Cervical Cancer Screening in Pregnancy and Postpartum: A North Indian Hospital Based Prospective Observational Study
Download
Abstract
Introduction: In India, cervical cancer stands as the 2nd most common female cancer and it is the 2nd most leading cause of deaths in women aged 15 to 44 years. The first visit to the gynecologist for most of the women in India is during pregnancy, thereby making it a fair opportunity for the screening of premalignant and malignant cervical disease.
Methods: A prospective observational study was conducted in the Department of Obstetrics and Gynaecology, AIIMS, Rishikesh, Uttarakhand, India from January 2018 to January 2019. The Pap smear testing of 237 spontaneously conceived antenatal women, aging between 20 to 35 years was performed. The same women were followed up for postnatal testing after 6 weeks of delivery.
Results: Out of 237, 8 women were reported positive for pre malignant lesions of cervix in the antenatal testing, 5 cases of ASCUS, 1 case of AGC, 1 case of ASC-H & 1 case of HSIL. In the postnatal Pap smear testing, 37 women were lost to follow-up including 1 case of ASCUS. Postnatal Pap smear testing of the remaining 200 women showed that 193 women who were reported NILM in the antenatal period remained unchanged in the postnatal screening too. Out of the 7 women who tested positive, 4 cases of ASCUS, 1 case of AGC and 1 case of ASC-H showed regression, giving result as NILM in the postnatal screening test. Out of the 7 positive antenatal tests, 1 case which was reported as HSIL in the antenatal screening, remained unchanged in the postnatal period.
Conclusion: The study concluded that there is significant regression (p<0.01) of Positive Pap smear findings from antenatal to postnatal period. Hence, it is imperative to repeat Pap smear test in postnatal period.
Introduction
Cervical cancer is the 3rd most common cancer among women worldwide with an estimated 569,847 new cases and 311,365 deaths in the year 2018. In India, about 96,922 new cervical cancer cases were diagnosed and about 60,078 deaths occurred due to cervical cancer in the same year. Crude incidence rate of cervical cancer in the world is 15.1 per 100,000 per year and is 14.9 per 100,000 per year in India. It is the 2nd most common malignancy in Indian females (commonest being Carcinoma Breast) and the 2nd leading cause of death in women aged between 15 to 44 years. The cumulative risks of developing cervical cancer by age 75 years is 1% and of cervical cancer mortality is 0.8% worldwide. In India, it is 2% and 1% respectively [1]. Global incidence and mortality rate of cervical cancer depend upon the presence and effectiveness of screening programs for pre-invasive and invasive lesions of the cervix and human papilloma virus (HPV) vaccination. Due to these interventions, there has been a 75% decrease in the incidence and mortality of cervical cancer over the past 50 years in developed countries [2-4].
Awareness and health check-up practices have been shown to be poor in many developing countries, necessitating the need for structured awareness and vaccination campaigns. According to the world health survey 2003, in India the percentage of women screened for cervical cancer between age 25-64 years is only 3.1%. The first visit to the hospital for majority of the women in India is during pregnancy, hence, pregnancy makes a good opportunity for the screening of premalignant and malignant cervical disease. Cervical cancer has an estimated incidence of 0.8 to 1.5 cases per 10,000 births [5-7]. 1 to 3 percent women diagnosed with cervical cancer are pregnant or postpartum at the time of diagnosis [8-9]. About half of these cases are diagnosed antenatally, and the other half around 12 months postpartum [5]. The incidence of abnormal cervical cytologic findings during pregnancy is 0.72 to 1.67% [10]. Most patients are diagnosed at an early stage of disease probably as the result of routine antenatal screening, but it may also be a possibility that advanced-stage disease interferes with conception [11].
Cervical screening in pregnancy also poses a lot of problems because of hormone-induced changes in the cervix. Abnormal findings during pregnancy are generally more difficult to evaluate due to the normal pregnancy-related metaplastic changes.. Hence, repeat Pap smear screening in postnatal period is imperative as the persistent of high-grade lesions are common [12-15]. Abundant literature is available regarding the prevalence of premalignant lesions during pregnancy but there are very few prospective studies aiming to study the regression, persistence and progression of premalignant lesions of cervix from pregnancy to postpartum. Hence, the present study was designed with this background aiming at cervical cancer screening in the Antenatal women using Pap smear and comparing the pap smear results in pregnancy and Postpartum. Also the study attempted to establish a correlation between abnormal cervical cytology (i.e. high probability of HPV infection and abnormal vaginal microflora), and intrauterine fetal growth restriction.
