Correlation of P53 Expression with Clinicopathological Parameters, Hormone Receptors and HER 2 Neu Status in Breast Carcinoma
Download
Abstract
Background: Progesterone receptor (PR), estrogen receptor (ER) expression, human epidermal growth factor 2 (HER 2 neu) amplification/ overexpression, and p53 nuclear protein accumulation are all significant prognostic biomarkers in breast cancer (BC). This work aims to assess the co-presence of p53 overexpression with ER, PR, and HER 2 neu expression in invasive BC specimens by IHC and compare their expression with various clinicopathological features.
Objectives: To evaluate the expression of ER, PR, HER-2neu and p53 in invasive breast carcinoma specimens and to correlate the expression of p53 with ER, PR, HER-2 neu and the clinicopathological parameters.
Methods: Cases of Modified Radical Mastectomy received from June 2015 to May 2017 were studied. In addition to hematoxylin and eosin sections, immunohistochemical staining was done for ER, PR, HER 2 neu and p53. The expression of ER, PR, HER 2 neu and p53 was noted and the findings were correlated with other clinicopathological parameters.
Results: Among 86 cases studied most of them belonged to the age group 41-60 years (54, 62.8%). A significant positive correlation of p53 over expression with ER and PR positive tumours and Triple Negative tumours was noted. Also p53 overexpression showed a positive significant correlation with tumour grade.
Conclusion: P53 overexpression in breast carcinoma indicates an aggressive clinical course and can be used as a marker of poor prognosis.
Introduction
Breast carcinoma is the most prevalent malignancy worldwide in females and is one of the primary reason for mortality in women. It currently accounts for one out of every four malignancies in women [1]. In India, 118000 incident cases were reported in 2016, according to estimates with a 95% confidence level [2].
The tumor’s size, type, and grade as well as the condition of its lymph nodes determine the prognosis. Hormone receptor status like estrogen receptor (ER), progesterone receptor (PR) and human epidermal growth factor receptor 2 (Her2/neu) expression are universally employed as biomarkers for breast cancer and are analysed using Immunohistochemistry (IHC) [1]. In 1987, it was discovered that the HER-2/neu proto-oncogene was amplified, overexpressed, and related with a worsening of prognosis and reduced survival in 20–30% of invasive breast tumours [3].
HER 2 neu overexpression is associated with poor survival, but its main importance is as a predictor of response to agents that target this transmembrane protein (e.g. Trastuzumab or Herceptin [4].
The development of breast cancer involves a progression through intermediate stages until the invasive carcinoma and finally into metastatic disease. The usual surgical procedure for breast cancer is modified radical mastectomy, although the outcome after surgery varies widely. Apart from clinical parameters like age, menopausal status and disease presentation, important prognostic indicators in histopathology are tumor size and extent, histologic grade and lymph node status. In addition, there are other factors which not only are predictive, but also direct therapies against particular molecular targets [5].
The current therapeutic approaches for breast carcinoma consist of combinations of surgery, post- operative radiation, hormonal treatment, chemotherapy and trastuzumab. The choice between hormonal therapy which has minimal side effects and chemotherapy which has high morbidity and risks is a major responsibility of the clinician. Therefore, an accurate assessment of ER, PR and HER 2 neu status of breast cancers by the pathologist is very essential [6].
Hence, this study aimed to establish a correlation of p53 with ER and PR status and HER 2 neu overexpression, lymph node status, clinical features and tumor histopathology and to effectively use the results to prognosticate and treat invasive breast cancer patients.
Materials and Methods
The study was undertaken at a tertiary care hospital in Bangalore, Karnataka. A total of 86 invasive breast cancer cases which were diagnosed over a period of 23 months between June 2015-May 2017 were studied. Females of all age group were included in the study. Cases where only a trucut biopsy or a limited surgery has been done and in cases where there was extensive tumour necrosis without sufficient viable tumour cells for accurate evaluation of the IHC results were excluded from the study. Detailed history, clinical data and laboratory investigations were collected for each cases. All tissues were fixed in 10% buffered formalin for not more than 24 hours.
Representative tumor tissue was submitted for processing and H&E stain for routine histological diagnosis according to modified Bloom Richardson grading system of WHO. IHC for ER, PR and Her-2/neu were performed on representative blocks of paraffin embedded tissue. For IHC staining 4 μm thick sections were submitted. Sections were taken on slides previously coated with poly L lysine. Antigen retrieval was done by HIER method using Citrate buffer at PH 2.5 for ER/PR and PH 6 for HER 2 neu. The normal epithelial component was served as internal control for ER/PR. IDC with known HER 2 neu over lot of staining. The ER and PR results were screened and interpreted as positive when more than 1% of tumor cells showed positive nuclear staining. For interpretation of HER 2 neu staining in each case, the proportion of positive staining tumour cells (expressed in percentage) and the average intensity of staining (expressed as 0, 1+, 2+ or 3+) was evaluated. The relationship between various parameters such as age, duration of disease presentation, tumor size, tumour extent, histologic grade, lymph node status, size of the largest lymph node and hormone receptors ER, PR, HER2 neu with p53 expression were studied.
