Prostate Cancer: Germline Mutations in BRCA1 and BRCA2
Download
Abstract
Genetic alterations are one of the important known risk factors of Prostate cancer. The family predisposition of breast and ovarian cancers may cause the lethal progression of familial prostate cancer in some men. The Association of germline mutations in BRCA1 and BRCA2 genes can cause breast cancer in almost 35% of women and 9% of men. Carriers of these pathogenic variants have a higher risk of causing prostate cancer. This study focused on the analysis of mutations causing prostate cancer around the world, associated with breast cancer susceptibility genes.
Introduction
Prostate cancer is the 2nd most recurrently diagnosed cancer in men, and also the 5th leading cause of death worldwide [1]. In Prostate cancer, symptoms are not observed in the early onset of the disease. Incidence rates differ worldwide with the usage of different diagnostic tests. Prostate cancer frequency and death rates are strongly associated with age with the higher incidence being found in men over the age of 65 [1]. The early-stage prostate cancers are mostly latent and only 25% of cancers are known to be life-threatening [2]. Prostate-specific antigens (PSA), a glycoprotein expressed in Prostate cancer, based on elevated plasmatic level of PSA shows the occurrence of prostate cancer. In some conditions, men show elevated PSA levels without cancer. So, tissue biopsy has made the standard diagnostic test to confirm the presence of malignancy [3]. To grade the prognosis of prostate cancer Gleason score is used, which gives the potential rate of recurrence and mortality [4]. Prostate cancer can be treated in its early stages, so there will be no further development of metastases in patients. Once cancer reaches the metastatic stage, the survival chances are very less with aggressive cancer [5].
Risk factors
The major possible risk factors for Prostate cancer are first mentioned as age, lifestyle, food, ethnicity and molecular changes (genetic alterations), which have shown massive connections with hereditary cancer progressions [6]. Prostate cancer is a heterogeneous disease with a multiphase development process [6]. African-American men develop aggressive kinds of prostate cancer and the incidence rate is also higher when compared with white men. Diet plays an optimistic risk associated with prostate cancer. Consuming a higher amount of red meat, and saturated animal fat and lower consumption of fruits and veggies, vitamins, minerals and coffee [7].
Using GLOBOCAN 2020 estimation, we have collected the incidence and mortality rates of the prostate cancer population across the world. The following pie charts show the number of new cases registered (Figure 1), and the number of deaths recorded (Figure 2) in 2020 due to prostate cancer irrespective of men of all ages. The numbers are given according to the continents.
Figure 1. The Number of New Prostate Cancer Cases Recorded in 2020, with Respect to the Seven Continents.
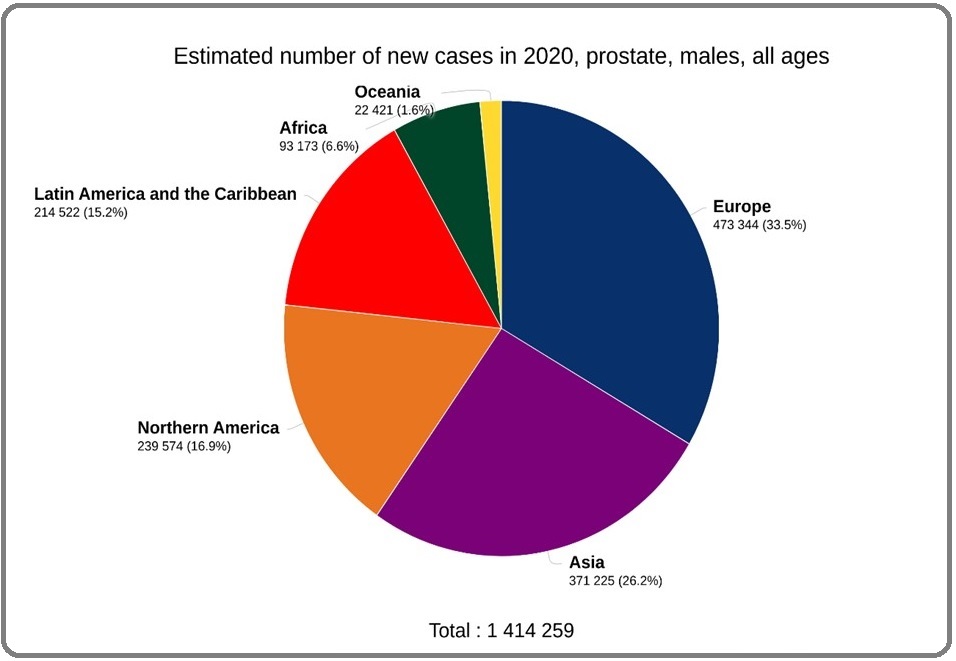
Figure 2. The Number of Deaths Recorded due to Prostate Cancer in 2020, with Respect to the Seven Continents.
