“See and Treat” an Advocated Approach for Precancerous Lesions of the Cervix- A North Indian Referral Center Based Randomized Control Trial
Download
Abstract
Objective: To establish the comparability of two step approach of See and treat with the conventional three step approach In management of Precancerous lesions of the cervix.
Methods: A Randomised controlled Trial was conducted in AIIMS Rishikesh over a period of one year (2020-2021). All women presenting to OPD in age group 25-60 years were screened with PAP smear and per speculum examination, and women with Abnormal PAP smear or clinically unhealthy cervix were subjected to colposcopy. Reid and Swede scores were calculated and colposcopy guided biopsy taken. Women with CIN2/3 on either of the colposcopy scores were randomized to two or three step approach. Women falling into two step approach (group A) underwent LEEP in the same sitting while the latter group (group B) was told to follow up with histopathology reports for further management.The final histopathological diagnosis and LEEP results were compared.
Results: Overtreatment rates were 22% in see and treat approach, distributed as 3.6% in HSIL + ASC_H group and 33 % in LSIL patients. None were lost to treatment in this group. 39 out of 50 women in Group B needed definitive treatment after their biopsy results and 48% of them were lost to follow up. 72% were adequately treated in group A while only 22 % could be adequately treated in Group B.
Conclusion: It can thus be safely concluded that despite the risk of overtreatment, a two step approach should be considered for preventive management, especially considering the rate of loss to follow up in three step approach. This study thus advocates the use of See and Treat protocol, especially in the high-grade cytology lesions. IN low risk cases too, the study proposes that see and treat protocol can be used, albeit with good clinical judgement. Offering opportunities to reduce suffering associated with the eminently preventable cervical cancer is an ethical imperative and the SEE and TREAT approach is an attempt in that early preventive direction.
Introduction
Cervical cancer is the 4th most common cancer in women with an estimated 570,000 new cases and 311,000 deaths in 2018 representing 6.6% of all female cancers. India and China together contribute more than a third of this global cervical burden, with 97000 cases and 60000 deaths in India in 2018 [1]. When diagnosed, cervical cancer is one of the most successfully treatable forms of cancer, as long as it is detected early and managed effectively. Cancers diagnosed in advanced stages can also be controlled with multidisciplinary treatment and palliative care.
Cervical cancer is the only gynecological cancer that satisfies the World Health Organization (WHO) criteria for implementation of a screening program. The long interval between infection and the development of invasive cervical carcinoma provides the benefit of scope for screening and secondary prevention. Yet, the unequal burden of cervical cancer is a simple example of the impact of unequal access to health care. Evidence is emerging from developing countries on the burden of loss to follow-up care after a positive cervical cancer screening/diagnosis, which impacts negatively on cervical cancer prevention and control [2]. Improving secondary prevention of cervical cancer should remain a key priority for women’s health globally for decades to come, especially in developing countries. A see-and-treat procedure is thus a step towards the same, It omits the step of colposcopic guided biopsy and minimizes the chances of lost to follow up. Patients undergo colposcopy and Loop electrosurgical excision procedure when indicated at the same time after receipt of a cytology report with cervical dysplasia. This procedure avoids noncompliance and false negative colposcopy biopsies and eases patient’s anxiety along with cutting down treatment costs [3,4]. The conventional three step approach involves a screening visit, a second visit for colposcopy and directed biopsy and the third visit for treatment of histopathologically proven cervical intraepithelial neoplasia (CIN) cases. With a comprehensive approach to screen and treat, cervical cancer can be eliminated as a public health problem within a generation.
Keeping in mind the existent screening and treatment lacunae and need for improved secondary prevention, the present study was planned with an objective to advocate the “See and treat approach” for preinvasive lesions of the cervix. The present study thus aims to establish the efficacy of see-and-treat approach over the conventional three step approach, in treating cervical intraepithelial neoplasia.