The categorical variables were expressed as percentages. Chi-squared test was used for categorical variables for calculating p-value (p-value <0.05 = significant). Statistical analysis was performed using SPSS version 21.
Results
A total of 86 cases of invasive breast carcinoma were studied, out of which most of the women belonged to the age group 41-60 years (54, 62.8%) followed by >60 years (19, 22.1%). The duration of symptoms in 36 (41.9%) cases was less than 6 months and in 50 (58.1%) cases was more than 6 months. Family history of breast carcinoma was present in 17 (19.8%) and absent in 69 (80.2%) of 86 cases Table 1.
| Clinical characteristics | N=86 | % | |
| Age group (years) | ≤ 40 | 13 | 15.1 |
| 41 – 60 | 54 | 62.8 | |
| > 60 | 19 | 22.1 | |
| Duration (months) | < 6 | 36 | 41.9 |
| > 6 | 50 | 58.1 | |
| Family history | Present | 17 | 19.8 |
| Absent | 69 | 80.2 | |
| Lymphatic invasion | Present | 54 | 62.8 |
| Absent | 32 | 37.2 | |
| Tumour size (cm) | < 2 | 5 | 5.8 |
| 2 – 5 | 57 | 66.3 | |
| >5 | 24 | 27.9 | |
| Largest lymph node | <2 | 58 | 67.4 |
| >2 | 28 | 32.6 | |
| SBR grade | Grade 1 | 9 | 10.5 |
| Grade 2 | 69 | 80.2 | |
| Grade 3 | 8 | 9.3 | |
| Tumour grading | Stage I | 1 | 1.2 |
| Stage II | 52 | 60.5 | |
| Stage III | 33 | 38.4 | |
| ER status | Positive | 49 | 57 |
| Negative | 37 | 43 | |
| PR status | Positive | 49 | 57 |
| Negative | 37 | 43 | |
| Her 2 neu status | Positive | 26 | 30.2 |
| Negative | 60 | 69.8 | |
| P53 status | Positive | 71 | 82.6 |
| Negative | 15 | 17.4 |
Out of 86 cases, 54 (62.8%) showed metastasis in the lymph nodes. The tumour size (largest dimension) ranged from 0.5 cm to 4 cm. Of 86 cases, 57 (66.3%) were in the range of 2 – 5 cm. The largest lymph node size was less than 2 cm in 58 (67.4%) cases. Scarff Bloom Richardson (SBR) score of 6 – 7 was seen in 69 (80.2%) cases and 52 (60.5%) were found to be in Stage II. Table 1.
ER was positive in 49 (57.0%) and negative in 37 (43.0%) cases, PR was positive in 49 (57.0%) and negative in 37 (43.0%) cases and HER2 neu showed positive expression in 26 (30.2%) and negative expression in 60 (69.8%) cases. P53 expression was positive in 71 (82.6%) and negative in 15 (17.4%) of a total of 86 cases as reflected I the Table 1.
Of the 86 patients ER/PR was positive in 49 patients (57 %), ER/PR was negative in 37 patients. ER/PR/Her2 neu was positive in 14 (16.3%) patients and ER/PR/Her2 neu negative in 25 (29.1%) patients. In 35 patients (40.7%) ER/PR was positive with negative HER2 neu and in 12 patients (14%) ER/PR was negative with positive HER2 neu as shown in the Table 2.
| Characteristics | N=86 | % | |
| ER AND PR | ER + / PR + | 49 | 57 |
| ER - / PR - | 37 | 43 | |
| ER, PR AND HER 2 neu | ER+/PR+/HER2 NEU+ | 14 | 16.3 |
| ER-/PR-/HER2 NEU- | 25 | 29.1 | |
| ER+/PR+/HER2 NEU- | 35 | 40.7 | |
| ER-/PR-/HER2 NEU+ | 12 | 14 |
Among all the Age groups, most of the patients had tumour size ranging from 2-5 (57, 66.28%) and most people belonged to the age group of 40 - 60 years (38, 70.37%) Table 3.
