Breast Cancer Literacy: Status of Peripheral Health Workers in Lucknow
Download
Abstract
Background: Every woman needs to know the facts, and the fact is, when it comes to breast cancer, every woman is at risk. India accounts for 7.2% of global cancer incidence, but in terms of mortality, the country accounts for 8.3% of global mortality. India faces a high burden of cancer with the late-stage presentation being a common feature. Early detection of cancer is an important strategy for improved survival and simple cost-effective treatment. Low levels of cancer awareness are a significant factor for delay in seeking treatment by women.
Objective: The present study was conducted among Peripheral Health Workers (PHWs) in the Lucknow district to assess their perception of risk factors of breast cancer, knowledge of symptoms, early detection methods, and their availability in the district.
Methods: The study was conducted from September 2017 to August 2018, among 450 female PHWs working in rural and urban areas of Lucknow. A semi-structured questionnaire was used to collect information about the awareness of PHWs regarding breast cancer. The awareness score was calculated based on their responses. Data were analyzed using SPSS version 24.0 (IBM Corporation).
Results: The mean score for overall knowledge of breast cancer was statistically significantly high in BHWs in comparison to ASHAs (Accredited Social Health Activist). The mean knowledge score of signs and symptoms was significantly high among BHWs (Basic Health Workers). PHWs that had undergone training for breast cancer had about 5 times higher chances of having an above-median score.
Conclusion: Current low awareness levels, scarcity of resources, and screening programs call for training and refresher pieces of training for peripheral level health workers to empower them to provide preventive health education and screening at the community level. Breastfeeding counseling sessions during home visits and VHNDs could be utilized as an opportunity to create awareness about breast cancer, especially its protective effect on breast cancer.
Introduction
Every woman needs to know the facts, and the fact is, when it comes to breast cancer, every woman is at risk. The incidence rate of breast cancer increased significantly by 3% annually over the time period 1988-2016 [1]. Female breast cancer is the leading cause of global cancer incidence in 2020, with an estimated 2.3 million new cases, representing 11.7% of all cancer cases; accounting for 1 in 4 cases in women [2]. It is the fifth leading cause of cancer mortality worldwide, with 685,000 deaths accounting for 1 in 6 cancer deaths in women [2]. Cancer breast (2 38 908) is expected to be the most common site of cancer in 2025 [1]. Early detection of cancer is an important strategy for improved survival and simple cost-effective treatment. India faces a high burden of cancer with late stage presentation being a common feature. India accounts for 7.2% of global cancer incidence, but in terms of mortality, country accounts for 8.3% global mortality [3]. This highlights the fact that cancer in India is tended to detect late. Among the data reported by the HBCRs, the majority of cases diagnosed with cancer breast in females, showed locoregional 57.0% spread, followed by 29.0% and 10.3% of cases with localized disease and distant metastasis, respectively [1].
Low levels of cancer awareness have been found to be a very important risk factor for delay in seeking treatment by the women. Gupta et al., (2015) [4] in their review of publications of eight years noted consistently low breast cancer literacy of risk factors among women in India, irrespective of their educational or socioeconomic status. Lay women as well as health personnel had low knowledge to perform BSE and very few of them practicing it regularly. Efforts to raise awareness about cancer are minimal in the country and even if available, awareness programs are concentrated more in the cities and have not reached the remote and rural parts of the country.
Given the current low level of awareness of Breast cancer (BC), delayed care-seeking among women and limited access to health services, urgent need is to create awareness of risk factors, sign and symptoms of BC among community and providing screening facilities available close to community so that women can avail it easily. NPCDCS program in India aims to prevent and control common Non Communicable diseases (NCDs) by increasing community awareness, facilitating early detection, and linking the identified cases with the follow-up and continuity of care through involvement of BHWs (Basic Health Workers) and ASHAs (Accredited Social Health Activist) at the primary care level. However, to correctly identify the cancer signs and symptoms, educating about the risk factors and motivating women for screening, health workers need to be themselves educated about every aspects of breast cancer. So, the present study was conducted among these Peripheral Health Workers (ASHAs and BHWs) in Lucknow district to assess their perception about risk factors of breast cancer, knowledge of symptoms, early detection methods and their availability in the district. This assessment will help the program manager’s in preparing training curriculum so that PHWs can engage communities effectively in cancer prevention programs and campaigns.