Materials and Methods
The present study was a Randomized control trial (CTRI/2020/05/025241) done in 100 patients of colposcopy-suspected CIN in whom two protocols of management were compared. The trial was conducted in the Department of Obstetrics and Gynecology, All India Institute of Medical Sciences (AIIMS), Rishikesh for a period of one year. Ethics clearance was obtained from Institutional ethics committee, AIIMS Rishikesh. (AIIMS/ IEC/19/691). Simultaneously correlation of clinical and cytological findings was done with their histopathology findings. Women aged 25-60 years who were suspected to have CIN by Abnormal screening results (PAP smear with Atypical squamous cells of undetermined significance (ASCUS) or worse, positive HPV DNA testing, positive Visual inspection after acetic acid or visual inspection with Lugol’s iodine) OR with history of post coital bleeding or clinically unhealthy cervix on per speculum examination or persistent discharge P/V, were subjected to colposcopy. If the colposcopy suggested high grade lesion, (Reid score>6 or Swede score>5), they were then included in the study. Women with visible growth on cervix, severe debilitating disease, history of pelvic irradiation, low-grade lesion on colposcopy, pregnant women or women who were unable to give informed consent, were excluded from the study. If the lesion appeared low grade on colposcopy, they were not included in the study. Only high grade squamous intra epithelial lesions on colposcopy were included. All included women were then randomized by simple randomization into Group A (See and Treat approach or 2 step approach) and Group B (conventional 3 step approach). They were allocated to the two treatment groups by computer generated randomization table. Random number Table (online) was used to assign a case number from 1-100 for each recruited case. The random number table was concealed, and only upon each recruitment the next online case number was generated.
Using the GRAPHPAD, an online software, each case number was pre-designated randomly to either Group A or Group B. They thus underwent simple randomization at two levels, and based on the group assigned, were offered further management. Further, the number generation and assignment to group was done by a nursing officer, thus keeping the investigators and participants blinded from the same.
Women in the group A, of See-and-treat modality, with CIN2/3, according to any one or both of the Colposcopy scores (Reid and Swede), underwent LEEP/ Thermal ablation/Conization in the same sitting. In case of discrepancy between the Reid Swede score regarding the grading of CIN, the higher score was considered, and patient was provided the treatment accordingly in the same sitting. Tissue obtained from these procedures was sent for Histopathological examination. Women were followed up after 1 week with their final histopathological diagnosis report (post LEEP/Thermal Ablation/ conization). They were considered Adequately Treated if HPE report was CIN 2/3 and margins were negative, Under-treated if HPE report was Invasive carcinoma, and Over treated if LEEP/ conisation specimen HPE report was CIN 1 or chronic inflammation or with no evidence of dysplasia. Women who did not return for follow up with HPE reports post procedure were considered as lost to follow up.
Women in Group B followed conventional three step treatment modality. They underwent colposcopy and guided biopsy from suspicious areas on colposcopy. They were told to follow up with the histopathology reports of the colposcopically guided biopsy for further management and were advised definitive procedure according to the histopathological report. Women who did not follow upwith biopsy report for further definitive treatment were considered as lost to follow up.
The pathologist reviewing the histopathology specimen of LEEP was not aware of which group the patient belonged to. Women undergoing see and treat approach, by the modality of thermal ablation, underwent a colposcopy biopsy as well, to ensure Histopathology report for comparison of results.
The study population was analysed for their demographic and clinic-pathological parameters. Also, the two study groups were compared finally in terms of initial cytology, final histopathology, adequacy of management, rates of overtreatment and rates of loss to follow up.
Sample size was estimated, taking the study done by N Guducu et al [5], as reference and the two proportions of cytological abnormalities which were concluded to be CIN2/3 after treatment by three-step-method vs after treatment by see-and-treat, were taken as the comparing proportions to calculate the sample size for the present study using the following formula:
n = (Zα/2+Zβ) 2 * (p1(1-p1) +p2(1-p2)) / (p1-p2) 2
where Zα/2 is the critical value of the Normal distribution at α/2 (for the confidence level taken of 95%, α is 0.05 and the critical value is 1.96) and Zβ is the critical value of the Normal distribution at β (for the power of 80%, β is 0.2 and the critical value is 0.84) and p1 and p2 are the expected sample proportions of the two groups. When P1: 19 %, P1 being the Proportion of CIN 2/3 on see-and-treat, out of smear result ASCUS+ LSIL and P2: 48.4 %, P2 being the Proportion of CIN 2/3 on three step treatment, out of smear result ASCUS+ LSIL ; then the sample size was calculated as 37 . OR when P1: 100 %, P1 being the Proportion of CIN 2/3 on see- and-treat, out of smear result ASC-H and P2:81.8%P2: being the Proportion of CIN 2/3 on three step treatment, out of smear result ASC-H; then the minimal sample size was calculated as 36. We included a sample size of 100 patients in the study.