Materials and Methods
A Prospective observational study was done in Department of Obstetrics & Gynecology, All India Institute of Medical Sciences, Rishikesh from January 2018 to January 2019. Women were recruited for initial 10 months of the study period and were followed up 6 weeks postpartum. The study was started after clearance from the institutional review board and ethics committee. 237 spontaneously conceived antenatal women presenting to the antenatal OPD with BMI 18-24.9 kg/m2 who consented for the study were included. Antenatal women with age less than 20 years or more than 35 years, history of medical disorders like hypertension, diabetes mellitus with vasculopathy, renal disease, anti-phospholipid antibody syndrome & chronic anemia and maternal or paternal history of small for gestational age were excluded from the study.
Informed and written consent was taken from the couple after explaining the detailed plan, purpose and duration of the study in their own language. Pap smear was performed similarly as for non-pregnant patients.
The patient was laid in the lithotomy position. Using Cusco’s speculum cervix was visualised and scraping from squamo-columnar junction was taken using cytobrush for endocervix and Ayres spatula for ectocervix with a 360-degree swipe. Scraping was spread evenly over the glass slide and immediately fixed with 95% alcohol for 30 minutes and stained with Papanicolaou stain and reviewed by pathologist. The women were counseled regarding slight vaginal bleeding after procedure and reassured. Results were expressed according to Bethesda system 2001 as-Negative for intraepithelial lesion (NILM), Atypical squamous cell of undetermined significance (ASCUS), Atypical squamous cell- can’t exclude high grade (ASC-H), low grade squamous intraepithelial lesion (LSIL), high grade squamous intraepithelial lesion(HSIL), squamous cell carcinoma, atypical glandular cells not otherwise specified (ASC-NOS), atypical glandular cells, suspicious for AIS or cancer (AGC-neoplastic), adenocarcinoma in situ. Women with abnormal cervical findings were managed according to ASCCP guidelines.
These women were followed till delivery and fetal birth weight was classified into percentile (intergrowth-211st standard growth chart) according to the sex and gestational age of the baby. Using these sex and gestational age-adjusted percentile, we classified FGR (Fetal growth restriction) babies as SGA - small for gestational age (those with sex-specific birth weights under the 10th percentile) or AGA - average for gestational age (those with sex-specific birth weights b/w 10th to 90th percentile). Follow up was done after 6 weeks of delivery and Pap smear was repeated.
All statistical analysis was carried out using SPSS 22.0 version. The quantitative data is represented as mean ±SD and the qualitative data is represented in frequency. The categorical data was analyzed using Chi Square Test, wherever necessary. P<0.05 was considered as significant.
