Evaluation of Microorganisms in Cervical Smears: A Single Institutional Experience
Download
Abstract
Human papilloma virus (HPV) and herpes simplex virus (HSV) are common microorganisms investigated in the diagnosis of cervical abnormalities, however other microorganisms have received less attention. This study aimed to identify different microorganisms present in cervical smears as well as to determine the association between those microorganisms and cervical abnormalities. A retrospective study was conducted from January 2008 to December 2012, evaluating the presence of microorganisms in cervical smears. The association between the microorganisms and cervical abnormalities was studied by using the odds ratio and relative risk tests. A total of 7112 cervical smears were analyzed. The mean age of the patients was 39.13 years (range 17 – 80). Bacteria were the most common microorganism but it showed no association with cervical abnormalities. HPV, HSV and Trichomonas vaginalis are the least common but showed a positive association with a relative risk of 16.59, 7.23 and 1.15 respectively. Bacteria and fungi are the most common microorganisms present in cervical smears but they are not associated with cervical abnormalities whereas HPV and HSV are less common but they are associated with cervical abnormalities.
Introduction
Cancer in the past, present and in the future continues to be a critical concern for all. In 2012, there were 14.1 million new cancer cases, 8.2 million cancer deaths and cervical cancer alone caused death of 265,700 women worldwide [1]. The main cause of cervical cancer is not known but infections with human papilloma virus (HPV) and to a lesser extent herpes simplex virus (HSV) are highly associated with cervical cancer [2][3][4]. Other risk factors include long duration of oral hormonal contraceptives, cigarette smoking, vitamin deficiency and immunosuppression [5].
Apart from those two viruses, other microorganisms have received less attention. The relationships between microorganisms and different types of cervical abnormalities might lead to consider that those microorganisms could be used as possible diagnostic indicators. This association between microorganisms and cervical abnormalities is also important to distinguish between normal flora and pathogenic microorganisms. Thus, the aim of this retrospective study was to identify different microorganisms present in cervical smears as well as to determine the association between those microorganisms and cervical abnormalities.
Materials and Methods
A retrospective review of cervical smears over a period of five years from January 2008 to December 2012 was performed. The records of all patients who had cervical smears were included. Usually for each cervical smear, two slides were fixed in 95% ethanol and then stained with Pap method. Trichomonas is usually identified by the presence of eosinophilic granules in the cytoplasm, the nucleus is pale, vesicular and eccentrically located, mature squamous cells with slightly enlarged, dark nuclei and small perinuclear halos. Occasionally many lymphocytes and mast cells may be seen. Flagella are sometimes seen. HPV is identified by the presence of koilocytosis whereas HSV by the presence of margination, moulding and multinucleation. Cytological diagnosis was classified into six categories: no malignancy which includes unsatisfactory, normal, inflammatory and benign changes, borderline nuclear changes, mild dyskaryosis, moderate dyskaryosis, severe dyskaryosis and carcinoma. This study was conducted after an approval from the Medical Research Committee and Ethics Committee. Statistical analysis was performed using SPSS (version 19.0) statistical package (SPSS Inc., Chicago, IL, USA). The association between the microorganisms and cervical cancer was studied by using the odds ratio (OR) and relative risk (RR) tests.
Results
A total of 7112 cases was found in this study, 93.1% were negative for cervical lesion and the remaining 6.9% were positive for different grades of cervical lesions. The mean age of the patients was 39.13 years (range 17 – 80). Women above 40 years are more affected than younger women with cervical lesions [Table 1].
| Grade of cervical lesion | Age Groups | Total | ||
| <21 | 21-40 | >40 | ||
| No malignancy | 51 94.4 % | 3918 94.6% | 2650 90.9 % | 6619 93.1 % |
| Borderline nuclear changes | 1 1.9 % | 104 2.5 % | 147 5.0 % | 252 3.5 % |
| Mild dyskaryosis | 2 3.7 % | 64 1.5 % | 59 2.0 % | 125 1.8 % |
| Moderate dyskaryosis | 0 0.0 % | 26 0.6 % | 21 0.7 % | 47 0.7 % |
| Severe dyskaryosis | 0 0.0 % | 24 0.6 % | 15 0.5 % | 39 0.5 % |
| Carcinoma | 0 0.0 % | 7 0.2 % | 23 0.8 % | 30 0.4 % |
| Total | 54 100 % | 4143 100 % | 2915 100 % | 7112 100% |
There are 6424 satisfactory samples (90.3%) for cytological diagnosis while only 688 (9.3%) showed unsatisfactory samples.