Data were coded and recorded in MS Excel spreadsheet program. SPSS v23 (IBM Corp.) was used for data analysis. Group comparisons for continuously distributed data were made using independent sample ‘t’ test when comparing two groups, and One-Way ANOVA when comparing more than two groups. Chi-squared test was used for group comparisons for categorical data. In case the expected frequency in the contingency tables was found to be <5 for >25% of the cells, Fisher’s Exact test was used instead. Statistical significance was kept at p < 0.05.
Results
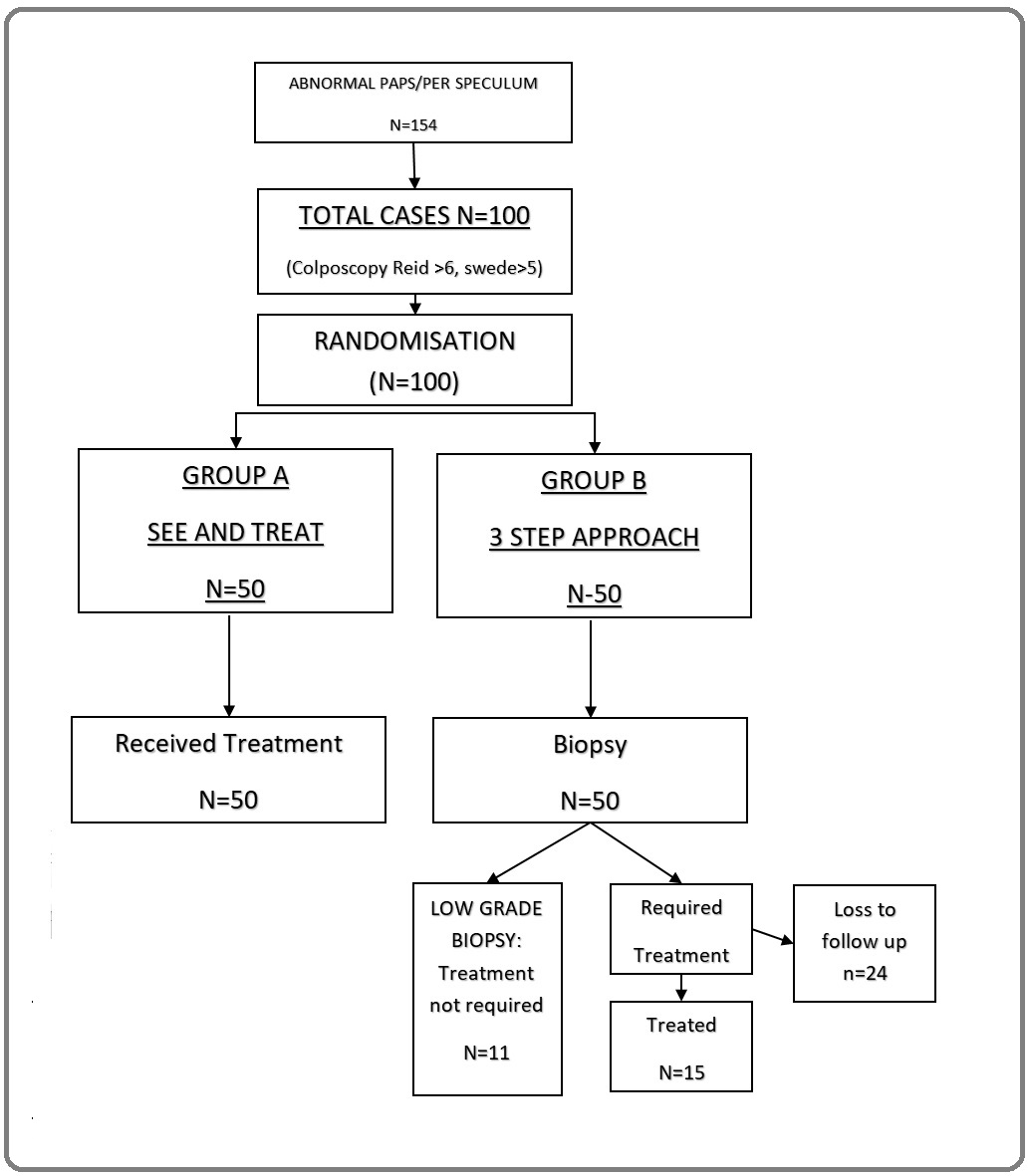
The study population was screened with clinical history, per speculum examination and pap smear testing. A total of 154 patients were screened from 2020 to 2021. On an abnormal screening test, patients were subjected to colposcopy.100 patients with high grade squamous intraepithelial lesions on colposcopy (Reid>6 Swede >5) were recruited in the study as per inclusion and exclusion criterion and were randomized into two groups of treatment, See and Treat (Group A) and Conventional 3 Step method (Group B). All 50 patients of Group A received treatment according to colposcopy findings at the same sitting while in Group B, 24 out of 50 patients were lost to follow up after the biopsy. Of the remaining 26, 11 did not require any treatment. Only 15 patients in Group B could be subjected to definitive treatment like LEEP, Cold knife conisation or cryotherapy (Figure 1).