Results
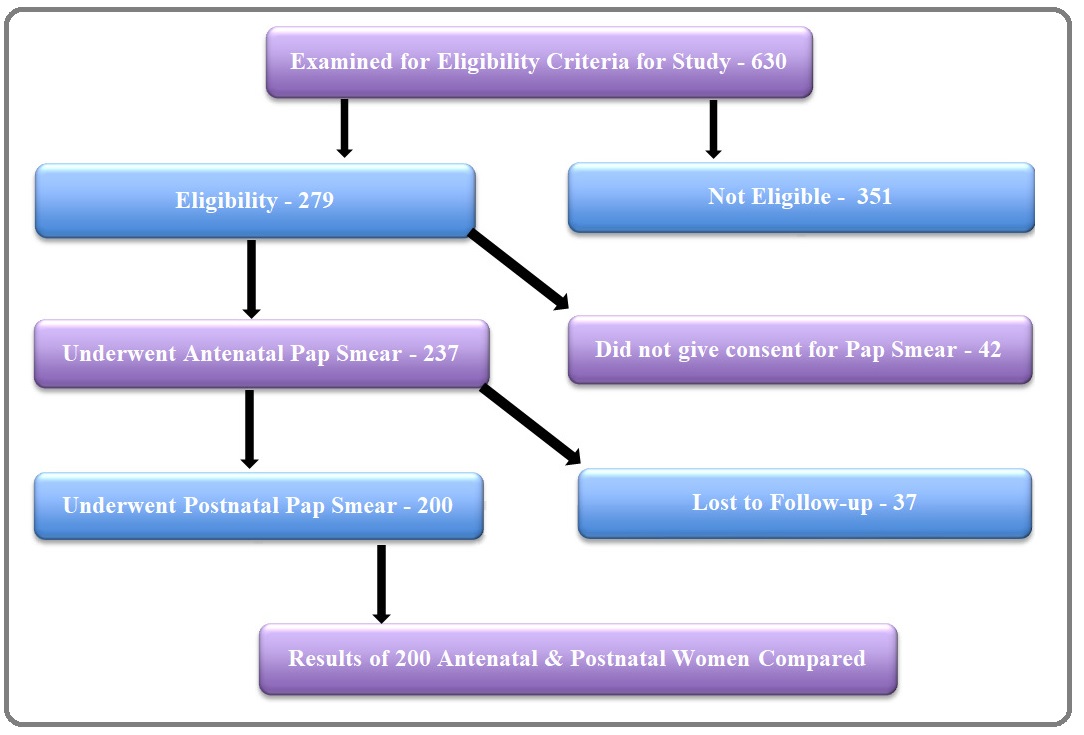
In the present study, 630 women were examined for eligibility out of whom 237 women fulfilled the eligibility criteria and underwent pap smear screening. These women had spontaneously conceived, ageing between 20 to 35 years with mean age 26.6±3.8 years (Figure 1).
Figure 1: Number of Patients at Different Stages of the Study.
These subjects had no risk factors for small for gestational age. Out of these 237 antenatal women, 102 (43%) women were between the age group of 20 to 25 years, 94 (39%) women were in the age group of 26 to 30 years and the remaining 41 (18%) women were in the age group of 31 to 35 years. Among these 237 antenatal women, 139 women (58%) were multipara and 98 women (42%) were primipara. In the present study, the Pap smear screening tests of these antenatal women were performed between 4 to 36 weeks period of gestation. Out of these 237 antenatal women, 71 women (30%) were tested before 14 weeks period of gestation, 128 women (54%) were tested between 14 to 28 weeks period of gestation & 38 women (16%) were tested after 28 weeks period of gestation. Out 237, 26 women have had primary education, 44 had secondary education, 39 had high school education, 89 had intermediate education and 39 were graduates. In terms of socio-economic status out of 237, 93 belonged to lower class, 125 belonged to lower middle class and 19 belonged to upper middle class (Table 1).
| Basis | Group | No. of Cases | Percentage (%) |
| Age (Years) | 20-25 | 102 | 43 |
| 26-30 | 94 | 39 | |
| 31-35 | 41 | 18 | |
| Parity | Multipara | 139 | 58 |
| Primipara | 98 | 42 | |
| POG (Weeks) | <14 | 71 | 30 |
| 14 to 28 | 128 | 54 | |
| >28 | 38 | 16 | |
| Education Level | Primary | 26 | 11 |
| Secondary | 44 | 18.50 | |
| High School (Matric) | 39 | 16.50 | |
| Intermediate (+2) | 89 | 37.50 | |
| Graduate | 39 | 16.50 | |
| Socio-economic Status | Lower | 93 | 39 |
| Lower Middle | 125 | 53 | |
| Upper Middle | 19 | 8 |
On per-speculum examination participating antenatal women it was observed that, out of these 237 antenatal women, 217 women (91.5%) had a healthy cervix & vagina. In the remaining 20 women (8.5%), 3 women had thick mucoid discharge, 7 women had thick curdy candidial discharge and 10 women had circumoral erosion. Out of the 10 women with circumoral erosion, 6 had only circumoral erosion present on cervix, 2 had hypertrophied cervix, 1 had nabothian cyst present and 1 was observed with bleeding on touch (Table 2).