Materials and Methods
The present cross-sectional study was conducted from September 2017 to August 2018, among female Peripheral Health Workers (ASHAs and BHWs) working in rural and urban areas of Lucknow. There are nine Community Health Centers in the rural blocks and urban areas have eight Bal Mahila Chiktsalaya (BMCs) equivalent to urban CHCs in Lucknow. Three rural and three urban community health centres were randomly selected. List of BHWs and ASHAs working in CHCs was obtained. From the list, participant were selected randomly for the study. Selected participants were contacted telephonically and meeting was fixed as per their working schedule for interview. Participants who could not be contacted telephonically were contacted during their weekly or monthly meetings at their respective CHCs.
Sample size and sampling method
Assuming level of awareness for female cancers in peripheral health workers as 65%, taking design effect of 2, sample size of 450 was calculated. In rural areas, 325 PHWs (232 ASHAs and 93 BHWs) and 125 PHWs (90 BHWs and 35 ASHAs) from Urban CHCs were selected and interviewed [5].
Study tool
A semi-structured questionnaire tool was used to collect information. The questionnaire had four sections. In section one, information on bio-social characteristics (age, educational status, marital status, family H/O cancer, training status for female cancers etc.) was collected. In section two, 15 questions were asked to assess the perception of health workers regarding the influence of different risk factors on the probability of occurrence of breast carcinoma. In section three, information on awareness of signs / symptoms was obtained and in section four, awareness about early detection methods and available screening services in the district for breast cancer were assessed. The survey also identified the source of information of these workers. The questionnaire was pilot tested before being administered to the participants in the study. Written informed consent was taken from each selected participant.
Data analysis
After cleaning and checking for consistency, data were analyzed using SPSS version 24.0 (IBM Corporation). Pearson’s Chi-square and student t-test were used for testing the association between variables. A ‘p’ value of less than 0.05 was considered statistically significant. Bivariate analysis was conducted to analyse the relationship between significant socio-demographic factors and the breast cancer knowledge score. Significant factors were then included in the multivariate logistic regression analysis.
Awareness Score
Each correct answer on the questionnaire was assigned a score 1 while 0 was awarded for incorrect/ don’t know response. The maximum awareness score was 15 for risk factors and 10 for signs and symptoms and three for knowledge regarding early detection methods. The minimum score was zero. A total score for each participant was computed by summing the number of correct answers. Based on the scores obtained, knowledge of the health workers was further categorized into five grades: very poor (≤20%), poor (21-40%), average (41-60%), good (61-80%), very good (81-100%).
Ethical Clearance
Ethical clearance for this study was obtained from the Institutional Ethical Committee of the King George’s Medical University, UP, Lucknow (Ref. code: 89th ECM II B-thesis/P2) before the commencement of the study.
Results
Biosocial characteristics of the Peripheral health workers The mean age of the PHWs was 36.5±8.3 years (36.2+6.3 and 37.1+10.5 years respectively for ASHAs and BHWs). Most of the PHWs were less than 50 years of age. Almost all of the BHWs were educated up to senior secondary or above while 40% of ASHAs were educated up to senior secondary level or more. The majority (88%) of ASHAs was from lower-middle or lower socioeconomic class while 40% of BHWs belonged to the middle or upper-middle class. The majority of PHWs were married (86.2%), Hindus (95.8%), and had parity of ≥2 (71%). About 7% of workers had history of regular OCP intake and 76% had breastfed their children. Only 36% of them were doing any form of physical exercise [5].
Training status
The mean duration of service was 7.3±5.6 years (7.7±4.6years and 6.7±6.7 years for ASHAs and BHWs respectively). Only 34 (7.6%) PHWs had ever received training for any type of cancer (4.9% ASHAs vs. 11.5% BHWs). Out of these 34, almost all of the PHWs had received training on breast cancer. 67% of them received training on cancers in the last five years. Beside doctors (54%), mass media (21.8%), and family and friends (10.7%) were other important source of information on cancers.
Overall knowledge of breast cancer knowledge
Mean score for overall knowledge of breast cancer (combining knowledge of risk factors, signs and symptoms, and screening methods) was statistically significantly high in BHWs in comparison to ASHAs (8.2±4.5 ASHAs Vs 9.7±5.1 BHWs). No significant difference was observed in the mean score obtained by the two groups regarding knowledge of risk factors and screening methods. However, the mean knowledge score of signs and symptoms was significantly high among BHWs (3.6+3.1 vs. 4.9±3.1: ASHAs vs. BHWs).
