Ten-Year Experience of Epidemiological Trends and Clinical Patterns of Vulvar Tumors in a Regional Cancer Center in India
Download
Abstract
Background and objective: Vulvar tumors are relatively uncommon female genitourinary malignancies, primarily affecting postmenopausal women. Incidence and patterns of vulvar tumors vary across nations, influenced by numerous factors. This retrospective study aimed to evaluate the epidemiological patterns and clinical profiles of vulvar tumors in a regional cancer center in India.
Material and Methods: This retrospective study was conducted at a regional cancer center in India over a 10-year period. Data on demographic profiles and tumor characteristics of all vulvar tumor patients were collected from the record section and reviewed. These data were analyzed to understand the clinic-epidemiological trends of vulvar malignancy.
Results: A total of 47 patients with biopsy-proven vulvar malignancy were identified. The mean age at presentation was 63.4 years. The majority of patients were from rural origins, postmenopausal, and multiparous. Pruritus was the most common presenting symptom. Histopathologically, squamous cell carcinoma constituted the majority of cases. The labia was the most frequent site of presentation. Bilateral involvement was observed in one-third of patients, and inguinal lymphadenopathy and extensive disease were present in five and four patients, respectively.
Conclusion: This study, conducted at the sole referral cancer institute in the state, highlights the clinic-epidemiological trends of vulvar tumors in the region. Limited studies from different regions of India have published local patient data on vulvar tumors. A nationwide collaborative effort is necessary to understand the precise burden of this relatively rare malignancy, identify epidemiological trends and risk factors, and inform management strategies for these patients.
Introduction
Vulvar tumor, a relatively uncommon female genito-urinary tumor, contributes around 2000 new cases every year in India [1]. It constitutes approximately 4% of all gynaecological malignancies and less than 1% of all female cancers [2,3]. Old age, addiction of smoking, chronic dermatological condition like lichen and long-time infection with human papilloma virus (HPV) are the major risk factors associated with vulvar malignancy [4-6]. Majority of vulvar tumor are squamous cell carcinoma (SCC); rare varieties include melanoma, Paget’s disease, basal cell carcinoma & lymphoma [4,7]. Diagnosis is confirmed by detailed history and physical examination, vulvar biopsy and clinical imaging. Staging is done according to International Federation of Gynaecology and Obstetrics [FIGO] guideline [2,8]. Incidence and patterns of vulvar tumor differ from nation to nation, depending upon multiple factors [9]. Retrospective studies on vulvar malignancy from Western and Northeast part of India depicted epidemiological trends in those areas [10,11]. A few cancer institutes of Northern India have also reported their patients’ data [2,3]. The objective of this analysis was to evaluate epidemiological trends and clinical profile of vulvar tumor in our institution retrospectively.
Materials and Methods
This is a single institution-based retrospective study done in a regional cancer centre over a period of 10-years from January 2010 to December 2019. Permission from Institutional Review board was taken. Data regarding socio-demographic profile and tumor characteristics of all patients, having either fine needle aspiration cytology (FNAC) or biopsy proven vulvar malignancy, encountered in that stipulated time were collected from record section and reviewed. Informed consent was taken from the live patients as far as possible. All data thus gathered was analyzed using software (Microsoft Excel and Statistical Package for Social Sciences) to get a visualization about epidemiological trends and clinical pattern of vulvar malignancy in this part of nation and also compared with the global statistics.
Results
During the entire period, a total 10548-female patients having histologically confirmed malignancy were registered, of which 47-patients had biopsy proven vulvar malignancy. These constituted approximately 0.45% of total malignancy diagnosed in women.