| Per-speculum Finding | No. of Case (s) | Percentage (%) |
| Circumoral Erosion Present & Bleeding On Touch | 1 | 0.55 |
| Circumoral Erosion & Nabothian Cyst Present | 1 | 0.55 |
| Circumoral Erosion Present & Cx Hypertrophied | 2 | 0.80 |
| Thick Mucoid Discharge Present | 3 | 1.20 |
| Circumoral Erosion Present | 6 | 2.50 |
| Thick Curdy Discharge Present | 7 | 2.90 |
| Cx & Vagina Healthy | 217 | 91.50 |
| Total | 237 | 100 |
Out of the 237 antenatal women, the Pap smear results of 229 women (96.6%) were reported Negative for Intraepithelial Lesions or Malignancy (NILM). A total of 8 women (3.4%) were found positive for pre-malignant lesions of the cervix in the antenatal Pap smear results. 61 (25.7%) out of 237 antenatal women were reported with other associated findings such as – Candida Infection, Bacterial Vaginosis, and Inflammatory changes (Table 3).
| Basis | Findings | No. of Case (s) | Percentage (%) |
| Antenatal Pap Finding | ASC-H | 1 | 0.40 |
| ASCUS | 5 | 2.20 | |
| AGC | 1 | 0.40 | |
| HSIL | 1 | 0.40 | |
| NILM | 229 | 96.60 | |
| Total | 237 | 100 | |
| Other Associated Antenatal Pap Findings | Candida | 9 | 3.80 |
| Bacterial Vaginosis | 10 | 4.20 | |
| Inflammation | 42 | 17.70 | |
| Total Other Findings | 61 | 25.70 |
After 6 weeks of delivery, out of the 237, 200 women returned for the postnatal Pap smear screening test. 37 women were lost to follow-up in the postnatal Pap smear screening test. These 37 lost to follow-up cases included 1 case of ASCUS while the remaining 36 had no abnormal findings in the antenatal smear. Out of the 200 women who returned for follow up, 199 women were reported Negative for Intraepithelial Lesions or Malignancy (NILM) in the postnatal Pap smear testing and one women showed HSIL. Out of the 7 women who antenatally tested positive for premalignant lesions of the cervix, 4 cases of ASCUS, 1 case of AGC and 1 case of ASCH showed regression, testing as NILM in the postnatal Pap smear screening test. 1 case reported as HSIL antenatally, remained unchanged in the postnatal Pap smear screening test. Regression of abnormal cervical cytology from antenatal to postnatal period is significant with P-value <0.01 (Table 5). In addition to the above, a total of 35 (17.5%) out of 200 postnatal women had other associated Pap smear findings (BV, Inflammation). Out of these 35, 29 women (14.5%) were reported with Inflammatory Changes and 6 women (3%) were reported Bacterial Vaginosis (Table 4) (Table 5).
| Basis | Findings | No. of Case (s) | Percentage (%) |
| Postnatal Pap Finding | ASC-H | 0 | 0.00 |
| ASCUS | 0 | 0.00 | |
| AGC | 0 | 0.00 | |
| HSIL | 1 | 0.50 | |
| NILM | 199 | 99.50 | |
| Total | 200 | 100 | |
| Other Associated Postnatal Pap Findings | Candida | 0 | 0.00 |
| Bacterial Vaginosis | 6 | 3.00 | |
| Inflammation | 29 | 14.50 | |
| Total Other Findings | 35 | 17.50 |
| Cross Tabulation | Progression | Regression | Unchanged | Total | P-value | |
| Antenatal Pap Smear Findings | NILM | 0 | 0 | 193 | 193 | |
| ASCUS | 0 | 4 | 0 | 4 | ||
| ASC-H | 0 | 1 | 0 | 1 | ||
| HSIL | 0 | 0 | 1 | 1 | ||
| AGC | 0 | 1 | 0 | 1 | ||
| Total | 0 | 6 | 194 | 200 | <0.01 |
Women who were tested positive for the other associated Pap smear findings (Inflammation, BV & Candida) were followed for repeat postnatal Pap smear screening test and the following observations were made.