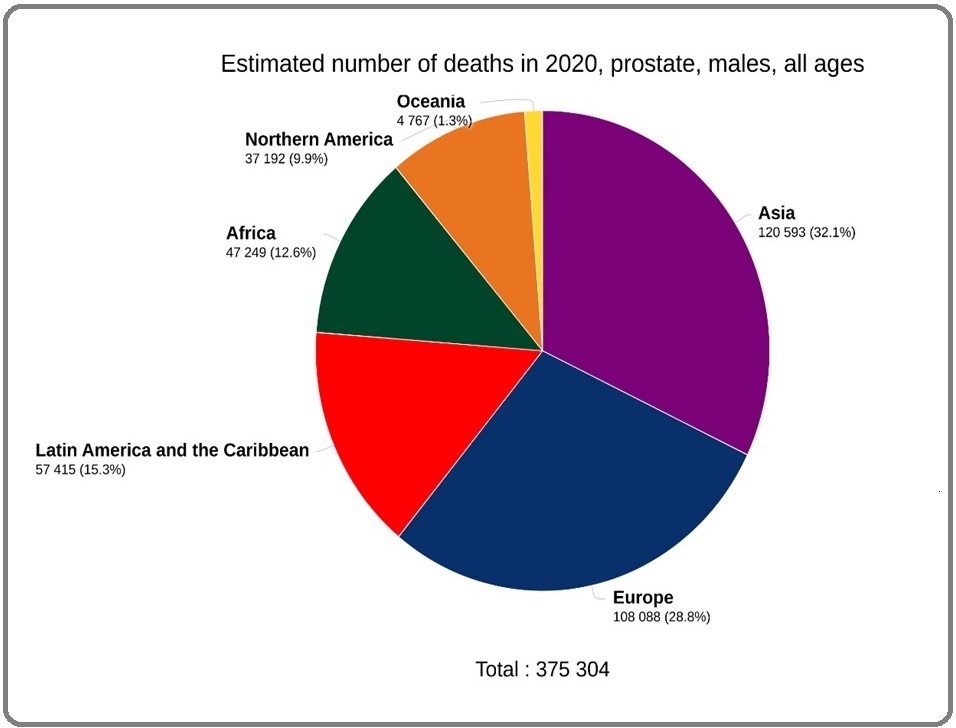
Total 14,14,259 new cases are recorded, where 4,73,344 (33.5%) are from Europe, followed by 3,71,225 (26.2%) are from Asia, 2,39,574 (16.9%) from North America, 2,14,522 (15.2%) are from Latin America and the Caribbean, 93,173 (6.6%) are from Africa, and lastly 22,421 (1.6%) are from Oceania (Figure 1) [8]. Figure 2, shows that 3,75,304 prostate cancer deaths have been recorded in 2020, in which 1,20,593 (32.1%) are from Asia, 1,08,088 (28.8%) are from Europe, 57,415 (15.3%) are from Latin America and the Caribbean, followed by 47,249 (12.6%) from Africa, 37,192 (9.9%) are from North America, and lastly 4,767 (1.3%) are from Oceania [8].