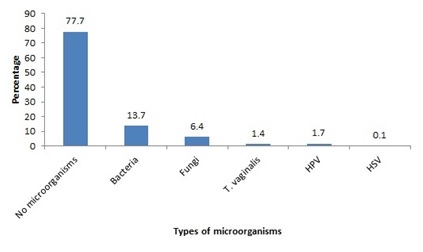
Bacteria were the most common microorganisms in cervical smears with 13.7% while HSV infection was rarely seen with 0.1% [Figure 1].
Figure 1. Frequency of microorganisms
For the sake of clarification, the six groups were categorized into two groups. First group is no cervical lesion group which includes unsatisfactory, normal, inflammatory and benign changes. The second group is cervical lesion group which includes borderline nuclear changes, mild, moderate and severe dyskaryosis and carcinoma. 90.0% of HPV cases were related to cervical lesion. Although HSV infection was rare, 50% of its cases were related to cervical lesion [Figure 2].
Figure 2. Microorganisms in normal and abnormal cervical smears
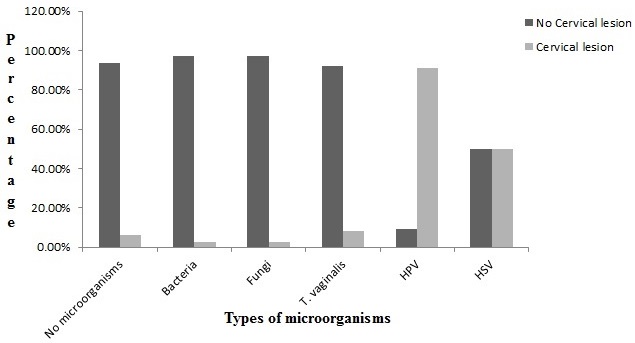
The relative risk (RR) of cervical cancer with HPV was 16.59. However, RR decreased less than one in case of bacteria and fungi. Trichomonas vaginalis and HSV both related to cervical lesion with a RR of 1.155 and 7.238 respectively [Table 2].
| Microorganisms | Odds Ratio | Relative Risk |
| Bacteria | 0.346 | 0.364 |
| Fungi | 0.348 | 0.365 |
| HPV | 172.533 | 16.594 |
| T. Vaginalis | 1.168 | 1.155 |
| HSV | 13.477 | 7.238 |
Discussion
The findings of this study show that bacteria and fungi are the most common microorganisms present in cervical smears with a percentage of 13.7% and 6.4%, respectively. However, these microorganisms have no significant association with cervical lesion as the relative risk (RR) is less than one. In cytopathology, Gram and Grocott's methenamine silver methods are not usually performed to demonstrate bacteria and fungi, respectively. Therefore, bacteria and fungi are not differentiated. Pap method, which is the routine staining method in cytopathology, stains bacteria and fungi when they present in large numbers and might miss them if they are scanty. The main benefit of using Pap stain as a routine stain in cytopathology is to differentiate between malignant, pre-cancerous and benign cells. In addition, other substances such as crystals, fibrin and pigments are stained [6]. Several studies showed that the demonstration of fungi, such as Candida albican, using microbiological culture is more sensitive than cervical Pap method [6][7][8]. In comparison, cervical smears have the advantage over microbiological culture in that bacteria and fungi and other microorganisms can be visualized in their natural habitat [9].
The presence of Trichomonas vaginalis (T. vaginalis) in cervical smears was less common. This study shows that only 0.4% were positive for T. vaginalis. The RR for T. vaginalis is 1.15, indicating a risk of developing a cervical lesion. The finding of this study is in line with other studies which collectively showed a true association between T. vaginalis infection and cervical lesion [10][11]. T. vaginalis is the most prevalent non-viral sexually transmitted infection [12]. The detection of T. vaginalis in cervical smears is not the best method. A study showed that both, microbiological culture and microscopic wet preparation for the identification of T. vaginalis is more sensitive than Pap method [13]. However, microbiological culture for detecting T. vaginalis is time consuming and costly.