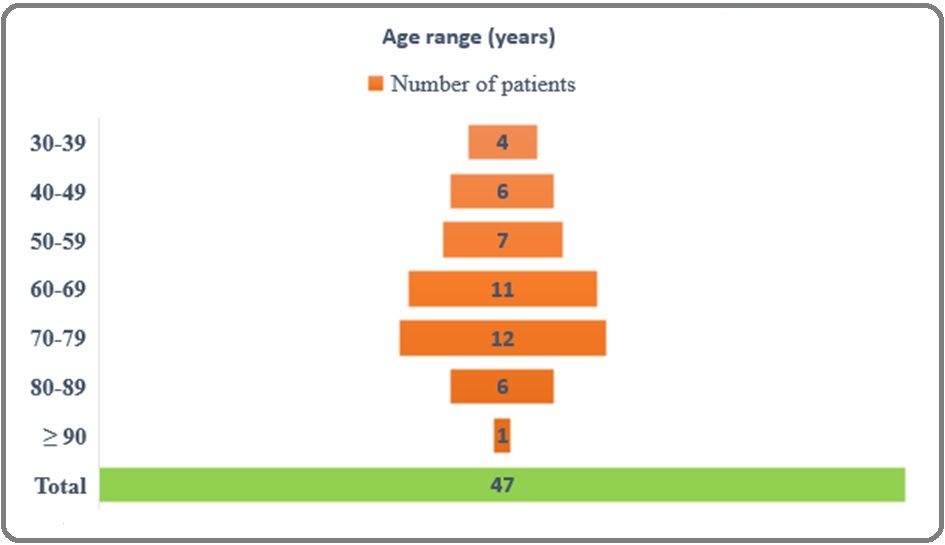
The age of the patients ranged from 30 to 90 years with mean age at presentation being 63.4 years. Greater part of the cases (49%) was seen in seventh and eighth decade of life (Figure 1).
Figure 1. Age Wise Distribution of Vulvar Malignancy.
Majority of the patients belonged to rural origin, rural to urban ratio being 2.9:1. Among all, around 78% patients (n=37) were post-menopausal at the time of diagnosis and only 7-patients (15%) were nulliparous. Overall, only 3-patients had a history of tobacco intake in the form of hookah smoking, others were free of addiction as per records.
At initial visit, 33-patients (70%) had a fair general condition with Karnofsky performance status (KPS) >70; only 3-patients had KPS <30 i.e. poor condition and the rest had average health status (KPS 30-70). Bulk of the patients had pruritus as typical presenting symptoms (61%) followed by ulceration (26%). Discharge from local site and pain were often associated with primary complaints. The duration of symptoms ranged from 2 to 14 months with a mean of eight months. Histopathologically, squamous cell carcinoma (SCC) constituted the major bulk (91.5%; n=43), most of them were either well- or moderately differentiated in grading. 4-cases of rare neoplasms were also observed; 1-case each of non-hodgkin lymphoma and vulvar melanoma and two cases of Paget’s disease. Verrucous carcinoma, the rare but indolent variant of SCC, was seen in 3-patients (Table 1).
| Histological Type | Number of patients (%) |
| Squamous Cell Carcinoma | 43 (91.5) |
| Well differentiated | 13 |
| Moderately differentiated | 19 |
| Poorly differentiated | 8 |
| Verrucous | 3 |
| Paget disease | 2 (4.3) |
| Melanoma | 1 (2.1) |
| Non-Hodgkin Lymphoma | 1 (2.1) |
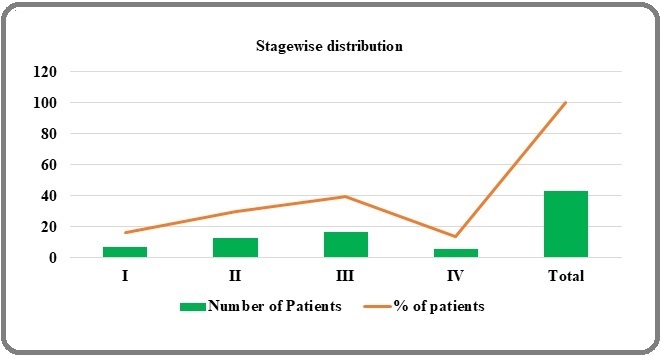
Labia (either majora, or minora or both) was the commonest site of presentation (76%; n=36). Bilateral vulva involvement was seen in 15-patients among these. These was ensued by inguinal lymphadenopathy and extensive multiple site involvement in five and four patients, respectively. 4-patients had disease in clitoris, while the patients diagnosed with NHL had localized, solid, non-tender, undistinguishable swelling. Surprisingly, none of the patient in our analysis had distant metastasis. Staging was done in all patients of vulvar SCC according to FIGO 2018 guideline, while the lymphoma and melanoma patient was staged as per Ann Arbor and Breslow staging system, respectively. Distribution of all SCC cases as per FIGO stage of disease was illustrated in Figure 2.
Figure 2. Distribution of All Vulvar Squamous Cell Carcinoma (SCC) as Per FIGO Staging.