Figure 1. Participant Flow Diagram Showing Screening, Recruitment and follow up.
Socio demographic and clinical characteristics of study participants are depicted in Table 1 and 2 respectively.
| Parameters | Group | p value | ||
| A | B | |||
| (n = 50) | (n = 50) | |||
| Age (Years) | 45.20 ± 9.96 (%) | 49.18 ± 10.80 (%) | 0.058 | |
| Age*** | 0.006 | |||
| 20-29 Years | 1 (2.0) | 1 (2.0) | ||
| 30-39 Years | 13 (26.0) | 11 (22.0) | ||
| 40-49 Years | 24 (48.0) | 10 (20.0) | ||
| 50-59 Years | 6 (12.0) | 19 (38.0) | ||
| 60-69 Years | 6 (12.0) | 8 (16.0) | ||
| 70-79 Years | 0 (0.0) | 1 (2.0) | ||
| Occupation | 0.824 | |||
| Housewife | 40 (80.0) | 43 (86.0) | ||
| Professional | 5 (10.0) | 4 (8.0) | ||
| Skilled Worker | 2 (4.0) | 2 (4.0) | ||
| Unskilled Worker | 3 (6.0) | 1 (2.0) | ||
| Education | 0.285 | |||
| Illiterate | 7 (14.0) | 9 (18.0) | ||
| Primary | 9 (18.0) | 10 (20.0) | ||
| Middle | 3 (6.0) | 0 (0.0) | ||
| High School | 6 (12.0) | 1 (2.0) | ||
| Intermediate | 14 (28.0) | 16 (32.0) | ||
| Graduate | 10 (20.0) | 13 (26.0) | ||
| Postgraduate | 1 (2.0) | 1 (2.0) |
| Chief Complaint | Group A (%) | Group B (%) | P value |
| Asymptomatic | 1 (2.0) | 2 (4.0) | 0.273 |
| Discharge P/V | 7 (14.0) | 8 (16.0) | |
| Dyspareunia | 4 (8.0) | 4 (8.0) | |
| Intermenstrual Bleeding | 7 (14.0) | 10 (20.0) | |
| Irregular Cycles | 1 (2.0) | 4 (8.0) | |
| Pelvic Pain | 14 (28.0) | 10 (20.0) | |
| Post-Coital Bleeding | 12 (24.0) | 4 (8.0) | |
| Post-Menopausal Bleeding | 4 (8.0) | 8 (16.0) | |
| Age at Menarche (Years) | 14.04 ± 1.16 | 13.74 ± 1.03 | 0.194 |
| Parity | 0.823 | ||
| P1 | 2 (4.0) | 2 (4.0) | |
| P2 | 21 (42.0) | 16 (32.0) | |
| P3 | 15 (30.0) | 19 (38.0) | |
| P4 | 8 (16.0) | 7 (14.0) | |
| P5 | 2 (4.0) | 4 (8.0) | |
| P6 | 1 (2.0) | 2 (4.0) | |
| P7 | 1 (2.0) | 0 (0.0) | |
| H/o Multiple Partners (Present) | 1 (2.0) | 0 (0.0) | 1 |
| Age at First Intercourse (Years) | 20.36 ± 1.45 | 20.12 ± 1.41 | 0.422 |
Mean age of the study participants was 47.19 +- 10.53 years. Literacy had a positive correlation with women who came for follow up. Maximum women who did not follow up were housewives but the association between occupation and rates of follow up was not significant. (Tables 1 and 2).
