Intensity Modulated Radiotherapy (IMRT) Versus Helical Tomotherapy (HT) in Esophageal Cancer: A Comparative Analysis
Download
Abstract
Purpose/Objectives: Definitive chemoradiation is an accepted alternative treatment in the management of esophageal cancer in patients who are not candidates for surgery. The location of esophagus poses a challenge because of its close proximity to the critical organs. Various modern techniques of radiation planning offer the advantage of better dose conformality and increased sparing of organs at risk. This study aims to compare the dosimetric parameters of Intensity Modulated Radiotherapy (IMRT) and Helical Tomotherapy (HT) planning techniques in radical radiotherapy for esophageal cancer patients.
Materials/Methods: A total of 38 patients of esophageal squamous cell carcinoma with clinical staging cT2-T4/N0-N2/M0 planned for definitive chemoradiation were enrolled from June 2021 till November 2022. CT simulation was done with intravenous and oral contrast, and contouring of tumor volumes and organs at risk were done according to RTOG contouring guidelines. All patients were planned for a total dose of 50.4Gy in 28 fractions. Radiation plans of IMRT and HT were generated for each patient. Dosimetric parameters of PTV D98, D2, Dmean, V95, V110, Homogeneity Index (HI) and Conformity Index (CI) were noted for both the plans. Organs at risk (OAR) parameters such as Lung (V20, V30, V5, Dmean), Heart (V25, V30, Dmean), Spinal Cord Dmax, Larynx (Dmax, Dmean) and Liver Dmean were noted. All parameters of the two different planning techniques were compared and analyzed using SPSS software v23 with paired t-test.
Results: The coverage of the PTV in IMRT and HT was similar in terms of PTV V95 and PTV D98. The regions receiving more than 107% and 110% of the prescribed dose was significantly higher in IMRT compared to HT, on assessing V107, V110 and D2 (p=0.001). HI was similar in both the groups, but the CI was significantly better in HT compared to IMRT (0.9 ± 0.02 vs 1.03 ± 0.01; p=0.002). Doses to the lungs, heart and liver were similar between the two groups. IMRT had higher spinal cord (39.1 ± 3.2 vs 34.2 ± 5.5; p=0.001) and laryngeal dose (9.6 ± 5.5 vs 5.6 ± 3.7; p=0.009) compared to HT.
Conclusion: HT offers better dose conformality and uniformity when compared to IMRT with lesser dose to spinal cord and larynx. As this is a dosimetric study, a larger sample size and patient follow up is essential for clinical correlation and assessment of benefit of different radiation modalities.
Introduction
Esophageal cancer is currently fifth most common cancer in India, accounting for 4.8% of all malignancies [1]. It’s also the leading cancer site in males in the northeastern region of India [2]. Multimodality treatment with neoadjuvant chemoradiation (NACTRT) and surgery is the established standard of care [3,4]. A majority of our patients present with locally advanced cancers, which may not always be surgically amenable. Definitive chemoradiation (CTRT) is a widely accepted alternative treatment of early and locally advanced esophageal cancer patients who are surgically or medically inoperable, or in patients who refuse surgery [5]. Radiation treatment of esophageal cancer is challenging due to the critical location in the mediastinum. Its proximity to organs like the lungs and heart makes it difficult to achieve adequate dose coverage with conventional treatment techniques [4,6]. Higher doses of Organs at Risk (OAR) may result in acute or chronic pneumonitis, pulmonary fibrosis, cardiac dysfunction, or myelopathy. There is also an increased risk of pericardial effusion, myocardial ischemia, and heart failure.
Modern treatment techniques like Intensity Modulated Radiotherapy (IMRT) and Helical Tomotherapy (HT) can provide better dose coverage and simultaneously decrease the OAR doses [7,8]. The use of these techniques can result in better deliverance of chemoradiation with minimal toxicities. They provide a good conformality of dose distribution in Planning Target Volume (PTV). However, an increase in the low-dose region is of imminent concern. A desirable dose color wash with adequate sparing of OARs is the ultimate goal of all high-end planning modalities. This study aims to compare the dosimetric differences between IMRT and HT planning techniques for early and locally advanced esophageal cancer.
