funds, which was very less as found out by other studies also. This proves that there is a great need for funding cancer treatment in India(Magrath et al. 2010; Ray 2013).
The Indian sub-continent is a vast land and patients in our study had traveled long distances for treatment. Traveling long distances is one of the hardships faced in the treatment of cancer(Nair et al. 2013). During the initial phases of treatment which involves investigations and diagnosis which are usually done as Out-Patient services, in this study only 26 of the 82 patients which are 31.7% patients could commute daily to their home after OP (Out Patient), while the other 68.3% of patients owing to the distance from their homes had to stay in lodges around the hospital resulting in increased indirect costs. Some patients as seen from this study choose to get treatment close to their home after having done all the investigations. When patients change treating centers there are unwanted repetitions of the investigations which increase the direct and indirect costs. Though there are several cancer registries(Coelho 2012; Nandakumar et al. 2005) we do not have a centralized cancer registry for India. A centralized cancer registry would reduce repetitions of investigations resulting in unwanted duplication of direct cost and also cut down the indirect cost associated with it. More tertiary cancer care centers which are also geographically requisitioned across India would reduce the travel, boarding and lodging costs.
Though the cost calculation of direct cost or medical expenses done in this study is from the information obtained from patients being treated in one institution, it will not very much from the estimates nationwide. The indirect cost or non-medical expenses can vary to some extent depending on the place of treatment as boarding and lodging can become costlier in bigger cities which will only further increase the proportion of indirect costs.in Conclusion,With the projections for cancer incidence(Dsouza, Murthy, and RY Aras 2013) and the economic burden of cancer population in India for the next few years is very high(DSouza, Murthy, and RY Aras 2013; Ramnath Takiar, Deenu Nadayil, and A Nandakumar 2010), we need to create awareness about the ill effects of tobacco use and prevent oral cancer. We also need to reduce the economic burden involved in the treatment of oral cancers. In our study, we have found that the indirect cost or non-medical expense involved in the treatment of oral cancers is very high and is a major factor for discontinuing the treatment, so steps should be taken to reduce the indirect cost associated with the treatment of oral cancer.
Recommendations
Staying away from home for long durations in the treatment of cancer and its repercussions is the biggest difficulty faced by the patients and relatives. The following recommendations as discussed previously will greatly reduce this and lessen the financial burden in cancer treatment.
- Developing a Centralised Oral cancer registry for India.
- Starting more tertiary care centers for cancer treatment which is geographically requisitioned across India.
- To make available Funding schemes and agencies for cancer treatment in India.
- Putting up Awareness clinics, cancer screening, and prevention camps.
Acknowledgments
We acknowledge the support given by the accounts department of CMC Vellore, in helping us collect the required information and also thank the involved patients for their cooperation.
Conflict of interest – Nil.
References
[1]. Coelho, Ken Russell.Challenges of the Oral Cancer Burden in India. Journal of Cancer Epidemiology .2012.
[2]. DSouza, Neevan DR, NS Murthy, and RY Aras.Projection of the Burden of Cancer Mortality for India, 2011-202. Asian Pacific Journal of Cancer Prevention.2013;14(7):4387–92.
[3]. Dsouza, Neevan DR, NS Murthy, and RY Aras.Projection of Cancer Incident Cases for India -Till 2026. Asian Pacific Journal of Cancer Prevention.2013;14(7): 379–86.
[4]. Magrath, Ian, Pierre Bey, Aziza Shad, Simon Sutcliffe. Cancer Funding in Developing Countries: The next Health-Care Crisis?. The Lancet .2010;376(9755):1827.
[5]. Nair, Kesavan Sreekantan, Sherin Raj, Vijay Kumar Tiwari,Lam Khan Piang. Cost of Treatment for Cancer: Experiences of Patients in Public Hospitals in India. Asian Pacific Journal of Cancer Prevention.2013;14(9): 5049–54.
[6]. Nandakumar, Ambakumar, Prakash Chandra Gupta, Paleth Gangadharan, Rudrapatna Narayanrao Visweswara, Donald Maxwell Parkin. Geographic Pathology Revisited: Development of an Atlas of Cancer in India. International Journal of Cancer.2005;116 (5):740–54.
[7]. Ramnath Takiar, Deenu Nadayil, and A Nandakumar. Projections of Number of Cancer Cases in India (2010-2020) by Cancer Groups. Asian Pacific Journal of Cancer Prevention.2010;11(4):1045-49.
[8]. Ray, B. Auditing Costs of Intensive Care in Cancer Patients in India: A New Area Explored. Indian Journal of Critical Care Medicine : Peer-reviewed, Official Publication of Indian Society of Critical Care Medicine .2013;17(5):269–70.
[9]. Song, Huan, Fang Fang, Unnur Valdimarsdóttir, Donghao Lu, Therese M.-L. Andersson, Christina Hultman, Weimin Ye, et al.Waiting Time for Cancer Treatment and Mental Health among Patients with Newly Diagnosed Esophageal or Gastric Cancer: A Nationwide Cohort Study. BMC Cancer.2017;17(1):2.
[10]. Subramanian, Sujha, Rengaswamy Sankaranarayanan, Bela Bapat, Thara Somanathan, Gigi Thomas, Babu Mathew, Jissa Vinoda, and Kunnambath Ramadas.Cost-Effectiveness of Oral Cancer Screening: Results from a Cluster Randomized Controlled Trial in India. Bulletin of the World Health Organization.2009;87(3):200–206.
[11]. Wani, MohammadAshraf, Sa Tabish, FarooqA Jan, NazirA Khan, Za Wafai, and Kk Pandita. Cost Analysis of In-Patient Cancer Chemotherapy at a Tertiary Care Hospital. Journal of Cancer Research and Therapeutics.2013;9(3):397.
License
Copyright
© ,
Author Details