Relationship between Breast, Ovarian and Prostate Cancer
Many studies have observed the genetic epidemiology of familial association between Breast, Ovarian and Prostate cancer. Gene alteration in BRCA (breast cancer susceptibility gene) is responsible for the familial clustering of these cancers. Around the world, Breast cancer is known to be the leading most common carcinoma causing women. Nearly thirty lakhs breast cancer cases have been diagnosed in 2018 and over six lakhs deaths were recorded worldwide. Ovarian cancer is less common and shows a higher rate of mortality. Around three lakhs cases were diagnosed in the same year and almost two lakhs deaths were recorded [9]. Prostate cancer is counted in the list of heritable cancers, showing higher chances of risks with familial breast cancer and familial prostate cancer. Studies have shown the risk for men with a history of breast or prostate cancer in their family has a higher rate of getting aggressive prostate cancer [10]. BRCA1 and BRCA2 are the known confer genes to date that risk about 8.6 folds in men less than 65 years [11]. Familial cancer aggression is more affected in people of younger age, with more than 3 affected generations. In first-degree relatives, the risk is twice as compared with the normal cases [12]. Being tumour suppressor genes BRCA1 and BRCA2 both the gene follow autosomal dominant inheritance pattern [14]. Both genes encode large protein factors which help in many cellular pathways. BRCA1 plays a key role in cellular functions like control system, processing, DNA damage and repair, chromatin remodelling and transcriptional regulation [15]. BRCA2 mainly participate in regulating the activity of RAD15, and also manages DNA recombination and repairing process [16]. Loss of function in these genes can structurally and functionally alter the stability at the genomic and chromosomal level [17]. Table 1 shows, about 50-65% of BRCA1 mutations can cause breast cancer and ovarian in females and 1.2% lead to male breast cancer.
| Cancer site | BRCA1 (%) | BRCA2 (%) |
| Breast | 50 - 65 | 40-55 |
| Pancreas | 1-3 | 2-7 |
| Ovarian | 40-65 | 15-25 |
| Prostate | 9 | 15 |
Also, 1-3% can risk pancreas cancer, and 9% can risk prostate cancer. Similarly, 40-55% of BRCA2 mutations can lead to breast cancer, and up to 9% can cause male breast cancer. 2-7% of mutations can lead to pancreas cancer, 15-25% of mutations risk ovarian cancer and 15% of mutations lead to prostate cancer.
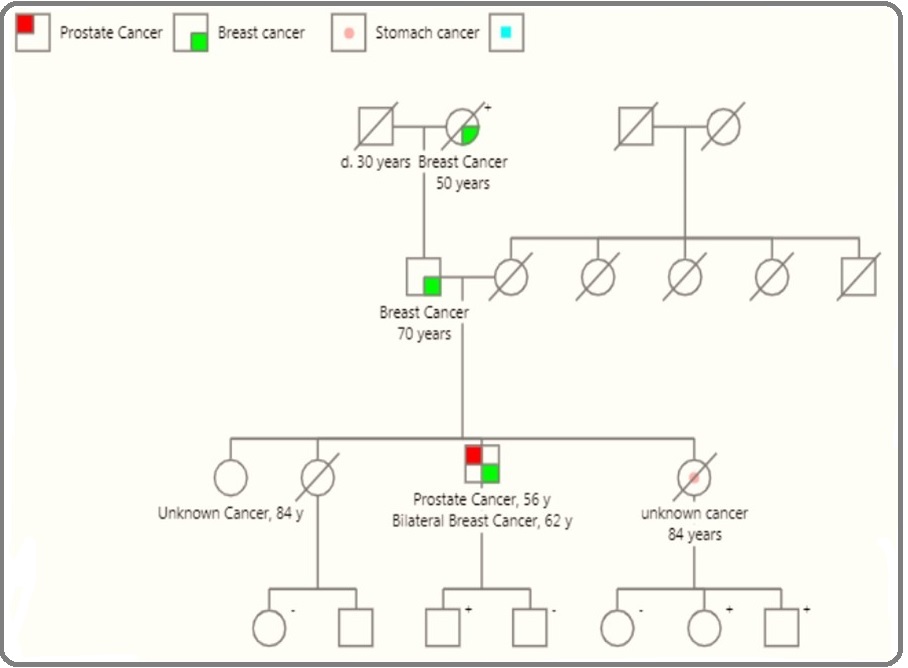
The pedigree chart (Figure 3) shows the germline mutation in the BRCA2 gene running in this family causing breast cancer in 50-year-old women, then the hereditary gene flows causing breast cancer in males of age 72 (offspring) in the first generation. In the second generation, one of the offspring showed the germline mutation of BRCA2 and was diagnosed with positive prostate cancer and also bilateral breast cancer at the age of 56 and 62 years respectively [18].