No new associated other findings were recorded in the postnatal Pap smear result that previously recorded NILM in the antenatal Pap smear result. However, Inflammatory Changes were recorded in 2 (1%) cases that were found positive for ASCUS in the antenatal Pap screening test (Table 6).
| Other Associated Pap Findings | Antenatal | Postnatal | ||
| Persisted | Regressed | New | ||
| Candida | 9 (4.5%) | 0 | 9 (4.5%) | 0 |
| Bacterial Vaginosis | 10 (5%) | 6 (3%) | 4 (2%) | 0 |
| Inflammation | 42 (21%) | 29 (14.5%) | 13 (6.5%) | 2 (1%) |
| Total | 61 (30.5%) | 35 (17.5%) | 26 (13%) | 2 (1%) |
We also determined the correlation of abnormal cervical cytology and bacterial vaginosis with intrauterine fetal growth restriction. While establishing this correlation it was observed that, out of the 7 neonates of women with abnormal cervical cytology, 5 were average for gestational age (AGA) and 2 were small for gestational age (SGA). Correlation is not significant as p-value (0.532) is >0.05 (Table 7 (A)&(B)).
| Cross Tabulation | ASC-H | ASCUS | AGC | HSIL | NILM | Total | |
| Wt. for GA | AGA | 1 | 3 | 0 | 1 | 131 | 136 |
| SGA | 0 | 1 | 1 | 0 | 62 | 64 | |
| TOTAL | 1 | 4 | 1 | 1 | 193 | 200 | |
| Table 7 (B) - Chi-Square Tests | |||||||
| Chi- Square Tests | Value | Df | Asymptotic Significance | ||||
| (2-sided) | |||||||
| Pearson Chi Square | 3.158a | 4 | 0.532 | ||||
| Likelihood Ratio | 3.917 | 4 | 0.417 | ||||
| N of Valid Cases | 200 |
*a. 8 cells (80.0%) have expected count less than 5. The minimum expected count is. 32
While establishing the correlation between bacterial vaginosis and intrauterine fetal growth restriction it was observed that, out of the 10 neonates of women with bacterial vaginosis, 4 were average for gestational age (AGA) and 6 were small for gestational age (SGA). This correlation was not significant (p-value-0.149) Table 8 (A)&(B).
| Cross Tabulation | Wt. For Gestational Age | Total | |||
| AGA | NA | SGA | |||
| Antenatal Bacterial Vaginosis | NO | 131 | 1 | 58 | 190 |
| YES | 4 | 0 | 6 | 10 | |
| Total | 135 | 1 | 64 | 200 | |
| Table 8 (B) - Chi-Square Tests | |||||
| Chi-Square Tests | Value | Df | Asymptotic Significance (2-sided) | ||
| Pearson Chi-Square | 3.811a | 2 | 0.149 | ||
| Likelihood Ratio | 3.549 | 2 | 0.17 | ||
| N of Valid Cases | 200 |
Discussion
The importance to increase awareness about the Pap smear screening test in India cannot be overemphasized. In the present study we utilized antenatal visits as an important opportunity for cervical cancer screening. We observed that there was only 1 case of pregnancy loss, which had ASC-H in the antenatal Pap smear test. favouring that the high-grade lesion might interfere with pregnancy. Apart from this, the procedure was reasonably safe.
In the present study out of the 237 antenatal women, the Pap smear results of 229 women (96.6%) were reported Negative for Intraepithelial Lesions or Malignancy (NILM). A total of 8 women (3.4%) were found positive for abnormal cervical cytology. In our study prevalence of abnormal cervical cytology in antenatal women was 2.2% for ASCUS, 0.4% for ASC-H, 0.4% for HSIL and 0.4% for AGC, with a total of 3.4% for abnormal cervical cytology.
In comparison to various studies conducted in different parts of the India and the world, authors found that the prevalence of abnormal cervical cytology was higher in the present study population from the State of Uttarakhand (India) as compared to other states of India but was lower in comparison to other countries (Table 9).