Materials and Methods
A total of 38 patients of esophageal cancer with histologically proven squamous cell carcinoma planned for definitive CTRT were enrolled from July 2021 till September 2022. The patient details are elaborated in Table 1.
| Characteristic | Total (n=38) |
| Age (years) | |
| Range | 38 – 72 |
| Median | 61 |
| Gender | |
| Male | 28 |
| Female | 10 |
| Location of tumor in esophagus | |
| Upper | 11 |
| Upper + Mid | 10 |
| Mid | 11 |
| Lower | 6 |
| Tumor length (cm) | |
| Range | 4.5 – 9 |
| Median | 7 |
| T stage | |
| T1 | - |
| T2 | 10 |
| T3 | 26 |
| T4 | 2 |
| N stage | |
| N0 | 18 |
| N1 | 12 |
| N2 | 8 |
| N3 | - |
| TNM Stage (AJCC 8th) | |
| Stage I | - |
| Stage II | 20 |
| Stage III | 16 |
| Stage IV | 2 |
| Radiation dose | 50.4 Gy |
| RT Technique | IMRT |
| Concurrent chemotherapy with Paclitaxel + Carboplatin | Median Cycles - 5 |
Planning CT scans with intravenous contrast were taken in the supine position with thermoplastic mould for immobilization. The contouring of Gross Tumor Volume (GTV), Clinical Target Volume (CTV), PTV, and OARs were done according to Radiation Therapy Oncology Group (RTOG) contouring guidelines as per 0436 protocol
[9] in MONACO Treatment Planning System (TPS) version 6.00.01. The OARs that were contoured included the Lungs, Heart, Spinal Cord, Larynx, and Liver. The CTV was delineated using a 3cm craniocaudal expansion and a 1cm radial expansion concerning GTV. The nodal volumes included depended upon the grossly enlarged nodes as well as the primary location of the GTV. All enlarged lymph nodes received a 1cm expansion, and were included in the CTV. A PTV margin of 1cm was given circumferentially to CTV as per our institution protocol, and a dose of 50.4 Gray (Gy) in 28 fractions (1.8 Gy per fraction) was prescribed. The objectives of planning were to ensure more than 95% coverage of the PTV with at least 95% of the prescribed dose with good conformality while maintaining the OAR dose constraints. All the patients were treated with the IMRT technique after approval of the planning. For the dosimetric comparison, the images were also transferred to PRECISION (ACCURAY) TPS, version 3.3.1.2 to generate plans for HT.
The Elekta Synergy Linac has 120 Multi-Leaf Collimator (MLC) systems with dynamic motion and variable dose rates. IMRT planning was done in MONACO TPS for Synergy with 6MV photons using 9 beams with Monte Carlo Optimization. Radixact-9 Helical Tomotherapy utilizes a rotating linear accelerator in a ring gantry with the couch in motion. It uses 6MV X-rays with a 64 leaves binary collimator of a 40 cm wide fan of thicknesses 0.625 cm to an isocenter of 85 cm. The MLC leaves open 51 times per rotation while closing in between as the gantry moves at a constant speed [10]. The TPS algorithm for treatment planning is convolution superimposition in PRECISION Software.
Each patient had both IMRT and HT plans generated with the same prescribed dose. The parameters analyzed for the PTV were D98 (dose received by 98% of PTV), D2 (dose received by 2% of PTV), V95 (volume of PTV receiving 95% of 50.4Gy), V110 (volume of PTV receiving 110% of 50.4Gy), and the Homogeneity Index and Conformity Index for both the plans. The homogeneity index (HI) was evaluated as the difference between the maximum and minimum dose to the target volume divided by the prescription dose. The conformity Index (CI) was calculated as the ratio of the reference isodose line to the treatment volume. The principal optimization criteria were set as 95% of the prescribed dose covering the whole PTV (V95), with no more than 1% of the PTV receiving more than 110% of the prescribed dose (V110). The OAR parameters included Lung V20, V30, V5 (volume of lungs receiving 20Gy, 30Gy and 5Gy respectively) and Dmean (mean dose), Heart V25, V30 and Dmean (volume of heart receiving 25Gy, 30Gy and mean dose respectively), Spinal Cord Dmax (maximum dose received), Larynx Dmax and Dmean, and Liver Dmean. The dose constraints attempted in the planning were according to QUANTEC guidelines [11]. The statistical analysis was done using the SPSS (Statistical Package for the Social Sciences) software version 22 (V22.0) with a paired t-test, and a p-value of less than 0.05 was taken as significant.
