A Case of Nodular Fasciitis of the Breast Previously Misdiagnosed as Breast Carcinoma; A Case Report
Download
Abstract
Introduction: Nodular fasciitis is an exceptional benign soft tissue tumor of the breast that clinically and radiologically can simulate invasive duct carcinoma.
Case presentation: We report a case of 67-year-old woman who had a palpable right breast mass of 2 months duration. Sonography showed a hypoechoic heterogeneous round nodule with irregular and speculated borders in right breast. Right breast mass core needle biopsy was inconclusive. Right mastectomy was done due to highly suspicious for malignancy on imaging. Pathological and immunohistochemical examination revealed that the tumor composed of a stellate spindle cell tumor with red blood cells extravasation, compatible with nodular fasciitis. Therefore, pathological evaluation of the lesion is crucial in the assembly of the diagnosis.
Conclusion: Nodular fasciitis should be considered in the differential diagnosis of any suspicious breast mass.
Introduction
Nodular fasciitis (NF) is a benign and reactive growth of the soft tissues related to fascia. The lesion is generally small and solitary; NF typically arises in the upper extremities of adults. NF usually occurs in patients who are between 20 and 35 years old, while it is uncommon in patients older than 60 years old [1]. NF of the breast is a benign pseudosarcomatous proliferative lesion that may develop, despite its extreme rarity. It is characterized by rapid appearance and growth. It can be mistaken for a breast carcinoma due to its vague clinical, radiological, and histological findings [2]. So, NF is a soft tissue lesion that in uncommon event occurs in the breast and can clinically and radiologically mimic malignant tumor. Awareness of such an entity in the breast obviates the need for preventable surgical intervention.
Case presentation
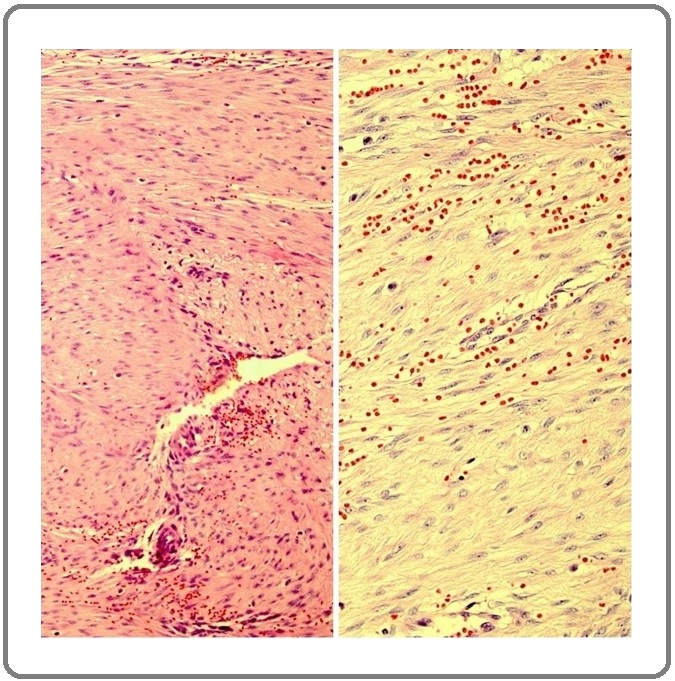
A 67-year-old female patient presented with a 2 months’ history of a right palpable breast mass. She was admitted to the department of surgery in Pars hospital in Tehran in Iran. The patient’s family history and past medical history were unremarkable. There was no history of trauma. General examination was negative and only right palpable breast mass at 10 o’ clock was found. No axillary lymph node swelling was found. Routine laboratory investigations were normal. The patient underwent sonography which showed a hypoechoic heterogeneous round nodule with irregular and speculated borders in right breast. So, imaging diagnosis of malignancy was virtually possible. Diagnosis required histopathologic examination in order to establish a diagnosis. We performed a core needle biopsy of breast, which was inconclusive. As the case was highly suspicious for malignancy, a right mastectomy with intra-operative frozen section study for right axillary lymph nodes were performed. Frozen section study showed one reactive sentinel lymph node. The pathologic report of breast mass revealed a neoplastic tissue composed of bundles and fascicles of bland-looking spindle cells. Extravasation of red blood cells and scattered lymphoid cells were also noted. No nuclear atypia, necrosis, or mitosis were seen (Figure 1).
Figure 1. Histopathologic Examination Revealed a Neoplastic Tissue Composed of Bundles and Fascicles of Bland-looking Spindle Cells. Extravasation of red blood cells are noted. No nuclear atypia, necrosis, and mitosis are seen (left: x100 and right: x400).
Based on the pathological findings, a phyllodes tumor and a spindle cell carcinoma, among other entities, were included in the differential diagnosis, but there was no definitive diagnosis. Immunohistochemical staining for smooth muscle actin (SMA) was positive and desmin was scattered positive. Cytokeratin (CK), P63, B-catenin, CD34, B-cell lymphoma 2 (BCL-2), and estrogen receptor (ER) were negative (Figure 2).
Figure 2. Immunohistochemical Examination Revealed A) Desmin (Scattered Positive), B) Smooth Muscle Actin (Positive), C) CD34 (Negative), D) B-catenin (Negative), E) P63 (Negative), F) Estrogen Receptor (Negative), and G) Cytokeratin (Negative).
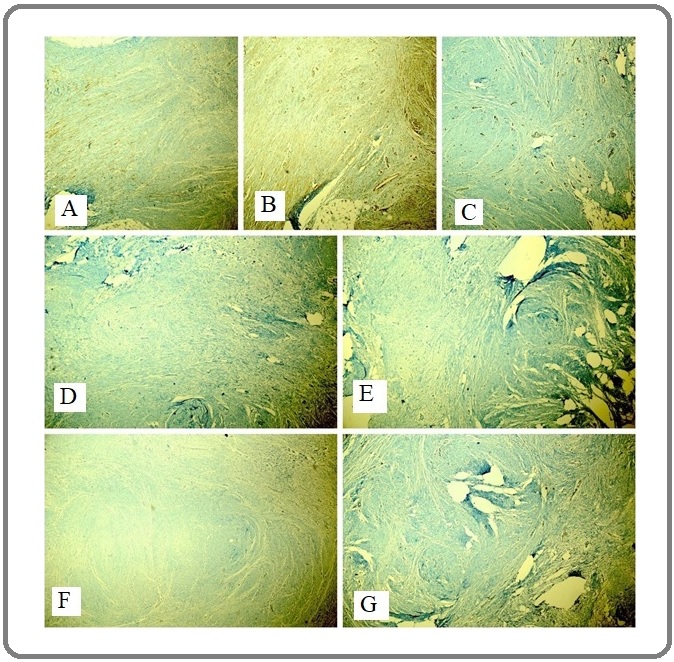
Proliferative index (Ki-67) was about 6-7%. The ultimate pathologic results ruled out the possibility of sarcoma and other spindle cell carcinoma, and confirmed that the breast mass was nodular fasciitis (NF). Based on the immunohistochemical findings, the patient received no adjuvant chemo-radio therapy.
Discussion
NF is a proliferative lesion of the reactive fibroblastic cells. Proliferation originates from the fascia of the subcutaneous tissue. This lesion can occur in every place in the body but it is rare in the breast [3]. NF, was first explained by Konwaler, et al. [4]. However, the etiology is still unclear. It is believed that local injury may stimulate the fibroblastic proliferation. Although, the history of trauma was recognized in about 10–15% of patients [5]. There was no history of trauma in our case. NF is described a reactive rather than a true neoplastic lesion. For the reason, its quick expansion, it is often misdiagnosed as a sarcoma. Also, it can clinically and radiologically mimic invasive cancer [6] which in our case, radiologic findings was highly suspicious for malignancy (invasive cancer). NF is able to be mistaken for malignant fibrous lesions such as fibrosarcoma or breast carcinoma when located in breast. This present a difficulty for appropriate treatment strategy as the natural history of nodular fasciitis is spontaneous regression [7]. The imaging manifestation of NF frequently exhibits the histological appearance. Thus, suspicious appearances have been described. This diversity in imaging appearance may expose that as the lesion becomes more mature it becomes more fibrotic [8]. NF is not regularly diagnosed by fine needle aspiration cytology or core needle biopsy, and it commonly needs excisional biopsy for histologic confirmation. As the articles that have reported the proliferation of neoplastic spindle cells were not conclusive, surgical excision and examination of the whole specimen are necessary to reach final diagnosis [9]. The diagnosis of bland looking spindle cell proliferations of the breast is often complicated because there are similar morphological and immunohistochemical overlap between the diverse entities [10]. Histologically, such proliferated spindle cells may show a specific level of mitosis and cellularity, which can enhance suspicion of malignancy, even though they are benign. Recent articles have described that the most general diagnostic difficulty arise with other benign and malignant spindle cell tumors (including spindle cell carcinomas and sarcomas) and fibromatosis [11]. In our case, NF was diagnosed based on the histomorphology and immunostaining consequences (positivity for SMA and desmin with negativity for CK, P63, BCL-2, and CD34). Some reports point out that the key structures for diagnosis are the existence of inflammatory cells (principally lymphocyte) and red blood cells extravasation with reactive fibroblasts clusters that are arranged in short bundles, as in our case [12]. The rarity and the unclear clinical and radiological findings of breast NF create the differential diagnosis and management challenging. Awareness of the clinical, pathological and prognostic aspects of this condition is necessary for breast specialists in order to get better their diagnostic and therapeutic interventions [13]. If the breast surgeon considers NF as a probability alongside with other differential diagnoses, close observation could be main management choice [14]. Most cases are diagnosed after subsequent surgical excision, the natural history is not well known. Also, local recurrence is infrequent and those managed conservatively regress spontaneously [15]. It is difficult to diagnose NF using imaging or preoperative biopsy. Therefore, to avoid overtreatment, it is mandatory to keep the possibility of nodular fasciitis in mind.
