External Beam Radiotherapy for Dysphagia Palliation in Advanced Esophageal Cancer: A Prospective Study
Download
Abstract
Background and Objective: Esophageal cancer is a highly aggressive malignancy often associated with a poor prognosis due to locoregional failure and distant metastases. Approximately 60–70% of patients present at an advanced stage, with a median survival of 6-10 months and are not candidates for definitive treatment. Dysphagia is the most common symptom, affecting 80%–90% of patients. The primary goal in managing patients with advanced disease is dysphagia control, which can improve nutritional intake and quality of life. External beam radiotherapy (EBRT) is a major palliative treatment option. The primary objective of this study was to assess the efficacy of external beam radiotherapy in alleviating dysphagia in patients with esophageal cancer.
Materials and Methods: This single-arm prospective clinical study was conducted at a tertiary care hospital in Northeast India. The study included 57 esophageal cancer patients ineligible for definitive treatment. Patients received EBRT of 30 Gy in 10 fractions over two weeks. Dysphagia was graded using the Modified Takita's grading system. Patients were followed up at one-month intervals after treatment to assess dysphagia and acute toxicity.
Results: Among 57 patients in the study, subjective dysphagia relief was observed in 82.45%. The median dysphagia score decreased from 3 to 2 at the end of the 3-month post-treatment period (p < .001). In terms of treatment-related toxicity, the treatment was well-tolerated. No grade 4-5 toxicity was encountered. The most common toxicity was radiation esophagitis, affecting 15 patients (26.31%).
Conclusion: Radiation can significantly improve dysphagia in esophageal cancer patients. It is suggested as an effective, non-invasive, and well-tolerated method for treating dysphagia in selected individuals with incurable esophageal cancer.
Introduction
With a global incidence of 604,000, esophageal cancer (EC) was the seventh most common cancer worldwide and the sixth most common cause of cancer-related death (544,000 deaths) in 2020, with a male preponderance [1].
The highest geographic incidence rates for both males and females are seen in Eastern Asia.
In India esophageal cancer is the 5th most common cancer, with an incidence of around 4.8%, with the highest burden seen in the northeastern region (NER). Esophageal cancer was responsible for 10.4% (13.6% of males and 7.0% of females) of all cancers detected annually in the Northeastern states, roughly three times higher than the global and national figures [2].
It is a highly aggressive disease, and most patients present in a locally advanced state. Progressive dysphagia is the most prevalent and unpleasant symptom of locally advanced esophageal cancer, affecting 80–90% of patients. This causes weight loss, odynophagia, dyspepsia, heartburn not responding to medications, and chest pain. Furthermore, patients with locally advanced cancer or distant metastasis frequently present with growing cancer-related complications resulting in poor nutrition, worsening performance status, and decreased quality of life [3].
Almost half of locally advanced esophageal cancer patients are deemed unsuitable for curative treatment, such as surgery or definitive radiotherapy. In such scenarios, palliation became the most suitable option [4]. Patients with metastatic esophagogastric cancer are considered incurable, with the goals being symptom relief and possible survival improvement.
Non-adherence to treatment has been linked to a low survival rate for people with esophageal cancer. A study from a tertiary cancer centre in NER found that less than half of the esophageal cancer patients received cancer-directed treatment, whereas 53.4% did not receive or left therapy in the middle [2].
In such scenarios, a large number of patients are candidates for supportive care with palliative treatment primarily aimed at palliating dysphagia.
The options for dysphagia palliation include external beam radiotherapy, chemotherapy, brachytherapy, insertion of metallic stents, photodynamic therapy, or combined modalities. Numerous patient and therapy-related factors must be considered when determining the appropriate treatment method. The best treatment should give effective palliation and be administered quickly and with as few side effects as possible [5].
Radiotherapy is documented to be associated with long-term symptomatic relief of dysphagia, lower complication rates, and better quality of life (QOL) [6]. Given the substantial disease load and the number of patients with symptomatic presentations, the role of RT in dysphagia palliation becomes critical.
Moreover, studies on the impact of radiotherapy on dysphagia palliation in northeast India are scarce, and most of our tertiary care centre’s patients have advanced EC with dysphagia to liquids or semisolids. Thus, this study examined the role of palliative radiotherapy (RT) for symptomatic relief in advanced-stage EC patients, and to evaluate the acute treatment related toxicities.
Materials and Methods
This was a single-centre, prospective observational study conducted in the Radiation Oncology Department of a tertiary care hospital in North-east India. The study protocal was approved by the institutional ethics committee and written informed consent was taken from the patients before initiation.
57 patients were included in the study. They were planned for palliative EBRT as per the multidisciplinary joint tumour board and included in the study.