| Characteristics | Age Group (%) | Total (N=86) | P-value | |||
| ≤ 40 (N=13) | 40-60 (N=54) | > 60 (N=19) | ||||
| Tumour Size (cms) | < 2 | 2 (15.38) | 3 (5.56) | - | 5 (5.81) | 0.343 |
| 5-Feb | 7 (53.85) | 38 (70.37) | 12 (63.16) | 57 (66.28) | ||
| >5 | 4 (30.77) | 13 (24.07) | 7 (36.84) | 24 (27.91) | ||
| SBR Grade | Grade 1 | 2 (15.38) | 4 (7.41) | 3 (15.79) | 9 (10.47) | 0.364 |
| Grade 2 | 9 (69.23) | 47 (87.04) | 13 (68.42) | 69 (80.23) | ||
| Grade 3 | 2 (15.38) | 3 (5.56) | 3 (15.79) | 8 (9.3) | ||
| Lymphatic invasion | Present | 10 (76.92) | 34 (62.96) | 10 (52.63) | 54 (62.79) | 0.377 |
| Absent | 3 (23.08) | 20 (37.04) | 9 (47.37) | 32 (37.21) | ||
| Lymph node size (cms) | < 2 | 9 (69.23) | 35 (64.81) | 14 (73.68) | 58 (67.44) | 0.769 |
| > 2 | 4 (30.77) | 19 (35.19) | 5 (26.32) | 28 (32.56) | ||
| Tumour grading | Stage I | - | 1 (1.85) | - | 1 (1.16) | 0.881 |
| Stage II | 7 (53.85) | 34 (62.96) | 11 (57.89) | 52 (60.47) | ||
| Stage III | 6 (46.15) | 19 (35.19) | 8 (42.11) | 33 (38.37) | ||
| P53 | Positive | 12 (92.31) | 44 (81.48) | 15 (78.95) | 71 (82.56) | 0.585 |
| Negative | 1 (7.69) | 10 (18.52) | 4 (21.05) | 15 (17.44) | ||
| ER/PR | Positive | 7 (53.85) | 29 (53.7) | 13 (68.42) | 49 (56.98) | 0.521 |
| Negative | 6 (46.15) | 25 (46.3) | 6 (31.58) | 37 (43.02) | ||
| ER, PR and HER 2 neu | ER+/PR+/HER2 NEU+ | 2 (14.38) | 6 (42.85) | 6 (42.85) | 14 (16.28) | 0.524 |
| ER+/PR+/HER2 NEU- | 5 (38.46) | 23 (42.59) | 7 (36.84) | 35 (40.7) | ||
| ER-/PR-/HER2 NEU+ | 2 (15.38) | 9 (16.67) | 1 (5.26) | 12 (13.95) | ||
| ER-/PR-/HER2 NEU- | 4 (30.77) | 16 (29.63) | 5 (26.32) | 25 (29.07) |
Of all the age groups studied, most of them had SBR grading of Grade 2 (69, 80.23%) and most of the patients belonged to the age group 40 – 60 years (69, 80.23%).
Metastasis in lymph nodes was present in 54 patients (62.79%) and was most prevalent in the age group <40 years (69.23%) followed by 40 – 60 years (34, 62.96%). Lymph node size mostly observed was <2 in 58 (67.44%) patients with most of patients being in age <40 years (9, 69.23%). P53 was positive in 71 (82.56 %) patients and 12 patients (92.31%) of 13 in age group < 40 years. Table 3. Of the 14 triple positive cases, 6 (42.85%) cases each were seen in the age group of 40 – 60 and above 60 years respectively and 2 (14.3%) with age less than 40 years. Of the 25 triple negative cases, 16 (29.63%) were seen in the age group of 40 – 60 years, 5 (26.32%) with age more than 60 years and 4 (30.77%) with age less than 40 years as displayed in Table 3.
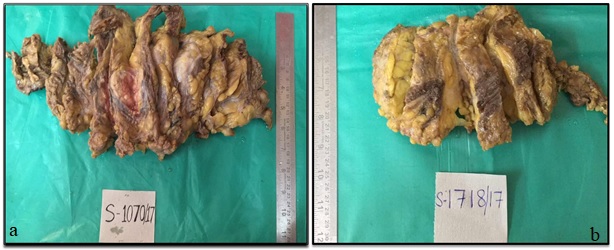
Of 49 cases with ER and PR positive in 36 (73.47%) have tumour in the size range of 2 – 5 cm followed by 11 (22.4%) cases had tumour with size more than 5 cm. Of 37 cases with ER and PR negative, 21 (56.76%) had tumour with size in the range of 2 – 5 cm followed by 13 (35.1%) cases with size more than 5 cm (Figure 1).
Figure 1. Gross Specimen of Modified Radical Mastectomy. a) Gross specimen of modified radical mastectomy showing a well circumscribed grey white ulceroinfiltrative tumour. b) Gross specimen of modified radical mastectomy showing a grey white infiltrative tumour.