Discussion
Our institute is a regional cancer centre and the only tertiary cancer centre serving all the cancer patients of this state over last three to four decades. Vulvar cancer is comparatively an infrequent malignancy with only 45240 cases per year globally [12]. Due to rarity of its occurrence, large scale prospective study would not be possible. Patient and tumor characteristics along with different treatment modalities and their impact over outcome in vulvar malignancy were mainly extrapolated from retrospective reviews. In recent years, a few articles globally have reported demographic and clinico-pathological profiles of vulvar tumor patients by retrospective analysis (Table 2) [3, 11, 13-18].
| Author | Year | Time period | Number of patients | Age | Post-menopausal status (%) | Multiparous (% of patients) | Histology |
| Schuurman et al [13] | 2013 | 22 years | 5680 | - | - | - | SCC-4614 Melanoma-341 Others-725 |
| Chhabra et al [11] | 2014 | 24 years | 18 | - | - | 72.22 | - |
| Buttmann-Schweiger et al [14] | 2015 | 13 years | 13125 | 71-73 years (median) | - | - | SCC-12205 Melanoma-414 Others-506 |
| Singh et al [3] | 2016 | 10 years | 41 | 52 years (mean) | 68.3 | 87.8 | SCC - 40 Non SCC – 1 |
| Kehila et al [15] | 2017 | 17 years | 76 | 65.4 years (mean) | 86.8 | 82.9 | SCC-72 Melanoma-4 |
| Lakhwani et al [16] | 2019 | 2.5 years | 5 | 58 years (mean) | 100 | 80 | SCC-5 |
| Mousavi et al [17] | 2019 | 20 years | 106 | 59.2 years (mean) | 80.2 | 92.5 | SCC-79 Melanoma-3 Others-26 |
| Tanaka et al [18] | 2019 | 35 years | 815 | - | - | - | SCC-389 Melanoma-28 Others- |
However, number of similar article from our country is limited. Incidence, demography, risk factors and tumor properties vary over geographical and cultural differences, it is worthwhile to document the same in the patients addressed by our hospital.
In the present study, the incidence of vulvar malignancy among all women malignancy is 0.45% which is nearly similar to study done by Chhabra et al in Western India [11]. However, Prevalence of vulvar cancer varies grossly over different parts of world. Southern Africa and Europe comprise a high burden of this malignancy, while the disease is infrequent in Gulf countries [9]. This might be due to prevalence of contributing infections like human-papilloma virus (HPV), behaviours factors like smoking and sexual habits in these population apart from geographical variations only.
Mean and median age of the patients analysed here were 63.4 and 66 years, respectively. These correlated very well with the conclusion of earlier published studies carried out in Northeast India as well in Western world [10, 19]. Age specific prevalence analysis, according to decade of life, revealed maximum cases (12 out of 47) in eighth decade of life i.e. between 70 to 79 years of age and minimum cases (4/47) in 4th decade (between 30 to 39 years) of life; which consolidated the outcome of previous study by Ouh et al [20]. No cases in our analysis was below 30 years of age. In a recently published global population based study, the researchers also concluded that incidence of vulvar cancer declined in women below 60-years of age, particularly for Indian inhabitants [9]. However, in comparison to the European literature, where the median age of vulvar tumor patients is around 71-73 years, our patients in the present review had comparatively younger age [21, 22]. Another study conducted in a Southern African country, where prevalence of vulvar cancer is comparatively more, median age of vulvar cancer patients was 42. This is due to higher prevalence of human immune virus (HIV) epidemic in that country and around 90% of that patient’s cohort were having prior HIV infection [23]. Anyhow, such variation in data demarcates the need of such study around different parts of world.
In these review, 76% of the total patients had disease in labia, and approximately two third had bilateral disease. These findings are very much in line with the global values [24]. However, local nodal involvement was seen in less patients (11% only) than that found in other studies [22, 25]. More than 90% of the vulvar malignancy in our institution revealed squamous cell carcinoma (SCC), which is consistent with other articles published over different parts of world [4, 7, 26]. Histological grading of all SCC tumors matched closely with National Cancer Institute (NCI) data [19]. Rare neoplasms were also found and addressed as per existing literature [27-29]. Bulk of the patients (nearly 70%) in our study were locally advanced that is in stage II and III; while around 15% cases were in stage I and IV. These values are similar with another Indian study by Nandwani et al, but does not match with the analysis by Lai et al [10, 30]. These may be due to deficiency of health awareness and lack of routine health check-up in our country. However, it is also satisfying to mention not a single patient was having stage IVB disease i.e. distant organ involvement.