Figure 3. Pedigree of germline mutation in BRCA2 flowing through this family causes hereditary breast and prostate cancer [18].
Most of the studies have shown the association of BRCA2 mutation for prostate cancer risk is stronger compared with the BRCA1 mutation. In a case-control study conducted by Ilir Agalliu et. al. In 2009, including a total of 979 prostate cancer and 1251 control cases of Jewish men. The results were observed with a three-fold increased risk for BRCA2 mutations with the higher Gleason score and also the first-degree family interactions can lead to stronger relationships. In the case of the BRCA1 mutation, there was a poor link but the deletions were associated with the elevated Gleason score risking the tumour [19]. Lauren Brady et.al. Conducted a study in 2022, where they found that germline mutation in some groups of genes penetrates the aggressive form of prostate cancer. The study included a total of 148 mutations where 32 were pathogenic. In that, they identified two mutations with BRCA1 and three with BRCA2 genes. And also, each mutation in BAP1 and BRRIP1 which are BRCA1- associated proteins [17].
We have reviewed the population study on Prostate cancer BRCA1 and BRCA2 mutation from the past 10 years and selected around 14 studies which conducted the mutational analysis of the candidate genes (Table 2).
| BRCA1 | BRCA2 | |||||||||
| Study | Year | Race | Samples | Mutation Detected | RR 95% CI Value | P- Val- ue | Samples | Mutation Detected | RR 95% CI Value | P Value |
| Elena Castro et.al. [20] | 2013 | UK | Cases: 2019 Control: 1940 | 18 | 0.021 | Cases: 2019 Control: 1940 | 61 | 0.001 | ||
| Elizabeth K. Bancroft et.al [21] | 2014 | UK | case: 376 | 2.35 (1.43-3.88) | case: 447 | 4.45 (2.99-6.61) | ||||
| Qing Zhu et.al. [22] | 2015 | China | Cases: 107 | 30 | 3.9 (1.4–8.5) | < 0.001 | Cases: 107 | 5 | 18.6 (13.2 - 25.3) | < 0.05 |
| C.C. Pritchard et.al. [23] | 2016 | US and UK | Cases: 692 | 6 | 3.9 (1.4–8.5) | 0.005 | Cases: 692 | 37 | 18.6 (13.2–25.3) | <0.001 |
| Matti Annala et.al. [24] | 2017 | USA | Cases: 319 | 1 | Cases: 319 | 16 | ||||
| P. I. Velho et.al. [25] | 2017 | Maryland | Cases: 150 | 2 | Cases: 150 | 9 | ||||
| Piper Nicolosi et.al. [26] | 2019 | African Americans | Cases: 3459 | 38 | Cases: 3436 | 75 | ||||
| Yukihide Momozawa et.al [31] | 2019 | Japanease population | Cases: 7636 | 14 | 2.27 (0.9 - 5.71) | 0.06 | Cases: 7636 | 83 | 5.65 (3.55 - 9.32) | <.001 |
| Yishuo Wua et.al. [27] | 2019 | Chainease population | Cases: 1694 | 3 | 2.80 (0.15–165.43) | 0.57 | Cases: 1694 | 20 | 12.88 (3.07–114.95) | 8.99E- |
| Burcu F. Darst et.al. [32] | 2020 | European- anscesty | Cases: 2770 Control: 2775 | 15 | 2.11 (0.37 -12.21) | 0.8 | Cases: 2770 Control: 2775 | 59 | 2.88 (1.22 - 6.83) | 6 |
| D. Wokołorczyk et.al. [33] | 2020 | European population | Cases: 390 Control: 308 | 2 | 0.5-34.3 | 0.2 | Cases: 390 Control: 308 | 4 | 0.4-134 | 0.02 |
| Tommy Nyberg et.al. [34] | 2020 | European population | Case:791 Control: 531 | 8 10 | Case: 731 Control: 428 | 247 | 0.1 | |||
| N. Segal et.al. [29] | 2020 | Isrel | Cases: 108 | 23 | 0.43 | Cases: 80 | 22 | |||
| Alyssa L. Smith et.al. [30] | 2022 | French Canadian Jewish | Cases:150 Cases:236 | 0 1 | 0 (0 - 3.4) 3.3 (0 - 18.1) | Cases:150 Cases:236 | 62 | 4.0 (1.7 - 8.6) 6.7 (0.8 - 22.4) | 0.43 |