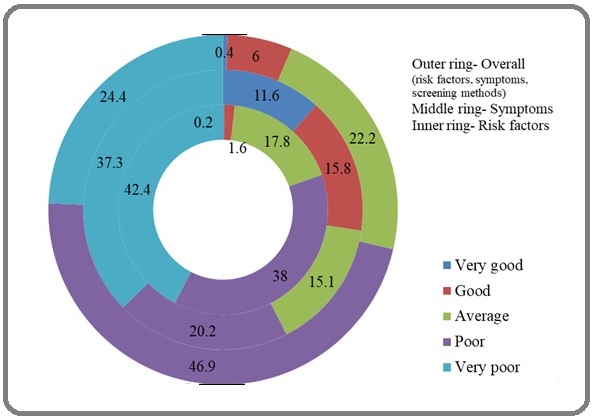
“Below-average” grading for overall knowledge was obtained by about two-thirds of the PHWs (Figure 1).
Figure 1. Grading of Awareness of Breast Cancer among PHWs.
However, knowledge of symptoms was more than risk factors among BHWs as well as in the ASHAs.
About one-third of the ASHAs and BHWs perceived, that prolonged use of Oral Contraceptive Pills (>10 years) will not affect the probability of having breast cancer in a woman (Table 1).
| Probability of having breast cancer in awoman with these conditions | Don’t know | Increased risk | Decreased risk | No effect | ||||
| ASHAs | BHWs | ASHAs | BHWs | ASHAs | BHWs | ASHAs | BHWs | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Use of Oral Contraceptive Pills (>10 years) | 71 (38.8) | 95 (35.6) | 46 (25.1) | 70 (26.2) | 14 (7.7) | 12 (4.5) | 52 (28.4) | 90 (33.7) |
| Late age at first child birth (> age 30 years) | 75 (41.0) | 124 (46.4) | 58 (31.7) | 90 (33.7) | 8 (4.4) | 10 (3.7) | 42 (23.0) | 43 (16.1) |
| Obesity | 79 (43.2) | 115 (43.1) | 53 (29.0) | 77 (28.8) | 5 (2.7) | 9 (3.4) | 46 (25.1) | 66 (24.7) |
| Breastfeeding the child for at least one year | 48 (26.2) | 68 (25.5) | 11 (6.0) | 30 (11.2) | 70 (38.3) | 85 (31.8) | 54 (29.5) | 84 (31.5) |
| Tobacco Smoking | 38 (20.8) | 69 (25.8) | 128 (69.9) | 182 (68.2) | 2 (1.1) | 2 (0.7) | 15 (8.2) | 14 (5.2) |
| Alcohol intake | 52 (28.4) | 86 (32.2) | 111 (60.7) | 153 (57.3) | 3 (1.6) | 2 (0.7) | 17 (9.3) | 26 (9.7) |
| Lack of physical activity (<30 min/ day) | 66 (36.1) | 113 (42.3) | 33 (18.0) | 57 (21.3) | 23 (12.6) | 23 (8.6) | 61 (33.3) | 74 (27.7) |
| Hormone therapy after menopause | 113 (61.7) | 202 (75.7) | 34 (18.6) | 34 (12.7) | 22 (12.0) | 10 (3.7) | 14 (7.7) | 21 (7.9) |
| Early menarche (< 12 years of age) in girls | 103 (56.3) | 164 (61.4) | 16 (8.7) | 57 (21.3) | 9 (4.9) | 8 (3.0) | 55 (30.1) | 38 (14.2) |
| Late menopause (>55 years of age) in women | 72 (39.3) | 150 (56.2) | 46 (25.1) | 64 (24.0) | 18 (9.8) | 9 (3.4) | 47 (25.7) | 44 (16.5) |
| Family H/O breast cancer in mother, sister | 53 (29.0) | 97 (36.3) | 49 (26.8) | 67 (25.1) | 2 (1.1) | 4 (1.5) | 79 (43.2) | 99 (37.1) |
| Exposure to Radiation therapy in past | 84 (45.9) | 150 (56.2) | 38 (20.8) | 64 (24.0) | 27 (14.8) | 17 (6.4) | 34 (18.6) | 36 (13.5) |
| Breast injury in the past | 47 (25.7) | 84 (31.5) | 108 (59.0) | 151 (56.6) | 2 (1.1) | 5 (1.9) | 26 (14.2) | 27 (10.1) |
| Stress | 61 (33.3) | 102 (38.2) | 58 (31.7) | 100 (37.5) | 3 (1.6) | 5 (1.9) | 61 (33.3) | 60 (22.5) |
Only 38.3% and 31.8% of the ASHAs and BHWs respectively perceived that breastfeeding the child will decrease the risk of breast cancer in a woman. Nearly one-fifth of BHWs and ASHAs had opined that late menopause will increase the risk of having breast cancer. Few (8.7%) ASHAs perceived that early menarche will increase the probability of breast cancer. About one third of the BHWs opined that family history of breast cancer will have no effect on the probability of having breast cancer in a woman. More than 60% of ASHAs and BHWs perceived the increased probability of the occurrence of breast cancer in women drinking alcohol or smoking.