In this study, infection with HSV is rare as seen in only 0.1%, however, the RR is 7.2, which indicates a high risk of developing a cervical lesion. Similar findings were also reported [14][15]. Changes of HSV in cervical smears include multinucleated epithelial cells with ground glass nuclei appearance, margination of the chromatin, and eosinophilic intranuclear inclusions [16].
HPV infection was seen in 1.7% in all cervical smears and the RR of cervical lesion with HPV infection is 16.59, indicating that patients are 16 times more susceptible to cervical cancer than non-infected patients. As mentioned earlier, HPV infection is highly associated with cervical cancer [2][3]. HPV DNA testing is more sensitive by detecting more true-positive precancers than cervical smears [17] [18]. Cytologic characteristics of HPV infection include koilocytosis and neoplasia. Koilocytic cells have a characteristic appearance marked by a dark nucleus encircled by a clear, cytoplasmic ring. The nuclei are usually enlarged and have an irregular border [19].
The findings of this study showed that abnormal cases of cervical smears were 6.9%. This finding is in line with the overall rate of abnormal cervical smears in developing countries where ranges between 1.5% and 6% were reported [20]. However, This finding is slightly higher than those studies in Saudi Arabia and Turkey where 1.7% and 3% were reported for abnormal cervical smears, respectively [21][22]. Also, our rates of mild dyskaryosis (1.8%), moderate dyskaryosis (0.7%), severe dyskaryosis (0.5%) and carcinoma (0.4%) are close to the findings of another neighbouring country performed in Saudi Arabia, where rates of 0.28%, 0.2%, 0.12% and 0.09% were reported, respectively [21]. A total of 688 (9.3%) out of 7112 cases were reported as unsatisfactory for cytological diagnosis. This could be due to sampling errors, insufficient number of cells, air drying artefacts or obscuring blood and inflammatory cells [23]. We also noticed that the number of unsatisfactory samples were reduced as we proceed to the subsequent years. This improvement could be referred to the increased experience of sampling and proper fixation and staining. It is worth to note that conventional cervical smears were used throughout this study.
Several limitations of our study are worth noting. First, differentiation of bacteria and fungi are not investigated with microbiological culture or other methods. Second, the absence of different types of HPV and HSV. Third, this study was based on data acquired from a single hospital, even though it serves as a tertiary referral hospital.
In conclusion, we found that bacteria and fungi are the most common microorganisms present in cervical smears but they are not associated with cervical abnormalities whereas HPV and HSV are less common but they are associated with cervical abnormalities.
Acknowledgements
We would like to thank all staff in Pathology Department at Sultan Qaboos University Hospital, Muscat, Sultanate of Oman, for their cooperation and help in providing the data.
References
- Global cancer statistics Jemal Ahmedin, Bray Freddie, Center Melissa M., Ferlay Jacques, Ward Elizabeth, Forman David. CA: A Cancer Journal for Clinicians.2011;61(2). CrossRef
- Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: A meta-analysis update Smith Jennifer S., Lindsay Lisa, Hoots Brooke, Keys Jessica, Franceschi Silvia, Winer Rachel, Clifford Gary M.. International Journal of Cancer.2007;121(3). CrossRef
- Epidemiologic studies of a necessary causal risk factor: human papillomavirus infection and cervical neoplasia Schiffman MH, Castle P. Journal of the National Cancer Institute.2003;95(6):E2.
- Human papillomavirus infection: biology, epidemiology, and prevention SCHEURER M.E., TORTOLERO-LUNA G., ADLER-STORTHZ K.. International Journal of Gynecological Cancer.2005;15(5). CrossRef
- Determination of cervicovaginal microorganisms in women with abnormal cervical cytology: the role of Ureaplasma urealyticum Lukic A, Canzio C, Patella A, Giovagnoli M, Cipriani P, Frega A, Moscarini M. Anticancer Research.2006;26(6c):4843-9.