Firstly, Elena Castro et. al. in the year 2013 studied the outcome of 2019 prostate cancer patient’s association with the status of BRCA1/2 genes and also the survival rates of the patients having the positive gene mutation. He used the Kaplan-Meier method to analyze the results and confirms the mutation results in more aggressiveness of the disease and have a poor rate of survival chances from metastasis [20,21]. In 2015 Qing Zhu et. al. conducted a study on the autoimmune response of BRCA1/2 in cancer and in a total of 107 tested patients of prostate cancer he found around 35 positive responses for the genes in which two patients show combine gene mutations [22]. In the year 2017 Matti Annala et. al. explained the outcome of heterozygosity tumour loss DNA repair deficient germline prostate cancer. He sequenced around 22 repair genes in 319 patients where he found 16 BRCA2 and one BRCA1 germline mutation [23,24]. In recurrence or developmental PCa germline mutations are very common among DNA repair genes in 2018 Pedro Isaacsson Velho et. al. worked on the association of this gene mutation in patients by germline testing. Around 150 samples were tested of which 43% have shown the germline mutation among which BRCA2 was found highest showing 14% results and similarly 9% of BRCA1 mutations were observed [25]. In the year 2019 Piper Nicolosi et. al. studied prostate cancer its prevalence for germline variants. In testing of 3459, 38 were positive for the BRCA1 mutation and 75 were positive for the BRCA2 germline mutation [26]. In the same year, two studies were conducted by Yukhihide M. et. al. and Yishuo Wu et. al. who worked on prostate cancer patients where the studies showed higher mutational rates in the BRCA2 gene than the BRCA1 gene. The studies included 7636 patients (of which 83 were showing BRCA2 mutation and 14 were showing BRCA1 mutations) and 1694 patients in which (20 responded positively for BRCA2 and 3 for BRCA1) respectively [27,28]. In the year 2020 N. Segal et. al. conducted a study where a total of 188 BRCA mutation (108 BRCA1, 80 BRCA2) carriers are screened for Prostate cancer. In 108 patients 23 were positive for BRCA1 and in 80 patients 22 were positive for BRCA2 [29,30]. So overall results show that BRCA mutations are strongly affecting patients who are diagnosed with prostate cancer.
In conclusion, the study shows that there is a significant relationship associated with the BRCA2 mutations which not only be the major risk for developing Hereditary and sporadic Prostate cancer it also helps to know the prognosis of the disease. BRCA1 mutation did not show a significant relationship but it affects the patients and screening can help to identify and treat them, which decreases the aggressiveness of the disease. In future, sequencing and screening of these mutations can be the major biomarkers which help in the early detection of Prostate cancer and also helps in targeted therapies which directly act on particular cell and are effective on the metabolic level.
Acknowledgments
Statement of Transparency and Principals:
· Author declares no conflict of interest
· Study was approved by Research Ethic Committee of author affiliated Institute.
· Study’s data is available upon a reasonable request.
· All authors have contributed to implementation of this research.
References
- Epidemiology of Prostate Cancer Rawla P. World Journal of Oncology.2019;10(2). CrossRef
- Chromosome rearrangement associated inactivation of tumour suppressor genes in prostate cancer Mao X, Boyd LK , Yáñez-Muñoz RJ , Chaplin T, Xue L, Lin D, Shan L, et al . American Journal of Cancer Research.2011;1(5).