No significant difference in knowledge of the ASHAs and BHWs regarding risk factors was observed in the study. The percent awareness of modifiable (or preventable) risk factors of breast cancer (Figure 2) with evidence such as late age at first child-birth (32.9%), use of OCPs (25.8%), obesity (28.9%), and sedentary lifestyle (20.0%) was less among PHWs.
Figure 2. Percent Awareness of Breast Cancer Risk Factors among Peripheral Healthcare Workers (N=450).

However, tobacco smoking (68.9%) and alcohol intake (58.7%) was reported by a higher number of PHWs. Awareness about non-modifiable risk factors with sufficient evidence such as the age of the women (0.3%), family history (25.8%), early menarche (16.2%), and late menopause (24.4%) was low among both ASHAs and BHWs.
About 9.3 percent of the peripheral health workers (8.6% ASHAs Vs 10.4%BHWs) were not aware of any risk factor for breast cancer. Only four BHWs were aware of all the four strong risk factors for breast cancer (viz. Long duration of use OCPs, Family history of breast cancer, late age at first childbirth and not breastfeeding the child) and none of the ASHAs was aware of all these four strong risk factors of carcinoma breast.
Sixteen percent of the PHWs (19.1% ASHAs Vs 11.5% BHWs) were not aware of any signs/symptoms of breast cancer. Only 17 percent PHWs (15.4% ASHAs Vs19.1% BHWs) were aware of four common signs and symptoms of breast carcinoma (viz. Lump in the breast, discharge from one or both nipples, Puckering or dimpling of the skin of the breasts and Pulled-in nipple). Most (72.9%) of the PHWs were aware of the presence of a lump in the breast or axilla region (Figure 3).
Figure 3. Knowledge of Peripheral Healthcare Workers regarding Signs/ Symptoms of Breast Cancer (N=450).
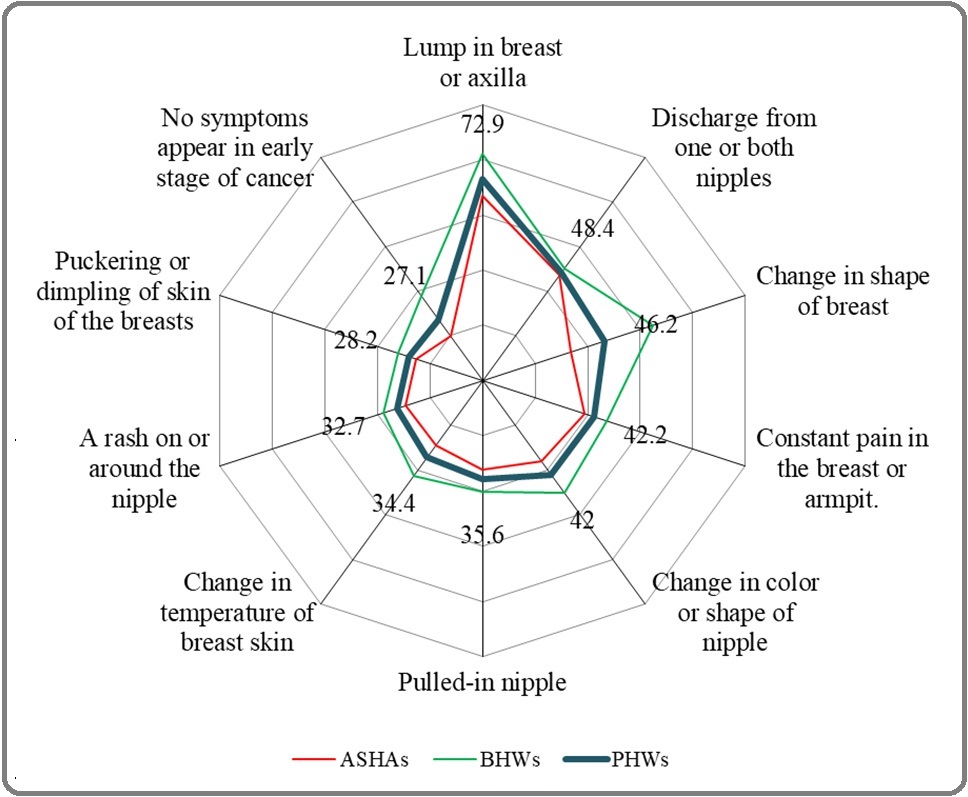
Out of the PHWs who were aware of a lump in the breast as a sign of cancer, most (83.5%) of them also perceived that every lump is not cancer. Awareness about the lump in the breast, change in the shape of the breast, change in color and shape of the nipple, and change in temperature of breast skin as a sign of breast carcinoma was significantly high among BHWs. About 27% of PHWs (19.9% ASHAs vs 37.7% BHWs) opined that no symptoms appear in the early stage of breast cancer.