Inclusion criteria: All the histologically proven cases of squamous or adenocarcinoma of the esophagus who were surgically inoperable or medically unsuitable for definitive therapy, aged more than 18 years, with a symptomatic dysphagia score of 2–6 as per modified Takita’s grading, and a WHO Performance score less than or equal to 3. Exclusion criteria were; patients with tracheoesophageal fistula, patients with a previous history of radiotherapy to the mediastinum or patients with another primary cancer or with a WHO performance score of 4.
Patient evaluation and treatment
The pre-treatment patient evaluation included taking a complete history, comprehensive general physical examination, routine blood count, and chemistry profile. Upper gastrointestinal endoscopy and biopsy; CECT scan of the thorax was done. USG whole abdomen, bronchoscopy and ECG were also done. Pre-treatment dysphagia was subjectively assessed and graded per the modified Takita’s grading. Patients underwent palliative EBRT to the mediastinum to a total dose of 30 Gy in 10 fractions, once daily fraction, for five fractions a week, for a total duration of 2 weeks. Patients were treated with a 2-D technique. Pre-treatment imaging and endoscopy reports were used to aid tumour localization. Treatment fields were defined using fluoroscopic simulation. A 3 cm margin was added in the cranial-caudal direction, covering the mediastinum. Treatment was delivered using AP-PA fields with 6 MV photon, with the patient in the supine position. Patients were followed up one month after completing EBRT to assess change in dysphagia and treatment-related acute toxicity. Subsequent follow-up was done at 1-month intervals up to 3 months.
Patients’ dysphagia scores were calculated at the time of enrolment and subsequently after radiotherapy and on each follow-up visit.
Modified Takitas grading was used for grading the dysphagia:
• Grade I: able to eat normally.
• Grade II: requires liquids with meals.
• Grade III: able to take only semisolid food.
• Grade IV: able to take only liquids.
• Grade V: able to swallow saliva but not liquids.
• Grade VI: complete dysphagia
Statistical tests
The Wilcoxon signed-rank test was used to compare median dysphagia scores before and after treatment. A p-value of less than 0.05 was considered statistically significant at a 5% confidence level.
Results
Between July 2021 and June 2022 57 patients were enrolled. All of them were followed up for efficacy and toxicity evaluation. There were 30 males (52.6%) and 27 females (47.4%). The median age of the study group was 60 years (44–84 years), and the most common age group was 51–60 years (40.35%). The baseline performance score of more than half of the patients was ECOG 2 (56.14%). There was no significant difference between genders in terms of age distribution. Compared to females, a significantly greater number of males were found to be addicted to tobacco and alcohol (Table 1).
| Age (years) | Median: | ||
| 60 (44-80) | |||
| Age group (years) | Number of patients (N=57) (%) | ||
| 41-50 | 6 (10.5) | ||
| 51-60 | 23 (40.3) | ||
| 61-70 | 14 (24.6) | ||
| 71-80 | 12 (21.0) | ||
| >80 | 2 (3.5) | ||
| Sex | |||
| Female | 27 (47.4) | ||
| Male | 30 (52.6) | ||
| Performance status (ECOG) | |||
| 1 | 22 (38.6) | ||
| 2 | 32 (56.1) | ||
| 3 | 3 (5.3) | ||
| Tumor location | |||
| Cervical | 4 (7.0) | ||
| Upper thoracic | 13 (22.8) | ||
| Mid thoracic | 23 (40.3) | ||
| Lower thoracic | 17 (29.8) | ||
| Histology | |||
| WDSCC | 6 (10.5) | ||
| MDSCC | 44 (77.2) | ||
| PDSCC | 6 (10.5) | ||
| PDC | 1 (1.8) | ||
| Addiction | |||
| Males | Females | p value | |
| Tobacco | 21 (70.0) | 5 (18.15) | <0.0001 |
| Alcohol | 11 (36.66) | 1 (3.70) | 0.0023 |
The proportion of patients with a baseline (pre- treatment) dysphagia grade of I, II, III, IV, V and VI were 0, 2, 29, 21, 2 and 3% respectively, with a mean score of 3.56 (+/- 0.84) (Figure 1).
Figure 1. Comparision of Dysphagia at Each Score before and after Treatment .