| S.No | Study | ASCUS | ASC-H | LSIL | HSIL | AGC | Total |
| 1 | Priya SS et al. [16] (Tamil Nadu, India) | 0.5 | - | 0.5 | - | - | 1 |
| 2 | Radha Bhai Prabhu et al. [23] (Tamil Nadu, India) | 0.3 | - | 0.3 | 0.3 | - | 1 |
| 3 | Bakari et al. [24] (Nigeria) | - | - | 5 | 1 | - | 6 |
| 4 | Ma L et al. [25] (China) | 5.6 | - | 2.97 | 0.64 | 0.14 | 9.4 |
| 5 | Khaengkhor p et al. [26] (Thailand) | 2.8 | - | 3.5 | 0.7 | - | 7 |
| 6 | Dinc et al. [27] (Turkey) | 0.9 | - | - | - | - | 0.9 |
| 7 | (Present study) Gill et al.(Uttarakhand) | 2.2 | 0.4 | - | 0.4 | 0.4 | 3.4 |
In addition to prevalence, we also attempted to highlight the importance of doing Pap smear in the postnatal period. Postpartum visit for cervical cancer has been traditionally done at 6 to 8 weeks postpartum. However studies have shown comparable results when the screening test is done 2 to 3 weeks postpartum as compared to 6 to 8 weeks [30]. In the present study, the follow up visit was scheduled at 6 weeks postpartum following the institutional protocol and it was convenient for postpartum women to get the screening at an already scheduled visit to the hospital. Upon postpartum testing, it was found that screening results during pregnancy could be false positive. Hence it is imperative to repeat the Pap smear test in the postnatal period before initiating treatment.
We found few studies been conducted in different parts of the world to observe the pattern of change in abnormal cervical cytology from the antenatal to the postnatal period. As per our knowledge, no such study as of now has been conducted in India. In the present study we observed that out of the 200 women, 199 were reported Negative for Intraepithelial Lesions or Malignancy (NILM) in the postpartum period showing significant regression with p-value <0.01.Out of 7 women who tested positive in the antenatal period, 6 women had NILM and 1 woman was reported positive for High-grade Squamous Intraepithelial Lesion (HSIL) in the postpartum period as well who had the same finding (previously HSIL) in the antenatal Pap smear screening test, showing persistence.
The observed regression rate in the present study was 85.7% (57.1% for low-grade lesion (ASCUS), 28.5% for high-grade lesions (ASC-H and AGC) and the observed persistence rate was 14.2%. Various other studies were also performed in different parts of the world to study the postpartum regression rate of Low and High grade lesions of the cervix (Table 10).
| S.No | Study | Low grade(ASCUS &LSIL) | High grade (HSIL, ASC-H and AGC) |
| 1 | Suzuki et al. [29] (Japan) | 61 | 25 |
| 2 | Bakari et al. [24] (Nigeria) | 15 | 0 |
| 3 | Ma L et al. [25] (China) | 72.3 | 17 |
| 4 | Siristatidis Ch et al. [28] (Greece) | - | 45 |
| 5 | Kaplan KJ et al. [13] (US) | 62 | 0 |
| 6 | Fader AN et al. [14] (US) | - | 53 |
| 7 | Gill et al. Present study | 57.1 | 28.5 |
Apart from premalignant lesions, this study showed 42 women (21%) with benign inflammatory Changes. Out of 7 women with abnormal cervical cytology, 2 had the development of inflammatory changes in the postnatal period despite the regression of abnormal cytology.
Similar to the present study, Priya SS et al. reported inflammatory changes in 26% of the subjects [16]. Atilgan R et al. and Kulkarni PR reported 95% and 74.5% benign inflammatory changes respectively which was much higher than the present study [17-18].
Bhutia K et al. and Barouti E et al. reported that women with persistent inflammation should be appropriately treated; else the chances of development of cervical intraepithelial lesions increases. Due to the low sensitivity of Pap smear, premalignant lesions of the cervix can be missed in women with inflammatory Pap smears [19-20]. We also attempted to determine the association of abnormal cervical cytology and bacterial vaginosis (BV) with intrauterine fetal growth restriction, and found no significant association. Thorsen et al. found that in nulliparous women, BV was associated with SGA (adj. OR 1.6 (0.7–3.1)) compared to nulliparous women without BV. No such associations were seen for multiparous women with BV.
They concluded that BV was not associated with spontaneous preterm birth, but was associated with both LBW and SGA in nulliparous women [21]. Similarly Svare et al. in Denmark, they found that birth weight was significantly lower in infants of women with BV than in infants of women without BV (3408 versus 3511 g, P < 0.01) [22].