Three-fourth (75.3%) of the PHWs was aware that early detection of breast cancer is possible with appropriate investigations (Table 2).
| Awareness and Perception | ASHAs (n=267) | BHWs (n=183) | Total (N=450) | * p-value |
| n (%) | n (%) | N (%) | ||
| Percent of PHWs aware of | ||||
| Early detection of breast cancer is possible with appropriate investigations | 199 (74.5) | 140 (76.5) | 339 (75.3) | 0.32 |
| Chances of survival improves, if breast cancer detected in early stage | 165 (61.8) | 152 (83.1) | 317 (70.4) | 0 |
| Regular screening for breast cancer is required in female 30 years and above | 30 (11.2) | 41 (22.4) | 71 (15.8) | 0.001 |
| Breast cancer is incurable | 215 (80.5) | 156 (85.2) | 371 (82.4) | 0.35 |
| Percent of PHWs aware of investigations available for early detection of breast cancer ** | ||||
| Clinical Breast examination (CBE) | 104 (39.0) | 40 (21.9) | 144 (32.0) | 0 |
| Breast self-examination (BSE) | 32 (12.0) | 37 (20.2) | 69 (15.3) | 0.017 |
| Mammography | 26 (9.7) | 42 (23.0) | 68 (15.1) | 0 |
| Ultrasound | 4 (1.5) | 5 (2.7) | 9 (2.0) | 0.36 |
| Biopsy | 16 (6.0) | 54 (29.5) | 70 (15.6) | 0 |
| Blood test | 24 (9.0) | 10 (5.5) | 34 (7.6) | 0.17 |
| X-ray | 10 (3.7) | 4 (2.2) | 14 (3.1) | 0.35 |
| Percent of PHWs having knowledge of BSE procedure# | 17 (53.1) [6.3] | 26 (70.3) [14.2] | 43 (62.3) [9.6] | 0.28 |
| Place (s) identified by Health Workers where early detection facilities are available ** | ||||
| Primary Health Centre | 6 (2.2) | 3 (1.6) | 9 (2.0) | 0.65 |
| Community Health Centre/BMC | 16 (6.0) | 10 (5.5) | 26 (5.8) | 0.47 |
| District hospital | 67 (25.1) | 49 (26.8) | 116 (25.8) | 0.66 |
| Medical College | 155 (58.1) | 132 (72.1) | 287 (63.8) | 0.002 |
| Private health facilities | 19 (7.1) | 19 (10.4) | 38 (8.4) | 0.22 |
*Chi-square test; **Multiple answers; #( ) percentage among those who knew BSE [ ] percentage among total population
Majority (70%) of PHWs perceived that survival rate in breast cancer improved if detected in an early stage of the disease but this awareness was significantly low among the ASHAs. Only 15.8% PHWs knew that regular screening for breast cancer is required in a female 30 years and above. Awareness of early detection methods was very low among both ASHAs and BHWs. Only 32.0% PHWs were aware of clinical breast examination (CBE) as early detection method. Only 9.6% of PHWs were aware of BSE procedure. Among 189 PHWs, who identified BSE or CBE as an early detection method, only about one-fourth of the PHWs (18 ASHAs and 32 BHWs) had undergone CBE/ BSE at least once in the last six months. Majority (63.8%) of health workers said that early detection methods are available at medical colleges whereas one-fourth responded that early detection facilities are available at the district hospital. Few (5.8%) identified CHC/BMC as place where facilities for early detection is available.