In Group A, it was observed that 11 of 50 (22%) patients were overtreated. Overtreatment rates were 3.6% in HSIL + ASC_-H group and 33 % in LSIL group. No patients were lost to follow up in Group A as they were treated in the same step as colposcopy.
In Group B, 39 out of 50 women needed definitive treatment after their biopsy results, but 24 out of 50 (48%) women in Group B were lost to treatment as they did not follow up with biopsy results.
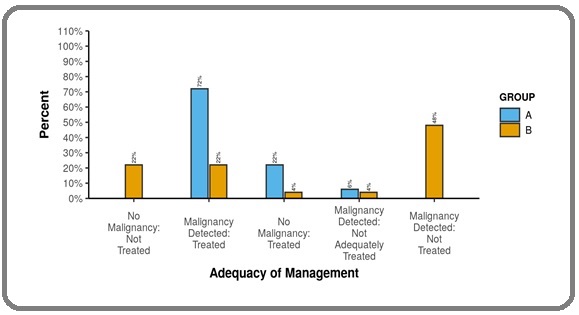
When comparing the adequacy of treatment between the two groups, 36 out of 50 (72%) were adequately treated in group A while only 11 out of 50 (22 %) could be adequately treated in Group B. There was a statistically significant difference between the two groups in terms of Adequacy of Management (X2 = 54.729, p = <0.001). Participants in Group A had the larger proportion of being adequately treated while participants in Group B had the larger proportion of lost to follow up with no definitive treatment done for 24 out of 50 patients (Figure 2).
Figure 2. Comparison of Adequacy of Management in Group A and Group B.
Other associated parameters were also studied. Per speculum findings were analyzed and their accuracy was determined using histopathology as the gold standard and were accurate in 67/100 cases. Per speculum examination was concluded as an important screening tool due to the high association of abnormal findings with risk of CIN. Pap smear accuracy in High grade colposcopy lesions was 91.4 % and HSIL was the most common finding. In the entire study population (n=100), 76 % had CIN 2+ lesions, 6 % had CIN 1and 17% had no evidence of dysplasia. 1 % was inadequate. 54 % women underwent LEEP, 9 % underwent cryotherapy and 2 % underwent conization.
Discussion
Cervical cancer is a major cause of female morbidity and mortality around the world and has been a subject for active research in the past few decades. As primary prevention, behavioral modifications and HPV vaccines are being promoted, and as a secondary prevention the early diagnosis and treatment of cervical precancerous lesions is being encouraged.
The ability of a patient to attend a screening or colposcopy clinic, and then to return for possible treatment, and further to return to clinic for follow-up evaluation (“the patient factor”) is an important component to the success of any program. The patient factor has not been addressed enough in the discussion of cervical cancer screening or treating techniques and guidelines. The justifiable excitement over primary prevention by vaccination should be combined with treating those who have already inflicted the virus and could be on a possible downhill path towards invasive disease, albeit have the time in hand to halt the progression at the stage of Cervical Intraepithelial neoplasm.
With this backdrop, the present randomized control trial was conducted. This study screened 154 women and included 100 women (with colposcopy suggestive of high-grade lesion). Recruited women were subjected to secondary prevention i.e LEEP with or without cervical biopsy (Group B and Group A respectively).
Per speculum examination was a screening tool used, other than Pap smear. Upon reviewing the literature, it was found that abnormal per speculum examination was not commonly included as a cause of referrals in previous studies [6]. The present study includes abnormal per speculum examination, which was present in majority of women, as a screening tool for colposcopic referrals. In most of the cases of an abnormal cervix, the Pap smear was also abnormal. Yet this wasn’t true for all. Cases with unhealthy cervix but a normal PAP smear with a high-grade lesion on colposcopy, had CIN2+ in two thirds of cases. This clearly defines the importance of clinical examination, as an adjunct with colposcopy, to improve screening and defies the sole dependence on PAP smear as screening tool, especially in low resource settings. The present study thus advocates using clinical suspicion as an important adjunctive tool. Larger studies can further validate the strength of per speculum examination.
The screened patients were subjected to colposcopy and randomised into Group A (50- see and Treat) and Group B (50- 3 Step Approach). Management protocols and histopathology results were analysed. Group A (See and treat) had the possibility of overtreatment as no histopathological diagnosis was available at the time of treatment. Overall, 22% cases were over treated in Group A. The overtreatment rates of the present study are comparable to a retrospective study by Bosgraaf et al. They included 3192 women and aimed to examine the referring Pap smear result, colposcopy impression, and final histopathologic interpretation on the large loop electrical excision of the transformation zone (LLETZ) specimen for the population treated by See and treat. The over-treatment rate was 18.1%, similar to the present study [7].
In the present study, overtreatment rates were higher for LSIL as compared to HSIL. In Group A, ASCUS and LSIL had an overtreatment rate of 30 % while HSIL and ASC-H had an overtreatment rate of only 3.6 %. In scenarios where follow up and patient compliance is dependable , overtreatment can further be significantly kept in check by recruiting only the high-grade lesions to See and Treat, owing to the dependability on follow-up for the low grade lesions. Yet, in developing countries, owing to poor compliance due to multiple factors, the benefit of see and treat in HSIL and LSIL cases (with certain level of overtreatment) still outweighs the disadvantage of loss to treatment and follow up in the conventional 3 step approach. Colposcopy after cytology before management, in such scenarios, helps keeping the overtreatment further under check. Guducu et al found overtreatment rates in HSIL as high as 23%, which were higher than the present study. ASC-H had no overtreatment in their study while ASCUS + LSILwas overtreated to the extent of 81 %, much higher than the current study [5]. Monteiro et al recruited only those women who had HSIL on pap smear and the overtreatment rates were 2 % which was comparable to the present study [8].
Group B (3 step approach) had the possibility of loss to treatment. 39 out of 50 women (78 %) required treatment based on histopathological reports out of which 24 women (61.5%) were lost to treatment. 3 women with invasive malignancy on biopsy were also lost to treatment. Overall, Group B had a loss to treatment rate of 48 %. Studies suggest the loss to treatment depends upon multiple factors. The lack of easily accessible health facilities or the anxiety developed after the first colposcopy and biopsy visit are few of the many factors responsible. Megevand et al described that in PHASE 1, when colposcopy and treatment were not offered at the same site, the defaulter rate was 66 %. This defaulter rate was minimalized when the PHASE 2 trial offered treatment at the same site [9]. Thus, minimizing loss to treatment is a propelling factor to propose the See and treat approach.
All women with HSIL and a high grade colposcopic lesion, had a histopathology suggestive of premalignant or malignant lesions thereby reinforcing PAP smear and Colposcopy as a highly specific and efficient tool for screening high grade lesions. The importance of colposcopy can be further ascertained by seeing the contrasting higher overtreatment rates (16 % in HSIL) in the study conducted by Numnum et al, where HSIL on cytology was treated irrespective of their colposcopy scores [10]. Kjellberg et al, found sensitivity for HSIL out of cytology and colposcopically directed biopsy as 74.4 and 73.3%, respectively. Similar to the present study, they also emphasized the strategy of immediate LEEP after HSIL Pap smear and high-grade colposcopy owing to their high sensitivity [11] (Table 3).
| Study | Sample Size | Overtreatment in LSIL | Overtreatment in HSIL |
| Guduchu/ | 116 | ASC-US+LSIL: 81% | ASC-H:0% |
| Turkey | HSIL 22.3% | ||
| Cho/S Korea | 829 | LSIL+ASC-US :82.1% | 18% |
| Ingkapairog | 302 | -- | 52.80% |
| Monteiro/Brazil | 900 | LSIL+HSIL: 6.7% | 2% |
| Megevand/S. Africa | 2.10% | 3% | |
| Numnum/Birmingham | 51 | -- | 16% |
| Bosgraaf/Netherlands | 3192 | 29.20% | 4.5% (high grade colposcopy |
| 28.6% (low grade colposcopy) | |||
| Kittipat/Thailand | 55 | -- | 4% |
| Singla/India | 16 | -- | 13% |
| Current Study/India | 100 (50) | LSIL: 33% | HSIL :0% HSIL+ASC-H:3.6% |
| LSIL+ASC-US: 30% |
After thorough analysis, we conclude that a significant difference exists in the adequacy of management between the two groups ( Group A 72 % vs Group B 22 %). The present study thus advocates the use of See and Treat protocol, especially in the high-grade cytology lesions. In low risk cases too, the study proposes that see and treat protocol can be used, albeit with prudent clinical judgement. Limited studies have compared the treatment protocols in low grade cytology cases, and further studies can validate the use of See and Treat protocol for patients with LSIL and ASCUS.