- Quantifying the role of PSA screening in the US prostate cancer mortality decline Etzioni R, Tsodikov A, Mariotto A, Szabo A, Falcon S, Wegelin J, DiTommaso D, et al . Cancer causes & control: CCC.2008;19(2). CrossRef
- An updated catalog of prostate cancer predictive tools Shariat SF , Karakiewicz PI , Roehrborn CG , Kattan MW . Cancer.2008;113(11). CrossRef
- Overdiagnosis and overtreatment of early detected prostate cancer Bangma C. H., Roemeling S., Schröder F. H.. World Journal of Urology.2007;25(1). CrossRef
- Prostate cancer Nelson WG , De Marzo AM , Isaacs WB . The New England Journal of Medicine.2003;349(4). CrossRef
- Diet, anthropometric measures and prostate cancer risk: a review of prospective cohort and intervention studies Dagnelie P. C., Schuurman A. G., Goldbohm R. A., Van den Brandt P. A.. BJU international.2004;93(8). CrossRef
- Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries Sung H, Ferlay J, Siegel RL , Laversanne M, Soerjomataram I, Jemal A, Bray F. CA: a cancer journal for clinicians.2021;71(3). CrossRef
- First-degree family history of prostate cancer is associated the risk of breast cancer and ovarian cancer Zheng Q, Ying Q, Ren Z, Zhang Q, Lu D, Wang H, Wei W. Medicine.2021;100(4). CrossRef
- Family History of Breast or Prostate Cancer and Prostate Cancer Risk Barber L, Gerke T, Markt SC , Peisch SF , Wilson KM , Ahearn T, Giovannucci E, Parmigiani G, Mucci LA . Clinical Cancer Research: An Official Journal of the American Association for Cancer Research.2018;24(23). CrossRef
- The role of BRCA1 and BRCA2 in prostate cancer Li D, Kumaraswamy , Harlan-Williams LM , Jensen RA . Frontiers in Bioscience (Landmark Edition).2013;18(4). CrossRef
- Hereditary prostate cancer: epidemiologic and clinical features Carter B. S., Bova G. S., Beaty T. H., Steinberg G. D., Childs B., Isaacs W. B., Walsh P. C.. The Journal of Urology.1993;150(3). CrossRef
- BRCA1-and BRCA2- associated hereditary breast and ovarian cancer.2016 Petrucelli N, Daly MB , Pal T. .
- The roles of BRCA1 and BRCA2 and associated proteins in the maintenance of genomic stability Gudmundsdottir K., Ashworth A.. Oncogene.2006;25(43). CrossRef
- Cellular functions of the BRCA tumour-suppressor proteins Boulton S. J.. Biochemical Society Transactions.2006;34(Pt 5). CrossRef
- Common gene rearrangements in prostate cancer Rubin MA , Maher CA , Chinnaiyan AM . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2011;29(27). CrossRef
- Germline mutations in penetrant cancer predisposition genes are rare in men with prostate cancer selecting active surveillance Brady L, Newcomb LF , Zhu K, Zheng Y, Boyer H, Sarkar ND , McKenney JK , et al . Cancer Medicine.2022;11(22). CrossRef
- Men seeking counselling in a Breast Cancer Risk Evaluation Clinic Freitas AC , Opinião A, Fragoso S, Nunes H, Santos M, Clara A, Bento S, et al . Ecancermedicalscience.2018;12. CrossRef
- Associations of high-grade prostate cancer with BRCA1 and BRCA2 founder mutations Agalliu I, Gern R, Leanza S, Burk RD . Clinical Cancer Research: An Official Journal of the American Association for Cancer Research.2009;15(3). CrossRef
- Germline BRCA mutations are associated with higher risk of nodal involvement, distant metastasis, and poor survival outcomes in prostate cancer Castro E, Goh C, Olmos D, Saunders E, Leongamornlert D, Tymrakiewicz M, Mahmud N, et al . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2013;31(14). CrossRef
- Targeted prostate cancer screening in BRCA1 and BRCA2 mutation carriers: results from the initial screening round of the IMPACT study Bancroft EK , Page EC , Castro E, Lilja H, Vickers A, Sjoberg D, Assel M, et al . European Urology.2014;66(3). CrossRef
- Autoimmune response to PARP and BRCA1/BRCA2 in cancer Zhu Q, Han S, Zhou C, Cai M, Dai L, Zhang J. Oncotarget.2015;6(13). CrossRef
- Inherited DNA-Repair Gene Mutations in Men with Metastatic Prostate Cancer Pritchard CC , Mateo J, Walsh MF , De Sarkar N, Abida W, Beltran H, Garofalo A, et al . The New England Journal of Medicine.2016;375(5). CrossRef
- Treatment Outcomes and Tumor Loss of Heterozygosity in Germline DNA Repair-deficient Prostate Cancer Annala M, Struss WJ , Warner EW , Beja K, Vandekerkhove G, Wong A, Khalaf D, et al . European Urology.2017;72(1). CrossRef
- Intraductal/ductal histology and lymphovascular invasion are associated with germline DNA-repair gene mutations in prostate cancer Isaacsson Velho P, Silberstein JL , Markowski MC , Luo J, Lotan TL , Isaacs WB , Antonarakis ES . The Prostate.2018;78(5). CrossRef
- Prevalence of Germline Variants in Prostate Cancer and Implications for Current Genetic Testing Guidelines Nicolosi P, Ledet E, Yang S, Michalski S, Freschi B, O'Leary E, Esplin ED , Nussbaum RL , Sartor O. JAMA oncology.2019;5(4). CrossRef
- Germline DNA Repair Gene Mutation Landscape in Chinese Prostate Cancer Patients Wei Y, Wu J, Gu W, Qin X, Dai B, Lin G, Gan H, et al . European Urology.2019;76(3). CrossRef
- Rare Germline Pathogenic Mutations of DNA Repair Genes Are Most Strongly Associated with Grade Group 5 Prostate Cancer Wu Y, Yu H, Li S, Wiley K, Zheng S, LaDuca H, Gielzak M, et al . European Urology Oncology.2020;3(2). CrossRef
- Imaging-based prostate cancer screening among BRCA mutation carriers-results from the first round of screening Segal N., Ber Y., Benjaminov O., Tamir S., Yakimov M., Kedar I., Rosenbaum E., et al . Annals of Oncology: Official Journal of the European Society for Medical Oncology.2020;31(11). CrossRef
- Reflex Testing for Germline BRCA1, BRCA2, PALB2, and ATM Mutations in Pancreatic Cancer: Mutation Prevalence and Clinical Outcomes From Two Canadian Research Registries Smith AL , Wong C, Cuggia A, Borgida A, Holter S, Hall A, Connor AA, et al . JCO precision oncology.2018;2. CrossRef
- Germline Pathogenic Variants in 7636 Japanese Patients With Prostate Cancer and 12 366 Controls Momozawa Y, Iwasaki Y, Hirata M, Liu X, Kamatani Y, Takahashi A, Sugano K, Yoshida T, Murakami Y, Matsuda K, Nakagawa H, Spurdle AB , Kubo M. J Natl Cancer Inst.2020;112(4). CrossRef
- A Germline Variant at 8q24 Contributes to Familial Clustering of Prostate Cancer in Men of African Ancestry Darst BF , Wan P, Sheng X, Bensen JT , Ingles SA , Rybicki BA , et al . European Urology.2020;78(3). CrossRef
- An inherited NBN mutation is associated with poor prognosis prostate cancer Cybulski C., Wokołorczyk D., Kluźniak W., Jakubowska A., Górski B., Gronwald J., et al . British Journal of Cancer.2013;108(2). CrossRef
- Prostate Cancer Risk by BRCA2 Genomic Regions Nyberg T, Frost D, Barrowdale Da, Evans DG , Bancroft E, Adlard J, Ahmed M, Barwell J, Brady AF , Brewer C, Cook J. European Urology.2020;78(4). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Biology , 2023
Author Details