Cases with ER and PR positive, 41 (83.67%) were in Grade 2 and 4 (8.16%) were in Grade 1 and Grade 3 each, respectively. Table 4.
| Characteristics | ER/PR (%) | Total (N=86) | P-value | ||
| Positive (N=49) | Negative (N=37) | ||||
| Tumour size | < 2 | 2 (4.08) | 3 (8.11) | 5 (5.81) | 0.26 |
| 05-Feb | 36 (73.47) | 21 (56.76) | 57 (66.28) | ||
| >5 | 11 (22.45) | 13 (35.14) | 24 (27.91) | ||
| SBR Grade | Grade 1 | 4 (8.16) | 5 (13.51) | 9 (10.47) | 0.636 |
| Grade 2 | 41 (83.67) | 28 (75.68) | 69 (80.23) | ||
| Grade 3 | 4 (8.16) | 4 (8.16%) | 8 (9.3) | ||
| Lymphatic invasion | Present | 32 (65.31) | 22 (59.46) | 54 (62.79) | 0.579 |
| Absent | 17 (34.69) | 15 (40.54) | 32 (37.21) | ||
| Lymph node size (cms) | < 2 | 35 (71.43) | 23 (62.16) | 58 (67.44) | 0.364 |
| > 2 | 14 (28.57) | 14 (37.84) | 28 (32.56) | ||
| Tumour grading | Stage I | - | 1 (2.7) | 1 (1.16) | 0.465 |
| Stage II | 29 (59.18) | 23 (62.16) | 52 (60.47) | ||
| Stage III | 20 (40.82) | 13 (35.14) | 33 (38.37) | ||
| P53 | Positive | 37 (75.51) | 34 (91.89) | 71 (82.56) | 0.047* |
| Negative | 12 (24.49) | 3 (8.11) | 15 (17.44) |
Note, *; **; *** refer to <0.05, <0.01 and <0.001 level of significance
Of 49 cases with ER and PR positive, metastasis to lymph nodes was present in 32 (65.31%) and absent in 17 (34.7%) patients. P53 expression was positive in 37 (75.5%) cases and negative in 12 (24.5%) cases and it was significant (P- 0.047). Of 37 cases with ER/PR negative, p53 expression was positive in 34 (91.9%) cases and negative in 3 (8.1%) cases Table 4.
Of 14 triple positive cases, 11 (78.6%) had tumour with size in the range of 2 – 5 cm and 3 (21.4%) have tumour with size more than 5 cm. Of 25 triple negative cases, 15 (60.0%) had tumour with size in the range of 2 – 5 cm and 10 (40.0%) had tumour size more than 5 cm. Tumour size was significant with triple positive cases. (P 0.046). Of the 14 triple positive cases, 12 (85.7%) were in SBR Grade 2 and 2 (14.3%) in SBR Grade 1. Of the 25 triple negative cases, 17 (68.0 %) were in SBR Grade 2 and 16.0% are in SBR Grade 1 and 3 each. Of the 14 triple positive cases, metastasis to lymph nodes was present in 3 (21.4%) and absent in 11 (78.57%). Of the 25 triple negative cases, metastasis to lymph nodes was present in 12 (48.0%) and absent in 13 (52.0%). (P value 0.000) as shown in Table 5.
| Characteristics | ER, PR AND HER 2 neu (%) | Total (N=86) (%) | P-value | ||||
| ER+/PR+/HER2 NEU+ (N=14) | ER+/PR+/HER2 NEU- (N=35) | ER-/PR-/HER2 NEU+ (N=12) | ER-/PR-/HER2 NEU- (N=25) | ||||
| Tumour size (cms) | < 2 | - | 2 (5.71) | 3 (25) | - | 5 (5.81) | 0.046* |
| 05-Feb | 11 (78.57) | 25 (71.43) | 6 (50) | 15 (60) | 57 (66.28) | ||
| >5 | 3 (21.43) | 8 (22.86) | 3 (25) | 10 (40) | 24 (27.91) | ||
| SBR Grade | Grade 1 | 2 (14.29) | 2 (5.71) | 1 (8.33) | 4 (16) | 9 (10.47) | 0.393 |
| Grade 2 | 12 (85.71) | 29 (82.86) | 11 (91.67) | 17 (68) | 69 (80.23) | ||
| Grade 3 | - | 4 (11.43) | - | 4 (16) | 8 (9.3) | ||
| Lymphatic invasion | Present | 3 (21.43) | 29 (82.86) | 10 (83.33) | 12 (48) | 54 (62.79) | 0.000*** |
| Absent | 11 (78.57) | 6 (17.14) | 2 (16.67) | 13 (52) | 32 (37.21) | ||
| Lymph node size (cms) | < 2 | 12 (85.71) | 23 (65.71) | 8 (66.67) | 15 (60) | 58 (67.44) | 0.422 |
| > 2 | 2 (14.29) | 12 (34.29) | 4 (33.33) | 10 (40) | 28 (32.56) | ||
| Tumour grading | Stage I | - | - | 1 (8.33) | - | 1 (1.16) | 0.067 |
| Stage II | 11 (78.57) | 18 (51.43) | 5 (41.67) | 18 (72) | 52 (60.47) | ||