The drawbacks of the study were a possibility of subjective bias at the level of the colposcopist and a limited sample size. Lack of HPV test as a screening tool, due to institutional non availability was also a possible setback to the screening. Also, the efficacy of these treatment modalities and their follow up could be studied further. The strengths of the study included trained operators for each step minimising operator bias and use of different pathologists to review the cytology and histopathology thereby removal of observer bias. In addition, another strength was the use of multiple screening tools, including cytology as well as visual inspection of the cervix which ensured inclusion of maximum eligible participants. This study thus advocates the adjunctive use of visual per speculum inspection of cervix in further studies as well. In conclusion, Efforts should continue to inspire women to undergo screening and ensure early detection with treatment of the disease. The socio-economic dynamics of the population as well as health care facilities should guide the ideal management, and hence See And Treat management has its place. A successful reduction in disease burden could be achieved when patients and clinicians strive for it together. The See and Treat protocol reiterates that reduction in loss to follow up and readily available access to health care facilities should go hand in hand to conquer this disease.
Authorship Declaration
All authors are in agreement with the content of the manuscript. Dhriti kapur, Amrita Gaurav, Kavita Khoiwal, Sandipan Chowdhuri and Jaya Chaturvedi have managed the clinical aspect and patient management related to the trial. Smrati Sabnani and Shreya Panda have handled data management and drafting the manuscript. All the authors have proofread the manuscript and agreed to the final version. All the authors have no conflicts of interest or financial ties to disclose.
References
- Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis Arbyn M, Weiderpass E, Bruni L, Sanjosé S, Saraiya M, Ferlay J, Bray F. The Lancet Global Health.2020;8(2). CrossRef
- Loss to Follow-Up in a Cervical Cancer Screening and Treatment Program in Western Kenya Kiptoo S., Otieno G., Tonui P., Mwangi A., Orango O., Itsura P., Muthoka K., Oguda J., Rosen B., Loehrer P., Cu-Uvin S.. Journal of Global Oncology.2018;4(Supplement 2). CrossRef
- Anxiety caused by abnormal result of cervical smear test: a controlled trial Wilkinson C., Jones J. M., McBride J.. BMJ (Clinical research ed.).1990;300(6722). CrossRef
- Colposcopy E-Book: Principles and Practice Apgar BS , Brotzman GL , Spitzer M. Elsevier Health Sciences.2008;:555 p.
- Three-step approach versus see-and-treat approach in patients with cytological abnormalities Guducu N, Sidar G, Bassullu N, Turkmen I, Dunder I. International Journal of Clinical and Experimental Medicine.2013;6(5).
- One-step management of cervical lesions Darwish A, Gadallah H. International Journal of Gynecology & Obstetrics.1998;61(3). CrossRef
- Overtreatment in a see-and-treat approach to cervical intraepithelial lesions Bosgraaf RP , Mast P, Struik-van der Zanden PHTH , Bulten J, Massuger LFAG , Bekkers RLM . Obstetrics and Gynecology.2013;121(6). CrossRef
- Effectiveness of see-and-treat for approaching pre-invasive lesions of uterine cervix Monteiro ACS , Russomano F, Reis A, Camargo MJ , Fialho SA , Tristão MA , Soares T. Revista De Saude Publica.2009;43(5). CrossRef
- Can cervical cancer be prevented by a see, screen, and treat program? A pilot study Megevand E., Van Wyk W., Knight B., Bloch B.. American Journal of Obstetrics and Gynecology.1996;174(3). CrossRef
- A prospective evaluation of "see and treat" in women with HSIL Pap smear results: is this an appropriate strategy? Numnum TM , Kirby TO , Leath CA , Huh WK , Alvarez RD , Straughn JM . Journal of Lower Genital Tract Disease.2005;9(1). CrossRef
- 'See and treat' regime by LEEP conisation is a safe and time saving procedure among women with cytological high-grade squamous intraepithelial lesion Kjellberg L, Tavelin B. Acta Obstetricia Et Gynecologica Scandinavica.2007;86(9). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2022
Author Details