Small sample size and based on a single centre form the major limitations of this study. Also the cervical screening was performed by conventional pap smear and HPV DNA testing was not performed simultaneously.
To conclude, the present study demonstrated significant regression of pre malignant lesion of cervix from antenatal to postnatal period emphasizing the importance of postpartum testing. Efforts should be made to educate and counsel women about the importance of cervical cancer screening test in developing countries like India. Larger, multicentric studies are needed to assess the postpartum regression, persistence or progression of premalignant lesions of cervix.
Acknowledgements
We like to extend our sincere gratitude to the Department of Pathology for their contribution in this study.
Funding Information
The contributors of this study utilized no sources of funding.
References
- ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre) Bruni L, Albero G, Serrano B, Mena M, Gómez D, Muñoz J, et al . Human Papilloma-virus and Related Diseases in India.Summary Report 17 June 2019.
- Cervical cancer prevention in the era of prophylactic vaccines: A preview for gynecologic oncologists Collins Yvonne, Einstein Mark H., Gostout Bobbie S., Herzog Thomas J., Massad L. Stuart, Rader Janet S., Wright Jason. Gynecologic Oncology.2006;102(3). CrossRef
- Effect of screening on incidence of and mortality from cancer of cervix in England: evaluation based on routinely collected statistics Quinn M., Babb P., Jones J., Allen E.. BMJ.1999;318(7188). CrossRef
- A descriptive study of the decline in cervical screening coverage rates in the North East and Yorkshire and the Humber Regions of the UK from 1995 to 2005 Willoughby Bruce J., Faulkner K., Stamp E. C., Whitaker C. J.. Journal of Public Health.2006;28(4). CrossRef
- Obstetrical deliveries associated with maternal malignancy in California, 1992 through 1997 Smith Lloyd H., Dalrymple John L., Leiserowitz Gary S., Danielsen Beate, Gilbert William M.. American Journal of Obstetrics and Gynecology.2001;184(7). CrossRef
- Outcome of pregnancies after cold knife conization of the uterine cervix during pregnancy Demeter A, Sziller I, Csapo Z, Szantho A, Papp Z. Eur J Gynaecol Oncol.2002;23(3):207-210.
- Cervical cancer in pregnancy: reporting on planned delay in therapy Duggan B, Muderspach LI, Roman LD, Curtin JP, d’Ablaing G 3rd , Morrow CP. Obstet Gynecol.1993;82:598-602.
- Management of Stage I Cervical Cancer in Pregnancy Nguyen C., Montz F. J., Bristow R. E.. Obstetrical & Gynecological Survey.2000;55(10). CrossRef
- Cancer and Pregnancy CREASMAN WILLIAM T.. Annals of the New York Academy of Sciences.2001;943(1). CrossRef
- Screening for cervical neoplasia during pregnancy Cronjé H.S., van Rensburg E., Niemand I., Cooreman B.F., Beyer E., Divall P.. International Journal of Gynecology & Obstetrics.1999;68(1). CrossRef
- Cervical neoplasia during pregnancy: Diagnosis, management and prognosis Van Calsteren K., Vergote I., Amant F.. Best Practice & Research Clinical Obstetrics & Gynaecology.2005;19(4). CrossRef
- Special situation: abnormal cervical cytology during pregnancy Brown D, Barren P, Kaplan KJ, Winter WE 3rd , Zahn CM. Clin Obstet Gynecol.2005;48(1):178-85.