Results
The plan details of the two techniques including beam specifics and the average dose volume statistics of the PTV and OARs are summarized in Table 2.
| IMRT (n=38) | HT (n=38) | p value | |
| Radiation dose | 50.4 Gy | 50.4 Gy | |
| Number of beams | 9 | - | |
| HI | 1.06 ± 0.01 | 1.06 ± 0.02 | 0.42 |
| CI | 0.9 ± 0.02 | 1.03 ± 0.01 | 0.002 |
| PTV V95 | 99.6 ± 0.4 | 99.4 ± 0.6 | 0.15 |
| PTV V107 | 1.4 ± 0.9 | 0 | 0.001 |
| PTV V110 | 0.01 ± 0.01 | 0 | 0.001 |
| PTV D98 | 49.8 ± 0.6 | 49.7 ± 0.8 | 0.35 |
| PTV D2 | 53.7 ± 0.4 | 52.2 ± 0.6 | 0.02 |
| PTV Dmean | 51.9 ± 0.3 | 51.4 ± 0.4 | 0.12 |
| Lungs - V20 | 27.6 ± 6.6 | 26.6 ± 5.3 | 0.26 |
| V30 | 13.6 ± 4.1 | 12.4 ± 3.1 | 0.1 |
| V5 | 71.1 ± 18.6 | 73.1 ± 19.1 | 0.34 |
| Dmean | 14.8 ± 3.4 | 15 ± 3.1 | 0.41 |
| Heart - V25 | 23.8 ± 19.9 | 21.1 ± 14.9 | 0.27 |
| V30 | 18 ± 14.6 | 15.5 ± 11 | 0.22 |
| Dmean | 15.1 ± 10 | 15 ± 9.3 | 0.49 |
| Spinal Cord PRV Dmax | 47.1 ± 3.7 | 45.2 ± 4.5 | 0.039 |
| Spinal Cord Dmax | 39.1 ± 3.2 | 34.2 ± 5.5 | 0.001 |
| Larynx - Dmax | 42.5 ± 10.1 | 35.1 ± 16.4 | 0.003 |
| Dmean | 9.6 ± 5.5 | 5.6 ± 3.7 | 0.009 |
| Liver Dmean | 8.2 ± 8 | 9.1 ± 9 | 0.42 |
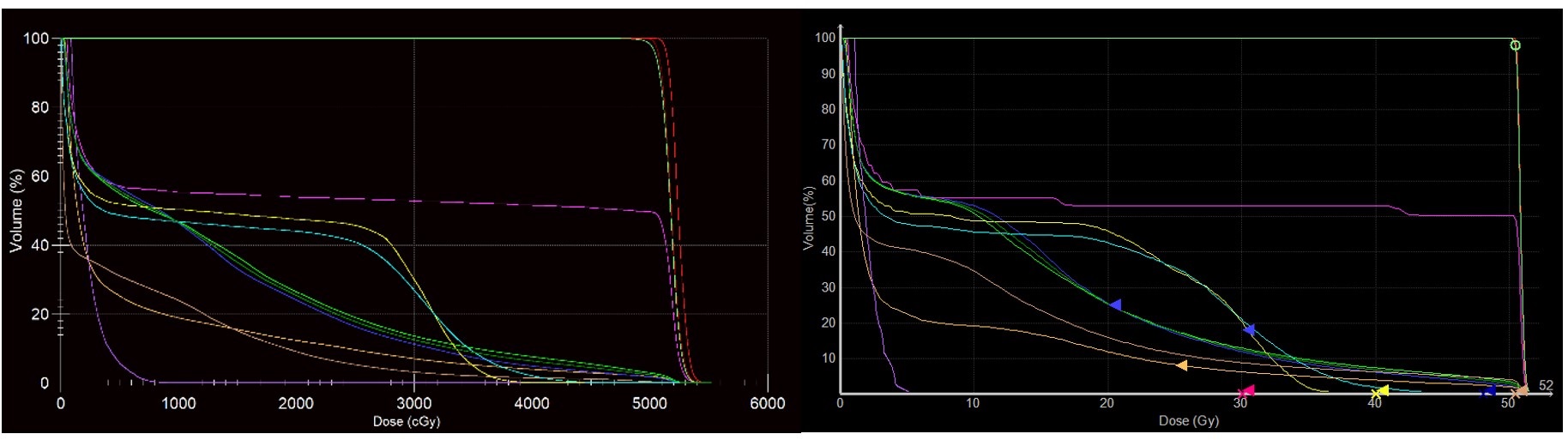
The dose color wash of two representative patients is shown in Figure 1 and the Dose Volume Histogram (DVH) comparison is shown in Figure 2.