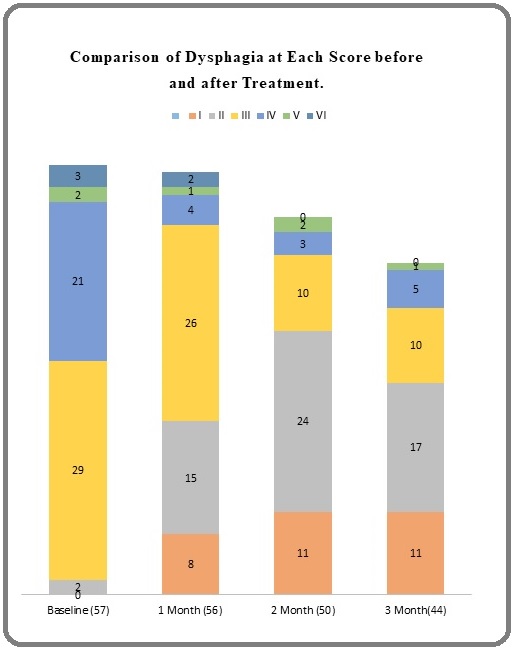
Over the study period, a significant improvement in dysphagia was noted. Significant decrease in dysphagia scores was observed between baseline and the 1st month, baseline and the 2nd month, and baseline and the 3rd month. (p<0.00001). We found that overall 47 (82.4%) patients had some dysphagia relief after treatment. Ten patients had no relief from dysphagia (Table 2).
| Baseline | Conclusion | 1 Month | 2 Month | 3 Month | |
| Median Score | 3 | 3 | 3 | 2 | 2 |
| IQR | 04-Mar | 04-Mar | 03-Feb | 03-Feb | 1.5-3 |
| Mean score | 3.56 | 3.42 | 2.67 | 2.22 | 2.27 |
| SD | 0.84 | 0.82 | 1.1 | 0.99 | 1.04 |
| 95% CI of difference of mean score | 3.56 ± 0.219 | 3.42 ± 0.213 | 2.67 ± 0.288 | 2.22 ± 0.274 | 2.27 ± 0.307 |
On subset analysis no significant difference was observed in dysphagia relief in relation to gender, age, performance status or tumor location (Table 3).
| Variable | Total patients | Dysphagia response | Response percentage (%) | p value | ||
| yes | no | |||||
| Gender | Male | 30 | 24 | 6 | 80 | 0.6 |
| Female | 27 | 23 | 4 | 85.18 | ||
| Age | 41-50 | 6 | 4 | 2 | 66.67 | 0.69 |
| 51-60 | 23 | 20 | 3 | 86.95 | ||
| 61-70 | 14 | 12 | 2 | 85.71 | ||
| 71-80 | 12 | 9 | 3 | 75 | ||
| >80 | 2 | 2 | 0 | 100 | ||
| Performance score | 1 | 22 | 20 | 2 | 90.90 | 0.32 |
| 2 | 32 | 24 | 8 | 75 | ||
| 3 | 3 | 3 | 0 | 100 | ||
| Tumour location | Cervical | 4 | 4 | 0 | 100 | 0.56 |
| Upper thoracic | 13 | 10 | 3 | 76.92 | ||
| Mid thoracic | 23 | 17 | 6 | 73.91 | ||
| Lower thoracic | 17 | 16 | 1 | 94.12 |
The treatment was overall well tolerated in terms of acute treatment-related toxicity. All of the patients were able to complete their stipulated treatment. No grade 4 or 5 toxicity was seen. The most commonly encountered toxicity was radiation esophagitis, which affected 15 patients (26.31%). Other toxicities were fatigue, nausea, and anorexia. All of them responded to conservative management.
Discussion
Dysphagia, the single most debilitating symptom of esophageal cancer, is found in 80–90% of the patients.. It results in suboptimal nutritional status and other constitutional symptoms. Therefore, the primary aim of palliative therapy is to relieve dysphagia.
In literature, only a few studies have examined the role of EBRT in palliative setting. A few retrospective studies have revealed decent results with a wide variety of radiotherapy schedules.
The principal finding of our study is that patients with advanced EC treated with short-course palliative EBRT have a significant improvement in dysphagia.
In their study, Diwan et al. gave an EBRT dose of 30 Gy over ten fractions, similar to our study (29). They found a significant decrease in mean dysphagia (p= 0.0001) following EBRT at one, two, and three months. None of their patients required a subsequent stent or feeding tube placement, and they did not find any RT-related toxicity. They also evaluated the change in QoL, and at the end of the 3rd month, they found a significant improvement in a number of QoL domains (dysphagia, eating, reflux, pain, and saliva) [7]
According to the existing literature, curative chemoradiotherapy (CRT) is superior to RT alone regarding local control and overall survival for patients with nonmetastatic, unresectable EC [8-10]. The patients our study, however, were declared unsuitable for curative CRT due to a number of patient or disease-related factors, including poor general health, medical co-morbidities, extensive locoregional disease, or distant metastases. In addition, Penniment et al. conducted a randomized trial comparing RT alone with CRT for dysphagia relief in a palliative setting. They found that 53% of patients experienced dysphagia relief, with a median response duration of 2.5 months for EBRT and 3.4 months for chemoradiotherapy. The difference was not statistically significant. (p value of 0.72); However, CRT was associated with a significantly greater incidence of grade 3-4 adverse events [11].