- Sensitivity of a Papanicolaou smear in the diagnosis of candida albicans infection of the cervix Og A, Oe o, To A. North American Journal of Medicine and Science.2010;2(2):97-9.
- Evaluation of cervical smears at King Hussein Medical Centre, Jordan, over three and a half years Malkawi SR, Abu Hazeem RM, Hajjat BM, Hajjiri FK. Evaluation of cervical smears at King Hussein Medical Centre, Jordan, over three and a half years.2004;10(4-5):676-9.
- The incidence of Candida albicans in the last day of pregnancy and the first days of the new born Alteras I, Aryeli J. Mycopathologia.1980;72(2):85-7.
- Visualization of vaginal flora in cervical smears using a modified microwave silver-staining method Boon ME, Marres EM, Hoogeveen MM, Goedbloed AF, Milios J. Visualization of vaginal flora in cervical smears using a modified microwave silver-staining method.1998;30(2):75-80.
- Trichomonas vaginalis and cervical cancer Zhang Z, Graham S, Yu S, Marshall J, Zielezny M, Chen Y. Annals of Epidemiology.1995;5(4):325-32.
- Is Trichomonas vaginalis a cause of cervical intraepithelial neoplasia? Results from a combined analysis of 24 studies Zhang Z, Begg C. International Journal of Epidemiology.1994;23(4):682-90.
- Trichomoniasis: under control or undercontrolled? Soper David. American Journal of Obstetrics and Gynecology.2004;190(1). CrossRef
- Diagnosis of trichomoniasis in Pap smears; how effective is it Avwioro OG. European Journal of Experimental Biology.2011;1(1):10-3.
- Genital herpes simplex virus infection in females in Ibadan Nigeria Oni AA1, Adu FD, Ekweozor CC, Bakare RA. West African Journal of Medicine.1996;15(2):107-10.
- Whole slide imaging of Pap cell block preparations versus liquid-based thin-layer cervical cytology: a comparative study evaluating the detection of organisms and nonneoplastic findings Tawfik O, Davis M, Dillon S, Tawfik L, Diaz FJ, Fan F. Acta cytologica.2014;58(4):388-97.
- Performance of herpes simplex challenges in proficiency testing: observations from the College of American Pathologists (CAP) Proficiency testing (PT) Program Moriarty AT, Darragh TM, Souers R, Fatheree LA, Wilbur DC. Archives of Pathology & Laboratory Medicine.2009;133(9):1379-82.
- High-risk HPV testing on self-sampled versus clinician-collected specimens: A review on the clinical accuracy and impact on population attendance in cervical cancer screening Snijders PJF, Verhoef VMJ, Arbyn M, Ogilvie G, Minozzi S, Banzi R. International Journal of Cancer.2013;132(10):2223-36.
- Are self-collected samples comparable to physician-collected cervical specimens for human papillomavirus DNA testing? A systematic review and meta-analysis Petignat Patrick, Faltin Daniel L., Bruchim Ilan, Tramèr Martin R., Franco Eduardo L., Coutlée François. Gynecologic Oncology.2007;105(2). CrossRef
- Diagnosis of human papillomavirus genital tract infection Trofatter KF. The American Journal of Medicine.1997;102(5):21-7.
- Longitudinal trends in cervical cytological lesions and the effect of risk factors. A 30-year overview Sigurdsson K, Sigvaldason H. Acta Obstetricia et Gynecologica Scandinavica.2006;85(3):350-8.
- Profile of Pap smear cytology in the Western region of Saudi Arabia Jamal A, Al-Maghrabi JA. Saudi Medical Journal.2003;24(11):1225-9.
- Comparison of cervical cytological screening results between postmenopausal and elderly women Çakmak B, Köseoğlu DR. Türk Patoloji Dergisi. .2014;30(1):38-42.
- Cytohistological correlation and discrepancy of conventional Papanicolaou smear test with corresponding histopathology: A retrospective study over a 5-year period Alwahaibi NY, Al Sulimi SK, Bai UR. Eastern Mediterranean Health Journal.2015;21(8):579-83.
License
Copyright
© ,
Author Details