Figure 1. a, Dose colour wash of 95% and 100% dose in IMRT; b, Dose colour wash of 95% and 100% dose in HT.
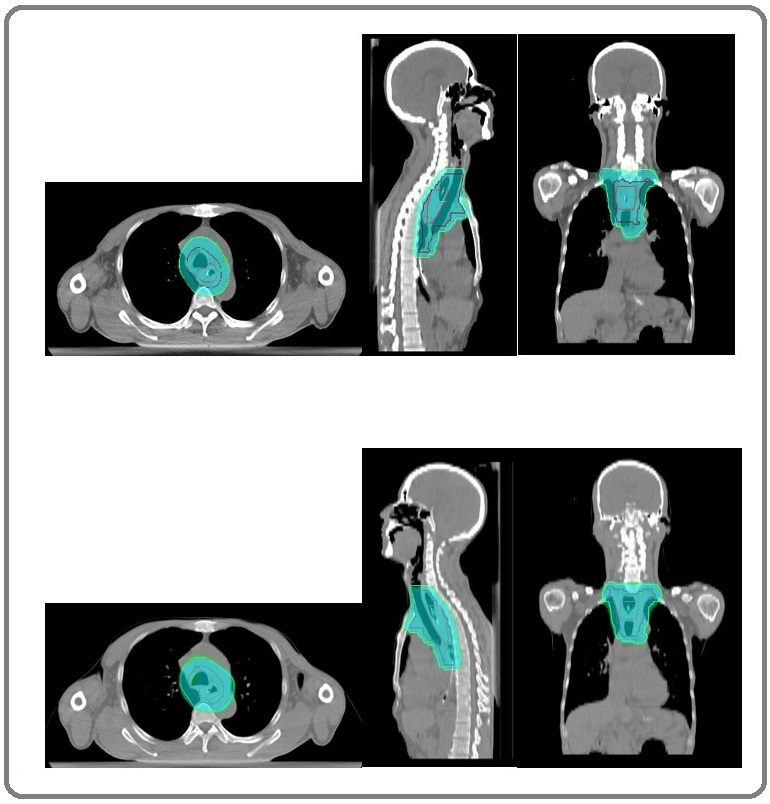
Figure 2. a, DVH IMRT; b, DVH HT.
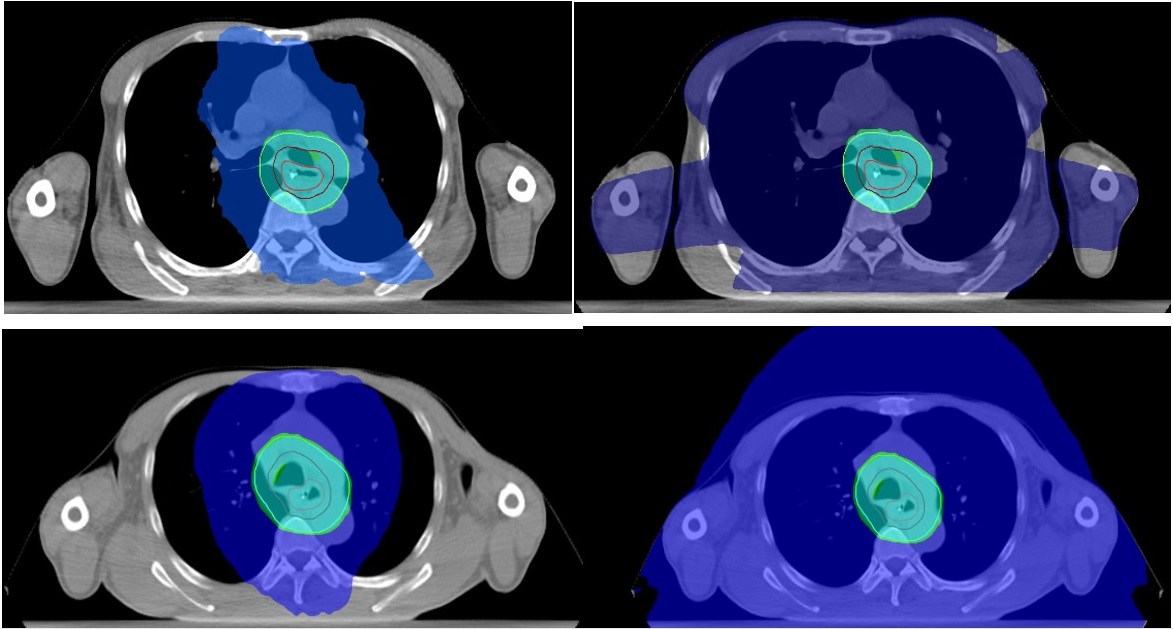
The coverage of the PTV in IMRT and HT was similar in terms of PTV V95 (99.6 ± 0.4% Vs 99.4 ± 0.6%; p = 0.15) and PTV D98 (49.8 ± 0.6 Gy Vs 49.7 ± 0.8 Gy; p = 0.35). However, the hot spots or the regions receiving more than 107% and 110% of the prescribed dose were significantly higher in IMRT compared to HT, as seen in assessing PTV V107, PTV V110, and PTV D2 (p=0.001, p= 0.001, p = 0.02, respectively). The volume of PTV receiving 107% and 110% of the prescribed dose was 0% in the HT group. The homogeneity index (HI) was similar in both the groups (1.06 ± 0.01 vs 1.06 ± 0.02; p = 0.42), but the conformity index (CI) was significantly better in HT compared to IMRT (0.9 ± 0.02 vs 1.03 ± 0.01; p = 0.002). The OARs assessed were the Lungs, Heart, and Spinal Cord in all patients. Larynx was assessed in patients receiving supraclavicular radiation, and the Liver was assessed in patients with distal esophageal disease. There was no significant difference in the dose received to the lungs between the IMRT and HT groups. The Lungs V20 (27.6 ± 6.6% vs 26.6 ± 5.3%; p = 0.26), V30 (13.6 ± 4.1% vs 12.4 ± 3.1%; p = 0.10), and Dmean (14.8 ± 3.4 Gy vs 15 ± 3.1 Gy; p = 0.41) were within the acceptable limits of the QUANTEC dose constraints in both the techniques [11]. But the low dose of Lungs, with respect to V5 (71.1 ± 18.6% vs 73.1 ± 19.1%; p = 0.34) was higher than the recommended <65% in both IMRT and HT arms. The low dose color wash region is shown in Fig 3 for both the plannings of a representative patient.
The dose received to the Heart was similar in both groups. The Heart V25 (23.8 ± 19.9% vs 21.1 ± 14.9%; p = 0.27), V30 (18 ± 14.6% vs 15.5 ± 11%; p = 0.22), and Dmean (15.1 ± 10 Gy vs 15 ± 9.3 Gy; p = 0.49) were not statistically different in IMRT and HT.
The Spinal Cord and Larynx doses however were significantly higher in the IMRT group compared to HT. The Spinal Cord PRV Dmax and Spinal Cord Dmax were higher in the IMRT group (47.1 ± 3.7 Gy vs 45.2 ± 4.5 Gy; p = 0.039; 39.1 ± 3.2 Gy vs 34.2 ± 5.5 Gy; p = 0.001 respectively). The Larynx Dmax (42.5 ± 10.1 Gy vs 35.1 ± 16.4 Gy; p = 0.003) and Dmean (9.6 ± 5.5 Gy vs 5.6 ± 3.7 Gy; p = 0.009) were also higher in IMRT arm compared to HT arm. The liver Dmean was similar in both groups (8.2 ± 8 Gy vs 9.1 ± 9 Gy; p = 0.42).
Discussion
The burden of esophageal cancer in northeastern India is the highest in our nation [2]. As a large proportion of the patients present with locally advanced esophageal cancers, the trimodality management with neoadjuvant chemoradiation and surgery is not always feasible. Some patients refuse surgery, for whom CTRT is a viable choice. Definitive CTRT has shown comparable results with patients undergoing NACTRT plus surgery [5,4]. Factors like tumor location, long-segment disease, chronic smoking history, pre-existing pulmonary dysfunctions, etc. can influence the radiation-induced toxicities seen in definitive CTRT. Hence, the need for better radiation treatment delivery is of utmost importance.
With the advent of IMRT, it has become possible to provide good dose coverage to the treatment volumes while maintaining an acceptable dose limit to the OARs. However, the risk of the subsequent increase in the low-dose region is always present. HT offers a different radiation delivery system in which patients are treated slice by slice. Although it provides better conformality compared to IMRT, the low doses of the OARs are comparable, if not more (Figure 3).
Figure 3. a, Dose Colour Wash of 20 Gy & 5 Gy in IMRT; b, Dose Colour Wash of 20 Gy & 5 Gy in HT.
Our study analyzes the dosimetric differences between the two techniques for a better understanding of striking a balance between adequate dose coverage and superior sparing of OARs.
Both IMRT and HT offered comparable dose coverage to the PTV, although dose homogeneity was better in HT. The V95 and D98 of PTV were 99.6% and 49.8 Gy respectively in IMRT, and 99.4% and 49.7 Gy respectively in HT, which were similar to the other dosimetric studies [12,13]. The volume of the PTV receiving higher than the prescribed dose, V107 and V110 was 0% in HT, showing better dose homogeneity compared to IMRT. The dose conformality was also better in HT, as seen with a CI of 1.03 when compared to the CI of 0.9 in IMRT. These observations were similar to the findings seen in previously conducted studies [13, 14]. As the patients are treated in a helical fashion with rotating linear accelerators, the underlying technology might explain the better CI seen in HT.
The patients included in this study had predominantly upper and mid-third esophageal lesions. Sparing of the lungs and heart became difficult even with the use of IMRT and HT. The majority of the patients had a long- segment disease, with the median length being 7cm. This resulted in significant radiation dose to the lungs and heart in both groups, as an increased amount of healthy tissue was being incorporated into the PTV. Invariably almost all patients of esophageal cancer treated in our institute have at least grade 1 pneumonitis during follow-up after CTRT. The use of IMRT results in a significant low-dose bath to the patient as evidenced by other studies [15,16], but the effect of HT has not been investigated extensively. The rotational technique can increase the spillage of the V5 which might result in long-term pulmonary complications.
Our study has shown similar lung dose parameters between both the techniques. Literature suggests that the development of radiation-induced pneumonitis can be reduced by adhering to reduced V20 and Mean dose to the lungs [17-19]. IMRT and HT techniques were able to achieve the dose constraints in V20 (27.6% vs 26.6%), V30 (13.6% vs 12.4%), and Dmean (14.8 Gy vs 15 Gy), similar to the available literature [13,14]. But the V5 of the lungs was higher compared to other studies. Wang et al showed an average V5 of 54.4% in HT and 44.8% in IMRT [13]. In our study, the V5 was 71.1% in IMRT and 73.1% in HT. This finding could be attributed to the long disease segments of the included patients. As the patients were treated with IMRT, the implication of HT in the patient’s treatment and its comparison with IMRT needs to be observed in a clinical and prospective setting. The cardiac dose parameter for long-term toxicity was not achieved by the techniques. This can be correlated to the long craniocaudal length of the PTV and the location of the tumors. The dose limit of V30 of less than 46% was achieved to reduce the acute effect of pericardial effusion [20]. However, all the assessed dose parameters of V25 (23.8% vs 21.1%), V30 (18% vs 15.5%), and Dmean (15.1 Gy vs 15 Gy) were significantly lower in our study in IMRT and HT compared to the existing data on dosimetric analysis [13,14]. The mean dose of the heart was also well below 26 Gy in both arms which could lessen chronic cardiac dysfunctions [21,22]. The Dmax to the spinal cord was significantly less in HT compared to IMRT, even for the spinal cord PRV. Both the plans were able to limit the maximum dose to an average of 39.1 ± 3.2 Gy in IMRT and 34.2 ± 5.5 Gy in HT, which is less than the recommended limit of less than 45 Gy [11]. However, HT fared better with improved dose homogeneity and conformality to PTV. The sparing of the spinal cord was better in our study than the doses achieved in previous studies [13-15].
Laryngeal toxicity has been mostly reported in cervical esophageal lesions [23,24], that were not included in our study. Patients with upper-third esophageal tumors who received supraclavicular radiation developed grade 1 and 2 laryngitis during the treatment which was resolved during follow-up. HT provided better sparing of the larynx, though the clinical effect cannot be assessed as this is a dosimetric study.
Our study provided a direct comparison between two modern radiation modalities to better decide the usage of the existing facilities in our region and to provide a curative treatment with reduced toxicities. We have observed that although both techniques were able to provide comparable dose parameters, HT might be better in terms of better conformality and decreased dose to OARs. As the availability of HT facilities in India is limited, IMRT is still the preferred technique due to better accessibility. As this study is a dosimetric comparison, the clinical comparison of both therapies cannot be assessed. The observations based on our study warrant further investigation using a larger sample size in a prospective randomized design, with an assessment of clinical end- points that could provide important insights into the long- term outcomes of esophageal cancer patients treated with modern-era radiation modalities.
In conclusion, this study demonstrates that the use of IMRT and HT in early and locally advanced esophageal cancer provides good conformality of radiation dose with acceptable dose volume parameters of the OARs. HT planning was found to be better in dose homogeneity and conformality, as well as decreased doses to the spinal cord and larynx. Both the plannings resulted in a large area of low-dose bath in the patients. As this study is a dosimetric analysis between IMRT and HT, the authors advocate for further investigation using randomized and prospective studies. A larger sample size and longer follow-up of the patients will provide concrete data on the long-term clinical implications of both techniques.
Acknowledgements
I would like to thank Dr. B.C. Goswami, Dr. S. Goswami, Dr. G. Bora and Dr. M. Paul for their constant support and help regarding this research.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors.
The authors declare no conflict of interest.
References
- International Agency for Research on Cancer (2020). Population Fact Sheets: India [online] Website https://gco.iarc.fr/today/data/factsheets/populations/356-india-fact-sheets.pdf [accessed 02/03/2023]..
- Indian Council of Medical Research – National Centre for Disease Informatics and Research: Report of National Cancer Registry Programme 2020 [online] Website https://ncdirindia.org/All_Reports/Report_2020/default.aspx [accessed 02/03/2023]..
- Progress report of combined chemoradiotherapy versus radiotherapy alone in patients with esophageal cancer: an intergroup study Sarraf M, Martz K, Herskovic A, Leichman L, Brindle JS , Vaitkevicius VK , Cooper J, Byhardt R, Davis L, Emami B. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.1997;15(1). CrossRef
- Chemoradiotherapy of locally advanced esophageal cancer: long-term follow-up of a prospective randomized trial (RTOG 85-01). Radiation Therapy Oncology Group Cooper JS , Guo MD , Herskovic A, Macdonald JS , Martenson JA , Al-Sarraf M, Byhardt R, et al . JAMA.1999;281(17). CrossRef
- INT 0123 (Radiation Therapy Oncology Group 94-05) phase III trial of combined-modality therapy for esophageal cancer: high-dose versus standard-dose radiation therapy Minsky BD , Pajak TF , Ginsberg RJ , Pisansky TM , Martenson J, Komaki R, Okawara G, Rosenthal SA , Kelsen DP . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2002;20(5). CrossRef
- Late toxicity after definitive concurrent chemoradiotherapy for thoracic esophageal carcinoma Morota M, Gomi K, Kozuka T, Chin K, Matsuura M, Oguchi M, Ito H, Yamashita T. International Journal of Radiation Oncology, Biology, Physics.2009;75(1). CrossRef
- Hybrid IMRT for treatment of cancers of the lung and esophagus Mayo CS , Urie MM , Fitzgerald TJ , Ding L, Lo YC , Bogdanov M. International Journal of Radiation Oncology, Biology, Physics.2008;71(5). CrossRef
- Comparing planning time, delivery time and plan quality for IMRT, RapidArc and Tomotherapy Oliver M, Ansbacher W, Beckham WA . Journal of Applied Clinical Medical Physics.2009;10(4). CrossRef
- Expert Consensus Contouring Guidelines for Intensity Modulated Radiation Therapy in Esophageal and Gastroesophageal Junction Cancer Wu AJ , Bosch WR , Chang DT , Hong TS , Jabbour SK , Kleinberg LR , Mamon HJ , Thomas CR , Goodman KA . International Journal of Radiation Oncology, Biology, Physics.2015;92(4). CrossRef
- Radiation characteristics of helical tomotherapy Jeraj R, Mackie TR , Balog J, Olivera G, Pearson D, Kapatoes J, Ruchala K, Reckwerdt P. Medical Physics.2004;31(2). CrossRef
- Quantitative Analysis of Normal Tissue Effects in the Clinic (QUANTEC) Summary of Dose Constraints - Approximate Dose/Volume/Outcome Data for Several Organs Following Conventional Fractionation Website http://individual.utoronto.ca/dtsang/misc/quantec.pdf [accessed 02/03/2023]..
- Helical tomotherapy for radiotherapy in esophageal cancer: a preferred plan with better conformal target coverage and more homogeneous dose distribution Chen YJ , Liu A, Han C, Tsai PT , Schultheiss TE , Pezner RD , Vora N, et al . Medical Dosimetry: Official Journal of the American Association of Medical Dosimetrists.2007;32(3). CrossRef
- Radiotherapy for esophageal cancer using simultaneous integrated boost techniques: dosimetric comparison of helical TomoTherapy, Volumetric-modulated Arc Therapy (RapidArc) and dynamic intensity-modulated radiotherapy Wang YG , Chen SW , ChienCR , HsiehTC , Yu CY , Kuo YC , Yang SN , et al . Technology in Cancer Research & Treatment.2013;12(6). CrossRef
- Dosimetric comparison of helical tomotherapy, RapidArc, and a novel IMRT & Arc technique for esophageal carcinoma Martin S, Chen JZ , Rashid Dar A, Yartsev S. Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2011;101(3). CrossRef
- [Dosimetric comparison of the helical tomotherapy, intensity-modulated radiotherapy and volumetric-modulated arc therapy in radical radiotherapy for esophageal cancer] Xu YJ , Li P, Hu X, Wang J, Ma HL , Chen M. Zhonghua Yi Xue Za Zhi.2019;99(41). CrossRef
- A comparison of conventional and conformal radiotherapy of the oesophagus: work in progress Guzel Z, Bedford JL , Childs PJ , Nahum AE , Webb S, Oldham M, Tait D. The British Journal of Radiology.1998;71(850). CrossRef
- Principles and techniques of radiation therapy for esophageal and gastroesophageal junction cancers Hazard L, Yang G, McAleer MF , Hayman J, Willett C. Journal of the National Comprehensive Cancer Network: JNCCN.2008;6(9). CrossRef
- Dose-volumetric parameters for predicting severe radiation pneumonitis after three-dimensional conformal radiation therapy for lung cancer Kim TH , Cho KH , Pyo HR , Lee JS , Zo JI , Lee DH , Lee JM , et al . Radiology.2005;235(1). CrossRef
- Prediction of radiation pneumonitis by dose - volume histogram parameters in lung cancer--a systematic review Rodrigues G, Lock M, D'Souza D, Yu E, Van Dyk J. Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2004;71(2). CrossRef
- Postoperative pulmonary complications after preoperative chemoradiation for esophageal carcinoma: correlation with pulmonary dose-volume histogram parameters Lee HK , Vaporciyan AA , Cox JD , Tucker SL , Putnam JB , Ajani JA , Liao Z, et al . International Journal of Radiation Oncology, Biology, Physics.2003;57(5). CrossRef
- Risk factors for pericardial effusion in inoperable esophageal cancer patients treated with definitive chemoradiation therapy Wei X, Liu HH , Tucker SL , Wang S, Mohan R, Cox JD , Komaki R, Liao Z. International Journal of Radiation Oncology, Biology, Physics.2008;70(3). CrossRef
- Long-term toxicity after definitive chemoradiotherapy for squamous cell carcinoma of the thoracic esophagus Ishikura S, Nihei K, Ohtsu A, Boku N, Hironaka S, Mera K, Muto M, Ogino T, Yoshida S. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2003;21(14). CrossRef
- Treatment Outcomes of Patients with Locally Advanced Synchronous Esophageal and Head/Neck Squamous Cell Carcinoma Receiving Curative Concurrent Chemoradiotherapy Chen YH , Lu HI , Chien CY , Lo CM , Wang YM , Chou SY , Su YY , Shih LH , Li SH . Scientific Reports.2017;7. CrossRef
- Long-term outcome of definitive radiotherapy for cervical esophageal squamous cell carcinoma Sakanaka K, Ishida Y, Fujii K, Itasaka S, Miyamoto S, Horimatsu T, Muto M, Mizowaki T. Radiation Oncology (London, England).2018;13(1). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2023
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times