The hallmark about the present article is that it was conducted in the regional cancer centre, where collaboration between all related department i.e. gynae- oncology, surgical-oncology, dermatology, and obviously radiation oncology, occurred. Limitation includes the retrospective nature of the analysis, and obviously, lack of immune-histochemical analysis in vulvar tumor. Another important fact not to miss, this analysis conducted on patients of vulvar tumor registered on our regional cancer centre only. A few patients visited outside our hospital, either to private clinicians or opted for traditional herbal medicine, cannot be counted and included in this review. Those will add more patients in our study cohort and help us to draw more clear cut idea about these less occurring tumor.
In conclusion, our study concludes that with a mean age of 63.4 years, vulvar cancer remains a health burden for older, especially for post-menopausal females. HPV and HIV status of these patients was not available in records and hence comments on their contribution in occurrence of vulvar tumor cannot be possible. Limited studies from different region of India have published local patients’ data on vulvar tumor. A nationwide collaboration in this regard will help to understand the exact burden of this relatively rare malignancy, epidemiological trends and risk factors as well as an idea about how to manage these patients.
References
- Cancer Statistics, 2020: Report From National Cancer Registry Programme, India Mathur P, Sathishkumar K, Chaturvedi M, Das P, Sudarshan KL , Santhappan S, Nallasamy V, John A, Narasimhan S, Roselind FS . JCO global oncology.2020;6. CrossRef
- Vulvar cancer: surgical management and survival trends in a low resource setting Kumar N, Ray MD , Sharma DN , Pandey R, Lata K, Mishra A, Wankhede D, Saikia J. Journal of the Egyptian National Cancer Institute.2020;32(1). CrossRef
- A cohort study of vulvar cancer over a period of 10 years and review of literature Singh N, Negi N, Srivastava K, Agarwal G. Indian Journal of Cancer.2016;53(3). CrossRef
- Cancer of the vulva: 2021 update Olawaiye AB , Cuello MA , Rogers LJ . International Journal of Gynaecology and Obstetrics: The Official Organ of the International Federation of Gynaecology and Obstetrics.2021;155 Suppl 1(Suppl 1). CrossRef
- Cervical and vulvar cancer risk in relation to the joint effects of cigarette smoking and genetic variation in interleukin 2 Hussain SK , Madeleine MM , Johnson LG , Du Q, Malkki M, Wilkerson H, Farin FM , et al . Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology.2008;17(7). CrossRef
- Lichen sclerosus and risk of cancer Halonen P, Jakobsson M, Heikinheimo O, Riska A, Gissler M, Pukkala E. International Journal of Cancer.2017;140(9). CrossRef
- Pathways of vulvar intraepithelial neoplasia and squamous cell carcinoma Del Pino M, Rodriguez-Carunchio L, Ordi J. Histopathology.2013;62(1). CrossRef
- FIGO staging for carcinoma of the vulva: 2021 revision Olawaiye AB , Cotler J, Cuello MA , Bhatla N, Okamoto A, Wilailak S, Purandare CN , et al . International Journal of Gynaecology and Obstetrics: The Official Organ of the International Federation of Gynaecology and Obstetrics.2021;155(1). CrossRef
- Geographic and temporal variations in the incidence of vulvar and vaginal cancers Bray F, Laversanne M, Weiderpass E, Arbyn M. International Journal of Cancer.2020;147(10). CrossRef
- An Overview of Vulvar Cancer: A Single-Center Study from Northeast India Nandwani M, Barmon D, Begum D, Liegise H, Kataki AC . Journal of Obstetrics and Gynaecology of India.2019;69(6). CrossRef
- Trends of vulvar cancer Chhabra S, Bhavani M, Deshpande A. Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology.2014;34(2). CrossRef
- Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries Sung H, Ferlay J, Siegel RK , Laversanne M, Soerjomataram I, Jemal A, Bray F. CA: a cancer journal for clinicians.2021;71(3). CrossRef