| Stage III | 3 (21.43) | 17 (48.57) | 6 (50) | 7 (28) | 33 (38.37) | ||
| P53 | Positive | 13 (92.86) | 24 (68.57) | 11 (91.67) | 23 (92) | 71 (82.56) | 0.045* |
| Negative | 1 (7.14) | 11 (31.43) | 1 (8.33) | 2 (8) | 15 (17.44) |
Note, *; **; *** refer to <0.05, <0.01 and <0.001 level of significance
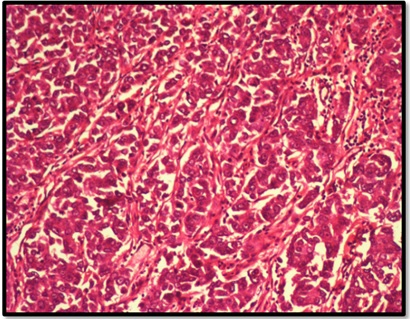
Of the 14 triple positive cases, p53 expression was positive in 13(92.9%) and negative in 1 (7.1%). Of the 25 triple negative cases, p53 expression was positive in 23 (92.0%) and negative in 2 (8.0%). (P value 0.045) Table 5. Of the 71 p53 positive cases, 44 (62.0%) were in the age group of 40 – 60 years, 15 (21.1%) patients were more than 60 years and 12 (16.9%) were 40 years. Duration of symptoms was more than 6 months in 41 (57.7%) cases and less than 6 months in 30 (42.25%). The size of the largest lymph node was less than 2 cm in 49 (69.0%) and more than 2 cm in 22 (31.0%) patients. Metastasis to lymph nodes was present in 44 (62.0%) and absent in 27 (38.0%). Tumour grading was classified as stage 2 in 42 (59.2%) cases, stage 3 in 28 (39.4%) cases. SBR Grade 2 was seen in 58 (81.69%), SBR Grade 1 in 9 (12.7%) and 4 (5.6%) cases were in SBR Grade 3 (P value- 0.019) (Figure 2).
Figure 2. Infiltrating Ductal Carcinoma. Infiltrating ductal carcinoma. Haematoxylin & eosin. (20x).
In 26 (30.8%) positive cases, HER 2 neu overexpression was seen in 24 (33.8%) patients Table 6.
| Characteristics | P53 (%) | Total (N=86) | P-value | ||
| Positive (N=71) | Negative (N=15) | ||||
| Age Group (years) | < 40 | 12 (16.9) | 1 (6.67) | 13 (15.12) | 0.585 |
| 40-60 | 44 (61.97) | 10 (66.67) | 54 (62.79) | ||
| > 60 | 15 (21.13) | 4 (26.67) | 19 (22.09) | ||
| Duration (months) | < 6 | 30 (42.25) | 6 (40) | 36 (41.86) | 0.872 |
| > 6 | 41 (57.75) | 9 (60) | 50 (58.14) | ||
| Tumour size (cms) | < 2 | 5 (7.04) | - | 5 (5.81) | 0.167 |
| 05-Feb | 44 (61.97) | 13 (86.67) | 57 (66.28) | ||
| >5 | 22 (30.99) | 2 (13.33) | 24 (27.91) | ||
| Lymph node size (cms) | < 2 | 49 (69.01) | 9 (60) | 58 (67.44) | 0.498 |
| > 2 | 22 (30.99) | 6 (40) | 28 (32.56) | ||
| Lymphatic invasion | Present | 44 (61.97) | 10 (66.67) | 54 (62.79) | 0.733 |
| Absent | 27 (38.03) | 5 (33.33) | 32 (37.21) | ||
| Tumour Grading | Stage I | 1 (1.41) | - | 1 (1.16) | 0.8 |
| Stage II | 42 (59.15) | 10 (66.67) | 52 (60.47) | ||
| Stage III | 28 (39.44) | 5 (33.33) | 33 (38.37) | ||
| SBR Grade | Grade 1 | 9 (12.68) | - | 9 (10.47) | 0.019* |
| Grade 2 | 58 (81.69) | 11 (73.33) | 69 (80.23) | ||
| Grade 3 | 4 (5.63) | 4 (26.67) | 8 (9.3) | ||
| HER2 NEU | Positive | 24 (33.8) | 2 (13.33) | 26 (30.23) | 0.117 |
| Negative | 47 (66.2) | 13 (86.67) | 60 (69.77) |
Note, *; **; *** refer to <0.05, <0.01 and <0.001 level of significance
Of the 15 p53 negative cases, most of them 10 (66.7%) were in the age group of 40 – 60 years. Duration of symptoms was more than 6 months in 9 (60.0%) and less than 6 months in 6 (40.0%). Tumour size ranged from 2 – 5 cm in 13 (86.7%). The size of the largest lymph node was less than 2 cm in 9 (60.0%) and more than 2 cm in 6 (40.0%). Metastasis to lymph nodes was present in 10 (66.7%) and absent in 5 (33.3%), 10 (66.7%) were in stage 2 and 5 (33.3%) in stage 3. SBR grading in 11 (73.3%) was SBR Grade 2 and 4 (26.7%) were in SBR Grade 3 (P value- 0.019). HER 2 neu overexpression was seen in 2 (13.3%) as presented in Table 6.