These findings suggest RT alone is a better approach in palliative setting.
The study by Walterbos et al. compared three EBRT schedules for symptom management in incurable esophageal cancer. They compared EBRT doses of 20 Gy (31%), 30 Gy (38%), or 39 Gy (32%) to look for any difference in dsphagia palliation, need for second intervention and overall survival (OS). 72% of the patients reported symptom relief with no variation between the schedules [12].
Some studies have compared EBRT to brachytherapy (BT) and found that EBRT yields superior results. Comparing EBRT to BT, Jeene et al. showed that 79 per cent of patients with dysphagia improved following EBRT, compared to 64 per cent with BT. In addition, more patients with dysphagia reported early initiation and peak effects of EBRT than BT at two weeks following EBRT [13].
There are several palliative treatment options for incurable carcinoma of the esophagus. Moreover, combinations of more than one treatment modality have been tried. The optimal choice of treatment strategy is influenced by many patient and treatment related factors. Some important patient related factors are, patient’s life expectancy, symptomatlogy, patient preference and anatomical considerations, such as disease extent. Key treatment related factors are anticipated toxicities, expected probability and duration of response, logistics of the available treatment option including personals and facilities at hand.
Considering all these factors treatment needs to be widely available and rapidly effective with minimal toxicity burden. In such scenarios short course of EBRT is seemingly a preferable option.
The current study had some drawbacks. First, as this was a single centre study with a small sample size, no general conclusions can be drawn. Second, a few risk variables (including alcohol and smoking) linked to EC were investigated. Thirdly, quality of life, overall survival and symptom-free survival were not assessed. Fourthly, long-term outcome of radiotherapy and its consequences could not be evaluated because of the short follow-up period. Finally, there was no quantification of residual illness at the end of the research.
In conclusion, our study showed that palliative EBRT can provide reasonable symptom control in the majority of patients with advanced carcinoma of the esophagus. Despite a lack of randomized comparison with other modalities, EBRT remains an effective, non-invasive means to palliate dysphagia in selected patients with advanced carcinoma of the esophagus. Due to the limited toxicity and the advantages in logistics, EBRT can be said to be the treatment of choice in this group of patients.
References
- Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries Sung H, Ferlay J, Siegel RL , Laversanne M, Soerjomataram I, Jemal A, Bray F. CA: a cancer journal for clinicians.2021;71(3). CrossRef
- A study of patients with oesophageal cancer in the north east india Baishya N, Kalita M, Kataki A, Krishnatreya M. BBCI EDGE.2022;3(1):1-5.
- Global cancer statistics, 2012 Torre LA , Bray F, Siegel RL , Ferlay J, Lortet-Tieulent J, Jemal A. CA: a cancer journal for clinicians.2015;65(2). CrossRef
- Interventions for dysphagia in oesophageal cancer Dai Y, Li C, Xie Y, Liu X, Zhang J, Zhou J, Pan X, Yang S. The Cochrane Database of Systematic Reviews.2014;2014(10). CrossRef
- A phase I/II study to evaluate the toxicity and efficacy of accelerated fractionation radiotherapy for the palliation of dysphagia from carcinoma of the oesophagus Kassam Z, Wong RKS , Ringash J, Ung Y, Kamra J, DeBoer G, O'Brien M, et al . Clinical Oncology (Royal College of Radiologists (Great Britain)).2008;20(1). CrossRef
- Palliation of Dysphagia in Carcinoma Esophagus Ramakrishnaiah VPN , Malage S, Sreenath GS , Kotlapati S, Cyriac S. Clinical Medicine Insights. Gastroenterology.2016;9. CrossRef
- Palliative radiotherapy and quality of life in patients with locally advanced thoracic esophageal cancer: a single centre experience from Central India Bandhate K, Diwan A. Reports of Practical Oncology and Radiotherapy: Journal of Greatpoland Cancer Center in Poznan and Polish Society of Radiation Oncology.2022;27(1). CrossRef
- Progress report of combined chemoradiotherapy versus radiotherapy alone in patients with esophageal cancer: an intergroup study Sarraf M, Martz K, Herskovic A, Leichman L, Brindle JS , Vaitkevicius VK , Cooper J, Byhardt R, Davis L, Emami B. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.1997;15(1). CrossRef
- Combined chemoradiotherapy vs. radiotherapy alone for early stage squamous cell carcinoma of the esophagus: a study of the Eastern Cooperative Oncology Group Smith TJ , Ryan LM , Douglass HO , Haller DG , Dayal Y, Kirkwood J, Tormey DC , et al . International Journal of Radiation Oncology, Biology, Physics.1998;42(2). CrossRef
- Combined chemotherapy and radiotherapy compared with radiotherapy alone in patients with cancer of the esophagus Herskovic A, Martz K, