Associations between Nonalcoholic Fatty Liver Disease and Histopathological Features of Patients with Adenocarcinoma of Colon in Dharmais National Cancer Hospital, National Cancer Center, Indonesia
Download
Abstract
Objective: Previous studies have suggested that non-alcoholic fatty liver disease (NAFLD) may be a risk factor for colon cancer and that there was a high prevalence of colon cancer patients with NAFLD. This study aimed to determine the prevalence of fatty liver in colon adenocarcinoma patients in Dharmais National Cancer Hospital, Indonesia, and its associations with grading and extend of invasion.
Methods: The retrospective cross-sectional study was conducted in Dharmais National Cancer Hospital, Indonesia. The diagnosis of adenocarcinoma of colon was confirmed by histopathology. The cases from 2018-2019 were studied. All variables taken from medical records were anthropometric measures, ALT, AST, grading, and extend of invasion of adenocarcinoma. The liver of the Patients’ was assessed with Hepatic Steatosis Index (HSI) scoring. The data was computed statistically with the chi-square test or Kolmogorov Smirnov test.
Result: 84 patients were included in the study. It was found that 14.3% of the patients have fatty liver. Bivariate analysis showed that HSI groups and well-differentiated and moderate-poor-differentiated adenocarcinoma have the p-value of 0,026. The p-value of HSI groups and extend of invasion of the adenocarcinoma was 1.
Conclusion: The prevalence of fatty liver in patients who had adenocarcinoma of colon was 14.3%. There was an association between fatty liver and grading. There was no association between fatty liver and the extend of invasion.
Introduction
Colon cancer is one of the most prevalent cancers worldwide. Colon cancer contributes to 6% of all cancer cases in 2020. A similar number is also seen in cases in Asia (6%). Indonesia has the highest mortality of colon cancer in Southeast Asia, with an estimation of 9444 deaths in 2020 [1].
Non-alcoholic fatty liver disease (NAFLD), also known simply as fatty liver is an accumulation of fat in the liver. The global prevalence of NAFLD increases in recent years. A study found that in Indonesia, 30% of its population has a fatty liver. Obesity is one of the risk factors of NAFLD. In fact, there is an association between NAFLD and overweight to severe obesity. The prevalence of obesity itself in Indonesia is rising rapidly since 1993, with a rate of 1.5 to 2 times faster than the global rate. This contributes to the prevalence of NAFLD as well [2-5].
According to recent studies, it was discovered that NAFLD might be a risk factor for colorectal cancer [3]. Mikolasevic et al. conducted a review of previous studies and found that there was a significant prevalence of NAFLD in colorectal benign and malignant tumors [6].
Lipid accumulation in the liver may cause inflammation. It is thought that the rise of inflammatory substances such as C-reactive protein (CRP), interleukin, and matrix metalloproteinase (MMP) plays a role in establishing a favorable environment for tumor growth in the colon and rectum. Moreover, the decrease of adiponectin in a fatty liver may trigger proliferation and create antiapoptosis effects [3].
There may be a relation between NAFLD and the differentiation of colon adenocarcinomas. One mechanism that may explain the relation is a liver fatty acid-binding protein (L-FABP) that upregulates in a fatty liver [7,8]. Apart from grading, colon cancer can be assessed through the extend of invasion. The increase of MMP in a fatty liver may further deepen the extend of invasion of a colon tumor [3,9].
The aim of this study was to determine the prevalence of fatty liver in colon adenocarcinoma patients in Dharmais National Cancer Hospital (DCNH), Indonesia, and its associations with grading and the extend of invasion. This study also gives a new perspective of the association between NAFLD and colorectal cancer.
Materials and Methods
The retrospective cross-sectional study was conducted in Dharmais National Cancer Hospital, Jakarta, Indonesia. Patients who had colon adenocarcinoma confirmed by histopathology from 2018-2019 were studied from medical records to obtain their anthropometric measures, ALT, AST, grading, and extend of invasion of the cases. Patients’ diabetic status and was also obtained. The anthropometric measures include body weight, height, and BMI. The BMI is defined as low BMI (under 25, i.e. normal BMI) and high BMI (more than 25, i.e. overweight and all obese grades). Patients with benign colon tumors such as adenomas and polyps were excluded. The excluded criteria of the study were patients with benign tumors colon such as adenomas and polyps. Patients with other liver diseases such as viral hepatitis, hepatocellular carcinoma, and secondary liver cancer as a result of metastasis from other organs including from the colon.
The diagnosis of adenocarcinoma, not-otherwise- specified (NOS), was confirmed by histopathology examination and the grading and the extend of invasion of the cases were determined. Grading was defined as the tumor’s differentiation and extend of invasion is defined as the tumor’s progression up to outside of the affected organ. The fatty liver was assessed with Hepatic Steatosis Index (HSI) scoring. This scoring was developed by Lee et al. to detect fatty liver with a specificity of 92.4%. It only uses simple data from laboratory results and physical examination. The formula of HSI is: (Formula 1)
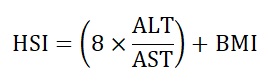
+ 2 if diabetic, +2 if female
HSI = Hepatic Steatosis Index
ALT = Alanine transaminase level
AST = Aspartate transaminase level
BMI = Body mass index
HSI can be interpreted as negative of NAFLD for scores below 30, positive of NAFLD for scores over 36, and inconclusive for scores between 30 and 35.9 [10]. The patients in this study were grouped into HSI < 36 and HSI ≥ 36.
Using univariate analysis, we determined the prevalence of NAFLD in patients with adenocarcinoma of colon and their baseline characteristics. The data obtained was then computed statistically in the bivariate analysis with the χ2 test or Kolmogorov Smirnov test with 95% confidence interval. A significant association was considered with a p-value of less than 0.05.
Results
A total of 84 patients were included in the study. Patients’ baseline characteristics are shown in Table 1.
| No. | Characteristic | Patient | % |
| 1 | Sex (n) | ||
| Male | 37 | 44 | |
| Female | 47 | 56 | |
| 2 | Age (x̄ , years old) | 55.9 | - |
| 3 | Weight (x̄ , kg) | 56.7 | - |
| 4 | Height (x̄ , cm) | 160.2 | - |
| 5 | AST (x̄ , U/L) | 28.3 | - |
| 6 | ALT (x̄ , U/L) | 20 | - |
| 7 | Diabetes (n) | ||
| Diabetes | 14 | 16.7 | |
| No Diabetes | 70 | 83.3 | |
| 8 | BMI (x̄ , Kg/m 2 ) | 22 | - |
| Normal BMI (n) | 67 | 79.8 | |
| High BMI (n) | 17 | 20.2 | |
| 9 | HSI (n) | ||
| HSI < 36 | 72 | 85.7 | |
| HSI ≥ 36 | 12 | 14.3 |
Histopathological features characteristics of patients are shown in Table 2.
| No. | Characteristic | n | % |
| 1 | Grading | ||
| Well | 42 | 50 | |
| Moderate | 37 | 44 | |
| Poor | 5 | 6 | |
| 2 | Extend of invasion | ||
| T1 | 2 | 2.4 | |
| T2 | 31 | 36.9 | |
| T3 | 39 | 46.4 | |
| T4 | 12 | 14.3 |
Table 1 shows that most of the patients were women (56%). The average age of patients was 55.9 years old. The mean body weight and height were 56.7 kg and 160.2 cm respectively. The majority of patients have a normal BMI (79.8%). Normal BMI was defined as BMI below 25. There were 20.2% of the patients with high BMI. 15 patients were overweight and 2 were obese. The HSI of each patient was calculated. 72 patients (85.7%) had HSI below 36 and 12 patients (14.3%) were positive of NAFLD according to HSI.
Table 2 shows that the majority of patients had well to moderate differentiation of adenocarcinoma (94% combined) and there was only a small percentage of patients with poorly differentiated adenocarcinoma (6%). Table 2 also shows a significant amount of patients with T2 and T3 stages (83.3% combined). There were 12 patients with T4 stage and only 2 patients with T1 stage of tumor invasion.
Cross tabulation and statistical analysis were conducted to determine any association between NAFLD and grading as well as the extend of invasion of the adenocarcinoma. The bivariate analyses are shown in Tables 3 and 4.
| No. | Variable | Grading | |||
| Well (n = 42) | Moderate to Poor (n=42) | p value* | OR (CI 95%) | ||
| 1 | HSI < 36 | 40 | 32 | 0,026 | 6,25 (1,277-30,58) |
| 2 | HSI ≥ 36 | 2 | 10 |
*Chi-square test, CI 95%
| No. | Variable | Extend of Invasion | p value* | |||
| T1 (n = 2) | T2 (n = 31) | T3 (n = 39) | T4 (n = 12) | |||
| 1 | HSI < 36 | 2 | 27 | 33 | 10 | 1 |
| 2 | HSI ≥ 36 | 0 | 4 | 6 | 2 |
*Kolmogorov Smirnov test, CI 95%
Table 3 shows that patients with well-differentiated adenocarcinoma were more likely to show low HSI scores. The number of patients with HSI over or equal to 36 was found to be greater in the moderate-poor differentiation group. Moderate and poor differentiation cells were combined because the number of patients with poorly differentiated adenocarcinoma was very low to meet the χ2 statistical analysis criteria (i.e. high number of cells with the expected count of less than 5). The combined cell resulted in a 0% of cells with the expected count of less than 5. Table 3 also shows the significance of the association between the two variables. The bivariate analysis showed a p-value of 0.026 with an odds ratio of 6.25 (95% CI 1.277-30.58).
Another bivariate analysis was also conducted between NAFLD and invasion depth (as shown in Table 4). Patients with HSI below 36 had various stages of invasion. This could influence the association significance between the variables. As the criteria for a χ2 test were not met, Kolmogorov Smirnov alternative test was conducted instead with a p-value of 1.
Discussion
The majority of the population with colon cancer are men as it is one of the risk factors of colon cancer [11]. Some studies also showed the high prevalence of colon cancer in men consistently [12, 13]. In this study, women had the higher number (56%). This discrepancy could be caused by the small number of samples that this study collected. Most previous studies used large samples (i.e. samples over 1000) and were conducted for a long period. This study only assessed 84 colon cancer patients in a short time so this could allow women to be the majority, although not significantly, in the current study.
Old age is also one of the risk factors of colon cancer [11]. According to literature, more than 90% of colon cancer patients have aged 50 and above [14]. The mean age in patients in this study was 55.9 years old. This finding is in line with one of the risk factors, aging. The mean age also falls into the category of early elderly age according to the Indonesian Ministry of Health.
This study found that 14.3% of the patients had NAFLD. A similar percentage is also found in a study conducted by Lin et al. (17,26%). In that study, patients’ fatty liver was assessed with abdomen ultrasonography (USG) (Lin et al., 2014). A cross-sectional study in the United States showed a small biopsy-proven fatty liver prevalence (1.6-10.5%) in patients with colon adenocarcinoma specifically [15]. The result of the current study showed a similar number with 2 studies that used 2 different modalities in detecting NAFLD. Biopsy remains the gold standard of NAFLD diagnosis, but this procedure is uncommon because oftentimes it does not have any clinical indication. USG, on the other hand, is the first-line modality in diagnosing NAFLD. This study was limited by the lack of USG performance for patients with colon cancer in DCNH, in which abdomen computed tomography (CT) is more preferred in recent years. CT is not able to display a good fatty liver presentation and therefore HSI was used instead as the alternative.
Ze et al. (2018) and Lee et al. (2020) investigated the association between fatty liver and colorectal tumors [16, 17]. Interestingly, both studies assessed the predictive value of Fatty Liver Index (FLI) for colorectal cancer, therefore they used FLI as the modality to detect fatty liver. A high tumor prevalence was found in patients with high FLI. It is also mentioned that FLI scores can be a predictor of colon adenomas or cancer [16, 17]. However, this study did not use FLI because it requires gamma-glutamyl transferase (GGT) and waist circumference. In DCNH, such examinations and tests are rarely conducted. This study used HSI that requires AST, ALT, BMI, and diabetic status which can be obtained easily. This makes HSI one of the simplest NAFLD scoring. Further studies on the predictive value of HSI for colon cancer can be conducted for establishing an easier colon cancer screening in the future.
The mechanism underlying the development of colon tumors in patients with NAFLD is not clearly understood. It is proposed that there are many factors involved in the growth of colon tumors by a fatty liver. Numerous cytokines such as adiponectin, TNF-α, interleukins, and MMP [3]. This cross-sectional study is limited to just explaining a phenomenon at one specific point of time. Lee et al. (2020) tried to establish a relation between NAFLD and colorectal cancer through a large retrospective cohort study. They found that patients with NAFLD can develop colorectal cancer after a 7.2-year follow-up with a hazard ratio of 1.23 [17]. This implies that NAFLD may be one of the causes of colon cancer development. More long-term studies are needed to form a stronger relation between NAFLD and colorectal cancer.
There was a significant association between NAFLD and grading (p = 0.026, OR = 6.25, 95% CI 1.277- 30.58). To our knowledge, there has been no study that specifically investigates the relation between NAFLD and colon cancer grading. However, Lin et al. (2014) found that 62.3% of NAFLD patients have poorly-differentiated colon cancer [13]. This significant number may explain the large number of moderate to poor differentiation patients with NAFLD in the current study.
This study also found that there was no significance in the association between NAFLD and extend of invasion (p = 1). Although not significant statistically, NAFLD may still cause a deeper invasion of colon cancer. This can be explained by the rise of MMP in a fatty liver [3] which one of its variants, MMP-9 affects tumor invasion and metastasis in the colon by inducing angiogenesis [9]. An Indonesian study has found a positive correlation between MMP-9 expression and tumor invasion depth in the colon. (r = 0.453). In the study, MMP-9 was found overexpressed in patients with stage T4 tumor and low in patients with stage T1 [18]. The usage of HSI and a low number of samples in this study may cause insignificance. Further evaluations with more patients and more conventional NAFLD detection instruments should be conducted to verify this relation.
This study has some limitations. First, this study did not take patients with more specific histopathology types such as mucinous or signet ring cell carcinomas which may add a little bit more patients to the study. We only took patients without specification or colon cancer in general (NOS). This was done to ensure that the study was consistent and did not widen to explain any relations between NAFLD and mucus overproduction or signet ring cell proliferation, for instance. Second, although USG is the best option for imaging fatty liver, there was a lack of USG data from the department of radiology in DCNH due to the lack of colon cancer patients undergoing USG. Because of this, we assessed patients’ livers with HSI instead. Third, HSI is a reliable tool to detect NAFLD, but there is a score range in which NAFLD is considered inconclusive (30-35.9). This might cause some patients with a score between the range to be undetected of NAFLD, even though they might have NAFLD if it was assessed by USG. It is also needed to assess further the usage of HSI in the Indonesian population. Lastly, this study was a cross-sectional study that still cannot determine which variable comes as the risk factor in the first place. This study is also unable to observe the progression of a disease in a high-risk population. It is very important to further assess the unclear relation of these 2 diseases prospectively, especially in countries where colon cancer is prevalent.
This study concludes that the prevalence of NAFLD in patients with adenocarcinoma of colon in Dharmais National Cancer Hospital from 2018-2019 was 14.3%. There was an association between NAFLD and grading and there was no association between NAFLD and the extend of invasion.
Acknowledgements
General: The authors extend thanks to Dharmais National Cancer Hospital for providing all medical records needed and giving insights so this study can be completed.
Funding Statement
The study received no funding.
Approval
The study was approved by the Deanship of Faculty of Medicine, Universitas Pembangunan Nasional Veteran Jakarta, Indonesia.
Conflict of Interest
Ethical Declaration
This study has been reviewed and was approved by the Committee of the Medical Research Ethics of Dharmais National Cancer Hospital (109/KEPK/XI/2021) in accordance with the ICH-GCP standard.
Authors Contribution
The authors contributed equally to the process of the study.
Data Availability
Data is not publicly available due to ethical reasons. However, it is obtainable through the corresponding author on reasonable request.
References
- Global Cancer Observatory: Cancer Today [WWW Document]. Ferlay J, Ervik M, Lam F. Int. Agency Res. Cancer. URL http://gco.iarc.fr/today (accessed 1.18.22).2020.
- The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases Chalasani Naga, Younossi Zobair, Lavine Joel E., Charlton Michael, Cusi Kenneth, Rinella Mary, Harrison Stephen A., Brunt Elizabeth M., Sanyal Arun J.. Hepatology (Baltimore, Md.).2018;67(1). CrossRef
- Association between non-alcoholic fatty liver disease and colorectal cancer Parizadeh Seyed Mostafa, Parizadeh Seyed Alireza, Alizade-Noghani Mohadese, Jafarzadeh-Esfehani Reza, Ghandehari Maryam, Mottaghi-Moghaddam Ali, Goldani Fatemeh, Khazaei Majid, Ghayour-Mobarhan Majid, Ferns Gordon A., Hassanian Seyed Mahdi, Avan Amir. Expert Review of Gastroenterology & Hepatology.2019;13(7). CrossRef
- Prevalence and Profile of Fibrosis in Diabetic Patients with Non-alcoholic Fatty Liver Disease and the Associated Factors Prasetya Ignatius Bima, Hasan Irsan, Wisnu Wismandari, Rumende Cleopas Martin. Acta Medica Indonesiana.2017;49(2).