Discussion
There is evidence that the incidence of breast cancer in India is on the rise. Several risk factors for the development of breast carcinoma have been established. The common denominator for most of the factors is prolonged estrogen stimulation operating on a genetically susceptible background [7].
In our study the age of the patients ranged from 34 to 82 years with a mean age of 59 years. The maximum cases are in the range of 40 to 60 years (62.8%). In various other studies, similar results as our study were obtained. In the study by Ayadi et al 51.6% of cases occurred in less than 50 years of age with median age of 51 years and 46% of cases occurred in less than 45 years [8]. In the study by Raina et al 49.7% of cases occurred in less than 45 years and 48.5% cases in greater than 45 years [9].
Majority of the cases (66.3%) had tumour with size 2- 5 cm followed by 27.9% cases with tumour measuring > 5 cm in largest dimension. None of the patients had received any chemo, radio or hormonal therapy. This study results were similar to study by Patnayak et al [7] where tumour size 2-5 cm was seen in most of cases (160, 79.6%) and least cases had < 2cm (19, 19.4%) [7].
Of 86 cases, 54 cases (62.8%) showed metastatic disease with the largest lymph node measuring < 2 cm in 67.4% cases similar to studies by Payandeh et al in which 64% had lymph node metastasis [10].
Of the 86 cases in our study, maximum cases (80.2%) were in SBR Grade 2, that is, they have an SBR score of 6 – 7. Similarly a study by Reddy SR et al showed 81.61% were in the SBR Grade II [11].
In our study we noted an overall 57.0% of ER positivity and 57.0% of PR positivity (Figure 3a and 3c).
Figure 3. Immunohistochemical Staining of Estrogen and Progesterone Receptor. a) Immunohistochemical staining- estrogen receptor (er) -positive expression. (10x). b) Immunohistochemical staining- estrogen receptor (er) –negative expression. (10x). c) Immunohistochemical staining- progesterone receptor (pr) -positive expression. (10x). d) Immunohistochemical staining- progesterone receptor (pr) -negative expression. (10x).
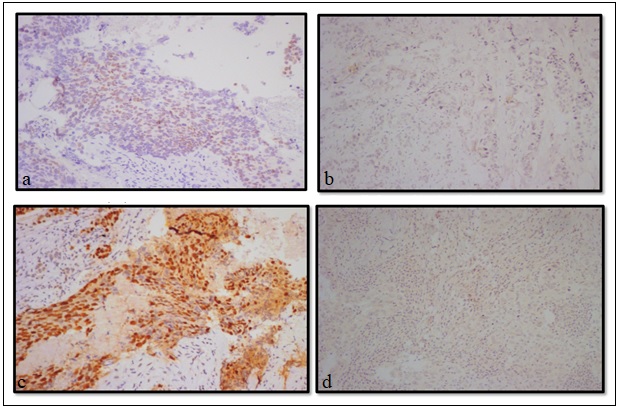
The prevalence of hormone receptor positive breast carcinoma in Asian countries has been found to be lower as compared to Western world. Western studies have reported 70 – 80% ER and 60 – 70% PR expression in cases of invasive ductal carcinoma, respectively [12]. The other study from India has documented lower positivity for the hormone receptors similar to our study. In a study by Dutta et al ER/PR overexpression was found in 33.5% [13].
The percentage of tumours expressing both ER and PR include 57.0%, of which maximum (59.2%) are seen in the age group of 40 – 60 years, with a tumour size of 2 – 5 cm in 73.5% and 65.3% showing lymphatic invasion. In this study there was a correlation between metastasis and ER, PR and Her 2 neu (p 0.000). The above results correlated with the study results by Siadati S et al where there was a significant correlation between lymphatic invasion and ER, PR and Her 2 neu expression (p<0.05) [14]. There was also a significant correlation between ER, PR receptors and p53 over-expression. In 91.9% of cases with both ER and PR positivity showed p53 over-expression similar to the study by Bae SY et al (90%) [15].
Triple negative breast cancers (TNBC) have recently attracted a lot of attention, because of their poor prognosis. TNBCs are frequently shown to harbour mutations in Tp53, resulting in loss of the G1 checkpoint and reliance on checkpoint kinase-1 to arrest cell in response to DNA damage. In our study, triple negative cases constituted 29.1% of the total cases, of which 64.0% are in the age group of 40 – 60 years, with a tumour size of 2 – 5 cm in 60% and 48% showing lymphatic invasion which was similar to study by Rana MJ et al where the mean age of TNBC patients was 53.3+11.6 years with 90% showing invasion [16].
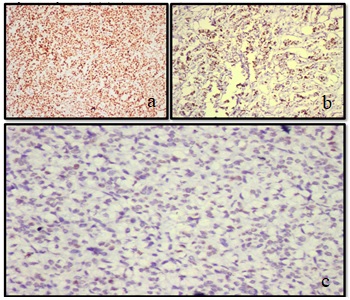
A significant correlation is noted between triple negative cases and p53 over-expression in our study (Figure 4a, b, c).
Figure 4. Immunohistochemical Staining of P53 Over expression. a) Immunohistochemical staining-p53 overexpression (3+). (10x). b) Immunohistochemical staining-p53 overexpression (2+). (10x). C) Immunohistochemical staining-p53 negative expression. (10x).
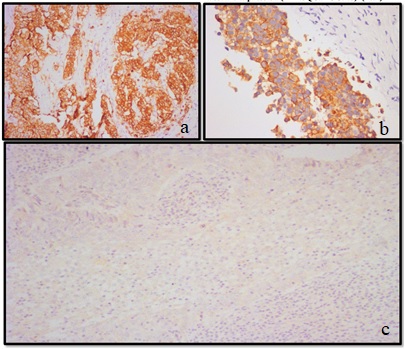
In 92.0% cases of triple negative show p53 over-expression. A study by Hashmi AA et al also showed correlation between triple negative cases and P 53 expression 49% of cases [17].
Since its initial discovery, HER 2 neu was used as a therapeutic target because of the efficacy of trastuzumab, a recombinant humanized monoclonal antibody that binds with high affinity to HER 2 in advanced breast cancer. Over-expression of HER 2 occurs through either amplification of the gene or mRNA over-expression. HER 2 neu over-expression is seen in 30.2% cases in this study (Figure 5a and Figure 5b) which is similar to that noted by Ambroise et.al. (27.1%) and Patnayak R et.al. (29.6%) [7][18].
Figure 5. Immunohistochemical Staining of Human Epidermal Receptor 2. a) Immunohistochemical staining- Human epidermal receptor 2 (HER 2 neu)- (3+). (10x) Positive expression. b) Immunohistochemical staining- Human epidermal receptor 2 (HER 2 neu)- Positive expression (2+-EQUIVOCAL).(20x). c) Immunohistochemical staining- Human epidermal receptor 2 (HER 2 neu)- Negaive expression (1+). (10x).
One study from north India had shown HER 2 neu oncogene over-expression is higher (46.37%) among Indian patients in comparison to 25 – 30% in most western literature [19,20].
However various studies show considerable variation regarding the frequency of HER 2 positivity. There is also evidence from the literature that coexistence of over- expression of HER 2 neu and p53 protein accumulation is a strong prognostic marker in breast cancer [21,22]. However, in our study we did not find a significant correlation between p53 and HER 2 neu over-expression. In our study the relation of p53 with age, duration of symptoms, tumour size, and lymphatic invasion was not found statistically significant. However, we found significant correlation of p53 over-expression with SBR tumour grade 2 (P-0.019). This finding is similar to that found in study by Deb P et al, where there statistical significance was found between P53 and SBR grade II (P<0.05) [23].
In conclusion, significant positive correlation between p53 over expression and tumour grade was seen in this study. Nodal involvement may be an indicator of metastatic disease, the cause of death in patients with breast cancer. Hence the generally admitted conclusion is that tumour size loses its prognostic role in cases of nodal involvement.
Significant positive correlation of p53 over expression with ER and PR positive tumours and Triple Negative tumours was noted.
Despite improving breast cancer outcomes, distant recurrence remains common and incurable. This study demonstrates the expression of p53 in invasive ductal carcinomas and its correlation with hormone receptors, HER 2 neu and clinico-pathological parameters, thus contributing to an expanding knowledge of prognostic and predictive markers that will allow individualized therapy for invasive breast carcinoma.
To conclude, we suggest that p53 accumulation detected immunohistochemically defines a subgroup of breast carcinoma patients with high tumour aggressiveness and adverse long term prognosis.
References
- Ki67 and P53 expression in breast cancer and their correlation with clinicopathological parameters Gogoi* S, Das B, Borgohain M, Gogoi G, Das J. Indian Journal of Pathology and Oncology.2021;8(4). CrossRef
- Breast cancer in India: Present scenario and the challenges ahead Mehrotra R, Yadav K. World Journal of Clinical Oncology.2022;13(3). CrossRef
- Triple-negative breast cancer molecular subtyping and treatment progress Yin L, Duan J, Bian X, Yu S. Breast cancer research: BCR.2020;22(1). CrossRef
- BD_Chaurasia’s_Human_Anatomy, Volume 1 - Upper Limb Thorax, 6th Edition .
- Diversity of Breast Carcinoma: Histological Subtypes and Clinical Relevance Makki J. Clinical Medicine Insights. Pathology.2015;8. CrossRef
- Correlation of the expression of estrogen receptor, progesterone receptor and HER2/neu with the clinical features and the tumour histopathology in patients of breast carcinoma at mahavir cancer sansthan Lata KB, Nirala SK. Int j res med sci.2021;9:2401-2408.
- Hormone receptor status (estrogen receptor, progesterone receptor), human epidermal growth factor-2 and p53 in South Indian breast cancer patients: A tertiary care center experience Patnayak R, Jena A, Rukmangadha N, Chowhan AK , Sambasivaiah K, Phaneendra BV , Reddy MK . Indian Journal of Medical and Paediatric Oncology: Official Journal of Indian Society of Medical & Paediatric Oncology.2015;36(2). CrossRef
- Correlation of HER-2 over-expression with clinico-pathological parameters in Tunisian breast carcinoma Ayadi L, Khabir A, Amouri H, Karray S, Dammak A, Guermazi M, Boudawara T. World Journal of Surgical Oncology.2008;6. CrossRef
- Clinical features and prognostic factors of early breast cancer at a major cancer center in North India Raina V, Bhutani M, Bedi R, Sharma A, Deo SV , Shukla NK , Mohanti BK , Rath GK . Indian Journal of Cancer.2005;42(1). CrossRef
- Expression of p53 Breast Cancer in Kurdish Women in the West of Iran: a Reverse Correlation with Lymph Node Metastasis Payandeh M, Sadeghi M, Sadeghi E, Madani S. Asian Pacific journal of cancer prevention: APJCP.2016;17(3).
- Histopathological Prognostic Factors In Carcinoma Breast - An Indian Institutional Experience Reddy SR , Chaitanya B, Latha PS . International Journal of Medical Research and Review.2014;2(6). CrossRef
- Correlation of hormonal receptor and her-2/neu expression in breast cancer: a study at tertiary care hospital in south Gujarat Vasudha B, Bharti J, Prashant P. National journal of medical research.2012;2:295-298.
- Hormone Receptors, Her-2/Neu and Chromosomal Aberrations in Breast Cancer Dutta V., Chopra G. S., Sahai K., Nema S. K.. Medical Journal, Armed Forces India.2008;64(1). CrossRef
- Correlation of ER, PR and HER-2/Neu with other Prognostic Factors in Infiltrating Ductal Carcinoma of Breast Siadati S, Sharbatdaran M, Nikbakhsh N, Ghaemian N. Iranian Journal of Pathology.2015;10(3).
- Poor prognosis of single hormone receptor- positive breast cancer: similar outcome as triple-negative breast cancer Bae SY , Kim S, Lee JH , Lee H, Lee SK , Kil WH , Kim SW , Lee JE , Nam SJ . BMC Cancer.2015;15(1). CrossRef
- Expression of p53 and p16 in Carcinoma Breast Tissue: Depicts Prognostic Significance or Coincidence Rana MK , Rana APS , Khera U. Cureus.2021;13(11). CrossRef
- Prognostic significance of p16 & p53 immunohistochemical expression in triple negative breast cancer Hashmi AA , Naz S, Hashmi SK , Hussain ZF , Irfan M, Khan EY , Faridi N, Khan A, Edhi MM . BMC clinical pathology.2018;18. CrossRef
- Immunohistochemical profile of breast cancer patients at a tertiary care hospital in South India Ambroise M, Ghosh M, Mallikarjuna VS , Kurian A. Asian Pacific journal of cancer prevention: APJCP.2011;12(3).
- Human epidermal growth factor receptor 2/neu and the clinic pathological profile in breast cancer: an observational study at a tertiary care hospital in Central India Shukla S, Ansari F. Int surg J.2021;8:3649-3653.
- Significance of Her-2/neu protein over expression in Indian breast cancer patients Kumar V, Tewari M, Singh U, Shukla HS . The Indian Journal of Surgery.2007;69(4). CrossRef
- Evaluation of immunohistochemistry and enzyme linked immunosorbent assay for HER-2/neu expression in breast carcinoma James R, Thriveni K., Ramaswamy G, Krishnamoorthy L, Mukherjee G, Vijayalaxmi Deshmane PP , Bapsy PP . Indian journal of clinical biochemistry: IJCB.2008;23(4). CrossRef
- PRIMA-1 inhibits growth of breast cancer cells by re-activating mutant p53 protein Liang Y, Besch-Williford C, Hyder SM . International Journal of Oncology.2009;35(5). CrossRef
- Correlationship of Hormone Receptor Status, P53 Mutation and C-Erb B-2 Overexpression with Nuclear Grading in Breast Cancers Deb P, Deshpande GU , Rai R. Medical Journal, Armed Forces India.2000;56(4). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2022
Author Details