Designation of PHWs, their age in years, and duration of service, socioeconomic status and training status for breast cancer were found to be statistically significantly associated with knowledge score of breast cancer on bivariate analysis. Subsequently a logistic regression model was performed to ascertain the effects of socio-demographic variables on the likelihood of getting above-median breast cancer knowledge score. PHWs with less than 10 years of duration of service, higher socioeconomic status, and those who received training for breast cancer were associated with the likelihood of getting better scores for breast cancer knowledge. PHWs that had undergone training for breast cancer had about 5 times higher chances of having an above-median score (Table 3).
| Variables | Bivariate Analysis | Multivariate Analysis | ||
| Odds ratio (95% CI) | p value | Odds ratio (95% CI) | * p value | |
| Age (years) | ||||
| ≤35 | 1.50 (1.03-2.19) | 0.035 | - | - |
| >35 | -References- | |||
| Designation | ||||
| ASHAs | 0.63 (0.43-0.91) | 0.015 | - | |
| BHW | -References- | |||
| Duration of service (years) | ||||
| ≤ 10 | 1.92 (1.31-2.80) | 0.001 | 1.63 (1.10- 2.41) | 0.014 |
| >10 | -References- | |||
| Socioeconomic status | ||||
| Class I & II | 2.02 (1.28- 3.19) | 0.002 | 1.74 (1.09- 2.79) | 0.021 |
| Class III, IV & V | -References- | |||
| Training status for breast cancer | ||||
| Yes | 6.97 (2.63- 18.51) | 0 | 5.24 (1.94- 14.15) | 0.001 |
| No | -References- |
Discussion
Bello et al., (2012) in their article entitled, “Awareness is the first step in the battle against Breast Cancer”, emphasized on the importance of awareness to tackle the cancer. Breast cancer prevention is not simply about educating and empowering women; equipping health workers with the appropriate skills and attitudes is also crucial [6]. In order to motivate and guide the women for screening it is important for the health workers to be well aware of risk factors, sign symptoms and various screening modalities. In the current study, overall knowledge about breast carcinoma was “below average’’ in more than two-thirds PHWs. Most of the PHWs had poor to “very poor” knowledge of risk factors (80.4%) and symptoms (57.5%) of breast cancer. Only a few PHWs (4.1%ASHAs vs. 9.8% BHWs) had “average to the very good” overall knowledge of carcinoma breast. Few (7.6%) PHWs did received education on breast cancer.
The elevated incidence rates of breast cancer reflect a longstanding higher prevalence of reproductive and hormonal risk factors (early age at menarche, later age at menopause, advanced age at first birth, fewer number of children, less breastfeeding, menopausal hormone therapy, oral contraceptives) and lifestyle risk factors (alcohol intake, excess body weight, physical inactivity), as well as increased detection through organized or opportunistic mammographic screening [2]. Efforts to decrease excess body weight and alcohol consumption and to encourage physical activity and breastfeeding may have an impact in stemming the incidence of breast cancer [2]. Control of specific modifiable breast cancer risk factors could have an impact in reducing the incidence of breast cancer in the long term [7]. More than 60% health workers in our study perceived that alcohol and tobacco consumption increase probability of occurrence of cancer. But only one fourth reported lack of physical activity can increase the probability of breast cancer in women. Fotedar et al., (2013) reported physical inactivity was least known risk factor for BC among the nurses [8].
Strong preventable/ modifiable risk factors for breast cancer like late age at first childbirth, prolonged OCP use were not known to most of the PHWs. In the study only one third workers opined that late age at first birth will increase the risk of BC but also about one fifth of them responded that it will have no effect on the probability of breast cancer.
Current etiological hypotheses suggest that cancer of breast is linked with obesity. About forty percent of workers had no clue about the influence of obesity on the probability of cancer. Gupta et al., (2015) [4] suggests that inclusion of latest evidence regarding breast cancer is important in training of health workers so that they can transmit it in the community.
Use of Oral contraceptive pill was considered to be a risk factor for BC by 25% of the health workers but about one third were not aware that use of OCPs for prolonged time can increase the chances of occurrence of BC in a woman. In the study, about 7% of the health workers were using OCPs themselves regularly since last five years.
Apart from this, awareness of the influence of strong non -modifiable risk factors such as early age at menarche and late age at menopause on the probability of getting BC was also low among the health workers. Only 8% ASHAs said that early menarche will increase the probability of BC while 25% of ASHAs and BHWs both responded that late menopause will increase its probability. Gupta et al., (2015) [4] in their review of studies (eight year publications from 2005-2013) related to breast cancer awareness in India also observed consistently low level of awareness for important risk factors such as age at menarche, age at menopause, and age at birth of the first child in the general population (varied from 1% to 21%). They found women more commonly believed that unhealthy habits like alcohol and tobacco consumption are more important risk factors for breast cancer in comparison to reproductive history. Likewise more than two thirds of the health workers in the present study were aware of smoking (68.9%), alcohol intake (58.7%) as the risk factors for breast cancer.
Family history of breast cancer was not identified as a major risk factor by the health workers. About 40% of the health workers opined that it will not have any effect on the probability of having cancer in a woman and 30% were not sure of its influence on the occurrence of BC. Fotedar et al., (2015) [8], Dey et al., (2015) [9] and Dahiya et al., (2018) [10] in their study identified awareness regarding family history of breast cancer as risk factor for carcinoma. Breastfeeding can be protective for breast cancer,
as for every 12 months a woman breastfed, her risk of breast cancer decreased by 4.3% [11]. Only one-third of the PHWs said that breastfeeding the child will decrease the risk of breast cancer. Dey et al., (2015) [9] and Somdatta & Baridalyne, (2008) [12] stated that 24 to 75 percent women of Delhi were aware of protective effect of breastfeeding. Interestingly across the states various researchers observed higher percentage of the women both in rural or urban communities were aware of the fact that breastfeeding reduces risk for BC.
Myths like ‘previous breast injury’ and ‘mental tension’ increases the risk for breast cancer were existing among one-fourth of the PHWs. Interestingly, Somdatta & Baridalyne, (2008) [12] reported that 20% of the women believed that trauma to the breast while feeding leads to breast cancer.
Sixteen percent of the PHWs were not aware of any signs/symptom of breast cancer. According to 37% BHWs and 20% ASHAs in the study, clinically it is not possible to recognize breast cancer in the early stages. The most common physical sign cited was lump in breast (73%) and majority of them (83%) opined that “every lump is not cancer”. Ignorance of the seriousness of painless lump delayed the treatment seeking by the women [13]. However, 27 % of the health workers also opined that in case of breast cancer, lump will be associated with the pain.
Other common signs and symptoms: discharge from one or more nipples, puckering of skin of the breasts and pulled-in-nipple were known to 25%-50% health workers. Similar level awareness was reported by B. & Shankar., (2017) [14]. Women are not aware that breast cancer can also present without a lump [9].
To improve breast cancer outcome and survival, early detection is the cornerstone of breast cancer control. Screening is an alien word for most people in India. In the present study, one fourth of the health workers were oblivious to possibility of early detection of BC by any methods. Seventy percent of the health workers (61.8 ASHAs% vs. 83.1% BHWs) perceived that if detected early it will improve survival time. However, majority (82.4%) of them also perceived that in absence of early detection and timely treatment BC is fatal. Dey et al., (2015) [9] expressed that in spite of campaigns spreading messages in India that cancer is curable if detected early, nearly half of women in their study think BC is incurable. Researchers think reason behind this might be that very few women had seen other women cured of breast cancer.
The World Health Organization (WHO) has recommended low-cost screening approaches such as clinical breast examination (CBE) and breast self-examination (BSE) for developing countries with limited or no resources for early detection and diagnosis of breast cancer. Interestingly, in comparison to BHWs more ASHAs identified clinical breast examination as one of the early detection methods. BHWs were significantly more aware of mammography. Overall awareness about breast self-examination was low among ASHAs as well as BHWs. Only 15.3% health workers were aware breast self-examination. The awareness about BSE was significantly higher among BHWs but only about 20% of the BHWs were aware of it. Menon et al also found most ASHAs had not up to date knowledge for breast self-examination. In study among urban women by Somdatta & Baridalyne., (2008) [12] women said BC could only be detected by a doctor through clinical examination. Only 9.6% of health workers in the present study had knowledge to correctly perform steps of breast self-examination. Out of those who were aware of BSE procedure, only 26.5% had performed BSE on themselves for screening in last one year. Similar results were found by researches among women of rural and urban settlement areas where 25-50% of them were aware of BSE [9], but few were aware of correct method of BSE and very few were practicing it for screening themselves. Dahiya et al., (2018) [10] reported that the actual practice of BSE was low with only half of the subjects reporting practicing BSE with frequency ranging from once a month in 41% subjects to once a year in 15%. Fotedar et al., (2013) [8] found that fifty-four percent of participants in their study reportedly practice BSE at least once every year.
The target population for breast cancer screening is all women over 30 years of age was known to only 15.8 percent of the health workers. Health care providers are not knowledgeable about techniques; neither did they encourage women to implement screening.