- Obesity and visceral fat in Indonesia: An unseen epidemic? A study using iDXA and surrogate anthropometric measures Smith Marc K., Christianto Erwin, Staynor Jonathan M. D.. Obesity Research & Clinical Practice.2021;15(1). CrossRef
- Non-alcoholic fatty liver disease and colorectal cancer Mikolasevic I., Orlic L., Stimac D., Hrstic I., Jakopcic I., Milic S.. Postgraduate Medical Journal.2017;93(1097). CrossRef
- Liver fatty acid-binding protein: a marker for studying cellular differentiation in gut epithelial neoplasms Carroll S. L., Roth K. A., Gordon J. I.. Gastroenterology.1990;99(6). CrossRef
- Hepatocyte and stellate cell deletion of liver fatty acid binding protein reveals distinct roles in fibrogenic injury Newberry Elizabeth P., Xie Yan, Lodeiro Carlos, Solis Roberto, Moritz William, Kennedy Susan, Barron Lauren, Onufer Emily, Alpini Gianfranco, Zhou Tianhao, Blaner William S., Chen Anping, Davidson Nicholas O.. FASEB journal: official publication of the Federation of American Societies for Experimental Biology.2019;33(3). CrossRef
- Cholic Acid Stimulates MMP-9 in Human Colon Cancer Cells via Activation of MAPK, AP-1, and NF-κB Activity Li Shinan, Ung Trong Thuan, Nguyen Thi Thinh, Sah Dhiraj Kumar, Park Seon Young, Jung Young Do. International Journal of Molecular Sciences.2020;21(10). CrossRef
- Hepatic steatosis index: a simple screening tool reflecting nonalcoholic fatty liver disease Lee Jeong-Hoon, Kim Donghee, Kim Hwa Jung, Lee Chang-Hoon, Yang Jong In, Kim Won, Kim Yoon Jun, Yoon Jung-Hwan, Cho Sang-Heon, Sung Myung-Whun, Lee Hyo-Suk. Digestive and Liver Disease: Official Journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver.2010;42(7). CrossRef
- Colorectal cancer Dekker Evelien, Tanis Pieter J., Vleugels Jasper L. A., Kasi Pashtoon M., Wallace Michael B.. Lancet (London, England).2019;394(10207). CrossRef
- Non-alcoholic fatty liver diseases and risk of colorectal neoplasia Ahn J. S., Sinn D. H., Min Y. W., Hong S. N., Kim H. S., Jung S.-H., Gu S., Rhee P.-L., Paik S. W., Son H. J., Gwak G.-Y.. Alimentary Pharmacology & Therapeutics.2017;45(2). CrossRef
- Increased risk of colorectal malignant neoplasm in patients with nonalcoholic fatty liver disease: a large study Lin Xian-Feng, Shi Ke-Qing, You Jie, Liu Wen-Yue, Luo Ying-Wan, Wu Fa-Ling, Chen Yong-Ping, Wong Danny Ka-Ho, Yuen Man-Fung, Zheng Ming-Hua. Molecular Biology Reports.2014;41(5). CrossRef
- Risk Factors for Colorectal Cancer Khosama Y. Cermin Dunia Kedokt.2015;42:829-832.
- Increased Prevalence of Colorectal Adenomas in Patients with Nonalcoholic Fatty Liver Disease: A Cross-Sectional Study Blackett John William, Verna Elizabeth C., Lebwohl Benjamin. Digestive Diseases (Basel, Switzerland).2020;38(3). CrossRef
- The Fatty Liver Index: A Simple and Accurate Predictor of Colorectal Adenoma in an Average-Risk Population Ze Eun Young, Kim Beom Jin, Jun Dong Hwan, Kim Jae Gyu, Kang Hyun, Lee Dong Young. Diseases of the Colon and Rectum.2018;61(1). CrossRef
- The association between nonalcoholic fatty liver disease and esophageal, stomach, or colorectal cancer: National population-based cohort study Lee Jung-Min, Park Yong-Moon, Yun Jae-Seung, Ahn Yu-Bae, Lee Kang-Moon, Kim Dae Bum, Lee Ji Min, Han Kyungdo, Ko Seung-Hyun. PloS One.2020;15(1). CrossRef
- Matrix Metalloproteinase-9 Expression Correlates Positively with Depth of Invasion of Colorectal Adenocarcinoma Shinta HE, Artha IGA, Saputra H. Indones. J. Pathol.2019;28:22-27.
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2022
Author Details