In conclusion, NF of the breast is an exceptional lesion that mimics breast cancer clinically and radiologically. Correct diagnosis needs histopathologic and immunohistochemical examinations. The pathologist should also be alert of the patient presentation in order not to misdiagnose this benign entity.
Acknowledgments
None.
Conflicts of interest
None declared.
Funding source
None.
References
- Nodular fasciitis of the breast and knee in the same patient Polat P, Kantarci M, Alper F, Gursan N, Suma S, Okur A. American Journal of Roentgenology.2002;178(6):1426-1428.
- Nodular Fasciitis of the Breast Previously Misdiagnosed as Breast Carcinoma Ozben Volkan, Aydogan Fatih, Karaca Fatih Can, Ilvan Sennur, Uras Cihan. Breast Care.2009;4(6). CrossRef
- Nodular fasciitis of the breast clinically resembling breast cancer in an elderly woman: a case report Hayashi Satoshi, Yasuda Shunsuke, Takahashi Nana, Okazaki Satoshi, Ishibashi Kei, Kitada Masahiro, Miyokawa Naoyuki. Journal of Medical Case Reports.2017;11(1). CrossRef
- Subcutaneous Pseudosarcomatous Fibromatosis (Fasciitis) Konwaler Benjamin E., Keasbey Louisa, Kaplan Leo. American Journal of Clinical Pathology.1955;25(3). CrossRef
- Nodular Fasciitis of the Breast Mimicking Breast Cancer Yamamoto Shinya, Chishima Takashi, Adachi Shouko. Case Reports in Surgery.2014;2014. CrossRef
- Involvement of 3q21 in Nodular Fasciitis Weibolt Vines M, Buresh Cary J, Roberts Cory A, Suijkerbuijk Ron F, Pickering Diane L, Neff James R, Bridge Julia A. Cancer Genetics and Cytogenetics.1998;106(2). CrossRef
- Nodular Fasciitis in the Axillary Tail of the Breast Chetlen Alison Lynn, Samardzic Dejan, Malysz Jozef. Journal of Radiology Case Reports.2014;8(5). CrossRef
- Unusual benign breast lesions Porter G.J.R., Evans A.J., Lee A.H.S., Hamilton L.J., James J.J.. Clinical Radiology.2006;61(7). CrossRef
- The Rare Benign Lesion That Mimics a Malignant Tumor in Breast Parenchyma: Nodular Fasciitis of the Breast Erinanc Hilal, Türk Emin. Case Reports in Pathology.2018;2018. CrossRef
- Practical approach to diagnosis of bland-looking spindle cell lesions of the breast Magro Gaetano. Pathologica.2019;111(04). CrossRef
- Enzinger and Weiss’s Soft tissue tumors 6-th edition. Philadelphia: Saunders/Elsevier; 2014 Goldblum J, Folpe A, Weiss SHW. .
- Nodular Fasciitis of the Breast: A Case Report Tulbah Asma, Baslaim Muna, Sorbris Ralph, Al-Malik Osama, Al-Dayel Fouad. The Breast Journal.2003;9(3). CrossRef
- Breast Nodular Fasciitis: A Comprehensive Review Paliogiannis Panagiotis, Cossu Antonio, Palmieri Giuseppe, Scognamillo Fabrizio, Pala Carlo, Nonnis Rita, Sotgiu Giovanni, Fois Alessandro, Palomba Grazia, Attene Federico. Breast Care.2016;11(4). CrossRef
- Fine needle aspiration cytology of nodular fasciitis of the breast Sakuma Takahiko, Matsuo Koji, Koike Shinya, Tagami Kouichiro. Diagnostic Cytopathology.2014;43(3). CrossRef
- A case of nodular fascitis of the breast and review of the literature Brown V., Carty N.J.. The Breast.2005;14(5). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2021
Author Details