Health care providers were not at the top of the list as a source of information. Instead electronic media and TV was noted to be the most important source of information on BC. For less educated women, it was relatives and friend who were the most important source of information. In conclusions, no significant difference in cancer literacy level was observed between BHWs and ASHAs. The existing breast cancer literacy level of BHWs and ASHAs was similar to the women, whom they are serving living in rural or urban slums. Awareness level was consistently low for stronger determinants of risk for breast cancer. Even health workers who were aware, uptake of screening methods for their own was very low. Current low awareness level, scarcity of resources and screening programs calls for training and refresher trainings of peripheral level health workers to empower them to provide preventive health education and screening at the community level. Breastfeeding counseling session during home visits and VHNDs could be utilized as an opportunity to create awareness about breast cancer, especially of its protective effect on breast cancer.
Strengths and limitations
For rolling out NPCDCS program, it is critical to prioritize the training of the ASHAs, ASHA facilitator and ANMs. Results of the present study can act as baseline data and help in assessment of effect of training. Limitation of the present study was that ASHAs and BHWs have different level of understanding but they were assessed using the same parameters which should have been different for both the groups.
Approval
Study was approved as a part of thesis.
Conflict of Interest
None
Ethical Declaration
Permission was obtained from the Institutional Ethical Committee of the King George’s Medical University UP, Lucknow, (Ref. code: 89th ECM II B-thesis/P2) before the commencement of the study.
References
- Report of National Cancer Registry Programme (2012-2016). In G.K. Rath (Ed.), Report of National Cancer Registry Programme (2012-2016) (Vol. 1, Issue December). ICMR- National Centre for Disease Informatics and Research. https://ncdirindia.org/All_Reports/Report_2020/default.aspx Rath GK , Gupta PC , Das AK , Ved RR , Arora NK , Chandra PS . 2020.
- Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries Sung H, Ferlay J, Siegel RL , Laversanne M, Soerjomataram I, Jemal A, Bray F. CA: a cancer journal for clinicians.2021;71(3). CrossRef
- Global cancer statistics, 2012 Torre LA , Bray F, Siegel RL , Ferlay J, Lortet-Tieulent J, Jemal A. CA: a cancer journal for clinicians.2015;65(2). CrossRef
- A review of breast cancer awareness among women in India: Cancer literate or awareness deficit? Gupta A, Shridhar K, Dhillon PK . European Journal of Cancer (Oxford, England: 1990).2015;51(14). CrossRef
- Cervical cancer: perception of peripheral health workers in Lucknow: a cross-sectional study Ansari A, Agarwal M, Singh VK , Nutan K, Deo S. International Journal Of Community Medicine And Public Health.2019;6(4). CrossRef
- Awareness is the first step in battle against breast cancer Bello M. Bulletin of the World Health Organization.2012;90(3). CrossRef
- WHO. (2014).Cancer Breast cancer : prevention and control. World Health Organization, 2007, 11–13. . CrossRef
- Knowledge of risk factors and early detection methods and practices towards breast cancer among nurses in Indira Gandhi Medical College, Shimla, Himachal Pradesh, India Fotedar V, Seam RK , Gupta MK , Gupta M, Vats S, Verma S. Asian Pacific journal of cancer prevention: APJCP.2013;14(1). CrossRef
- Breast cancer awareness at the community level among women in Delhi, India Dey S, Mishra A, Govil J, Dhillon PK . Asian Pacific Journal of Cancer Prevention.2015;16(13):5243-5251. CrossRef
- Knowledge and Practices Related to Screening for Breast Cancer among Women in Delhi, India Dahiya N, Basu S, Singh MC , Garg S, Kumar R, Kohli C. Asian Pacific journal of cancer prevention: APJCP.2018;19(1). CrossRef
- Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50 302 women with breast cancer and 96 973 women without the disease Beral V, Bull D, Doll R, Peto R, Reeves G. The Lancet.2002;360(9328). CrossRef
- Awareness of breast cancer in women of an urban resettlement colony Somdatta P, Baridalyne N. Indian Journal of Cancer.2008;45(4). CrossRef
- Awareness that early cancer lump is painless could decrease breast cancer mortality in developing countries Garg P. World Journal of Clinical Oncology.2016;7(3). CrossRef
- Awareness and screening behaviors of breast cancer among urban women in Mysuru, India- need for breast health education program B M, Shankar P. International Journal Of Community Medicine And Public Health.2017;4(8). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2023
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times