- Cervical dysplasia in pregnancy: a multi-institutional evaluation Fader Amanda N., Alward Erin K., Niederhauser Amy, Chirico Christina, Lesnock Jamie L., Zwiesler Daniel J., Guido Richard S., Lofgren Darla J., Gold Michael A., Moore Kathleen N.. American Journal of Obstetrics and Gynecology.2010;203(2). CrossRef
- Prognosis and recurrence risk for patients with cervical squamous intraepithelial lesions diagnosed during pregnancy Kaplan Keith J., Dainty Louis A., Dolinsky Brad, Rose G. Scott, Carlson Jay, McHale Michael, Elkas John C.. Cancer.2004;102(4). CrossRef
- Natural history of cervical intraepithelial neoplasia during pregnancy Serati Maurizio, Uccella Stefano, Laterza Rosa M., Salvatore Stefano, Beretta Paolo, Riva Cristina, Bolis Pier Francesco. Acta Obstetricia et Gynecologica Scandinavica.2008;87(12). CrossRef
- PAP smear in pregnancy: a hospital-based study Priya S. Senthil, Shankar R.. International Journal of Reproduction, Contraception, Obstetrics and Gynecology.2018;7(12). CrossRef
- Comparison of risk factors for invasive squamous cell carcinoma and adenocarcinoma of the cervix: Collaborative reanalysis of individual data on 8,097 women with squamous cell carcinoma and 1,374 women with adenocarcinoma from 12 epidemiological studies International Journal of Cancer.2006;120(4). CrossRef
- The Epidemiology of Cervical Cancer Franco Eduardo L., Schlecht Nicolas F., Saslow Debbie. The Cancer Journal.2003;9(5). CrossRef
- Persistent inflammation on Pap smear: Does it warrant evaluation? Gami N, Trivedi SS, Bhutia K, Puri M, Aggarwal K. Indian Journal of Cancer.2011;48(2). CrossRef
- The pathogenic microorganism in papanicolaou vaginal smears and correlation with inflammation Barouti E, Farzaneh F, Sene A. J Family Reprod Health.2013;7:23-27.
- Bacterial vaginosis in early pregnancy is associated with low birth weight and small for gestational age, but not with spontaneous preterm birth: A population-based study on Danish women Thorsen Poul, Vogel Ida, Olsen Jørn, Jeune Bernard, Westergaard Jes G., Jacobsson Bo, Møller Birger R.. The Journal of Maternal-Fetal & Neonatal Medicine.2006;19(1). CrossRef
- Bacterial vaginosis in a cohort of Danish pregnant women: prevalence and relationship with preterm delivery, low birthweight and perinatal infections Svare JA, Schmidt H, Hansen BB, Lose G. BJOG: An International Journal of Obstetrics & Gynaecology.2006;113(12). CrossRef
- Opportunistic cervical cancer screening in pregnancy Prabhu RB, Velayudham D, Netaji S, Singal H, Venkatachalam R. International journal of medical research and health sciences.2016;5(1):278-281.
- The prevalence and course of preinvasive cervical lesions during pregnancy in a Northern Nigerian Teaching Hospital Bakari Fadimatu, Abdul MuhammadA, Ahmed SaadA. Annals of African Medicine.2017;16(2). CrossRef
- Pregnancy-related cervical cytological changes and clinical management Ma L, Bian ML, Liu J, Wang XL, Pang CH, Chen Y, et al . Zhonghua Fu Chan Ke Za Zhi.2011 ;46(2):84-87.
- Prevalence of abnormal cervical cytology by liquid-based cytology in the antenatal care clinic, Thammasat University Hospital Khaengkhor p, Mairaing k, Suwannarurk k, Thaweekul y, Poomtavorn y, Pattaraarchachai j, Bhamarapravatana k. J Med Assoc Thai.2011;94(2):152-158.
- Pap Smear Screening Results for Turkish Pregnant Women Dinc Ayten. Asian Pacific Journal of Cancer Prevention.2012;13(11). CrossRef
- The role of the mode of delivery in the alteration of intrapartum pathological cervical cytologic findings during the postpartum period Siristatidis Ch, Vitoratos N, Michailidis E, Syciotis C, Panagiotopoulos N, Kassanos D, et al . Eur J Gynaecol Oncol.2002;23(4):358-360.
- Comparing Papanicolaou test results obtained during pregnancy and post-partum Suzuki Kazuhiro, Furuhashi Madoka, Kawamura Takuya, Kubo Michiko, Osato Kazuhiro, Yamawaki Takaharu. Journal of Obstetrics and Gynaecology Research.2017;43(4). CrossRef
- Postpartum Cervical Cancer Screening Adequacy and Results: Comparison of Results 2-3 Versus 6-8 Weeks Postpartum Carty, Jenava , Batig, Alison . Obstetrics & Gynecology .2017;129(5):57S.
License
Copyright
© ,
Author Details