- Trends in incidence and survival of Dutch women with vulvar squamous cell carcinoma Schuurman MS , Einden LCG , Massuger LFAG , Kiemeney LA , Aa MA , Hullu JA . European Journal of Cancer (Oxford, England: 1990).2013;49(18). CrossRef
- Incidence patterns and temporal trends of invasive nonmelanotic vulvar tumors in Germany 1999-2011. A population-based cancer registry analysis Buttmann-Schweiger N, Klug SJ , Luyten A, Holleczek B, Heitz F, Bois A, Kraywinkel K. PloS One.2015;10(5). CrossRef
- Vulvar cancer in Tunisia: Epidemiological and clinicopathological features multicentric study Kehila M, Harabi S, Mhiri R, Touhami O, Abouda HS , Khlifi A, Hsairi M, et al . Journal of the Egyptian National Cancer Institute.2017;29(2). CrossRef
- Surgical Management of Carcinoma Vulva-Case Series and Review of Literature Lakhwani P, Agarwal P, Mahajan ja , Goel A, Pande P, Mehta S, Kumar K. Indian Journal of Surgical Oncology.2019;10(2). CrossRef
- Vulvar cancer in Iran: Retrospective study over 20 years (1998-2018) Mousavi A, Yousefnezhad A, Modarres-Gilani M, Akhavan S, Sheikh-Hasani S. Journal of Family Medicine and Primary Care.2019;8(4). CrossRef
- Trends in incidence and long-term survival of Japanese women with vulvar cancer: a population-based analysis Tanaka Y, Ueda Y, Kakuda M, Yagi A, Okazawa A, Egawa-Takata T, Matsuzaki S, et al . International Journal of Clinical Oncology.2019;24(9). CrossRef
- Squamous Cell Carcinoma of the Vulva: A Survival and Epidemiologic Study with Focus on Surgery and Radiotherapy Scampa M, Kalbermatten DE , Oranges CM . Journal of Clinical Medicine.2022;11(4). CrossRef
- Prevalence and Treatment of Vulvar Cancer From 2014-2018: A Nationwide Population-Based Study in Korea Ouh YT , Kang D, Kim H, Lee JK , Hong JH . Journal of Korean Medical Science.2022;37(4). CrossRef
- Vulvar cancer in Germany: increase in incidence and change in tumour biological characteristics from 1974 to 2013 Holleczek B, Sehouli J, Barinoff J. Acta Oncologica (Stockholm, Sweden).2018;57(3). CrossRef
- Four-decade trends in lymph node status of patients with vulvar squamous cell carcinoma in northern Italy Preti M, Bucchi L, Micheletti L, Privitera S, Corazza M, Cosma S, Gallio N, et al . Scientific Reports.2021;11(1). CrossRef
- Vulvar cancer in Botswana in women with and without HIV infection: patterns of treatment and survival outcomes MacDuffie E, Sakamuri S, Luckett R, Wang Q, Bvochara-Nsingo M, Monare B, Bazzett-Matabele L, et al . International Journal of Gynecological Cancer: Official Journal of the International Gynecological Cancer Society.2021;31(10). CrossRef
- Preoperative predictors of inguinal lymph node metastases in vulvar cancer - A nationwide study Schnack TH , Froeding LP , Kristensen E, Niemann I, Ørtoft G, Høgdall E, Høgdall C. Gynecologic Oncology.2022;165(3). CrossRef
- Vulvar carcinoma in Norway: A 50-year perspective on trends in incidence, treatment and survival Meltzer-Gunnes CJ , Småstuen MC , Kristensen GB , Tropé CG , Lie AK , Vistad I. Gynecologic Oncology.2017;145(3). CrossRef
- Locally advanced squamous cell carcinoma of the vulva: A challenging question for gynecologic oncologists Gadducci A, Aletti GD . Gynecologic Oncology.2020;158(1). CrossRef
- Vulvar melanoma: relevant aspects in therapeutic management Campaner AB , Fernandes GL , Cardoso FDA , Veasey JV . Anais Brasileiros De Dermatologia.2017;92(3). CrossRef
- Primary Non-Hodgkin's Lymphoma of the Vulva: A Case Report and Literature Review Clemente N, Alessandrini L, Rupolo M, Bulian P, Lucia E, Canzonieri V, Sopracordevole F. Medicine.2016;95(10). CrossRef
- Paget's disease of the vulva: A review of 89 cases Onaiwu CO , Salcedo MP , Pessini SA , Munsell MF , Euscher EE , Reed KE , Schmeler KM . Gynecologic Oncology Reports.2017;19. CrossRef
- Vulval cancer incidence, mortality and survival in England: age-related trends Lai J, Elleray R, Nordin A, Hirschowitz L, Rous B, Gildea C, Poole J. BJOG: an international journal of obstetrics and gynaecology.2014;121(6). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2023
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times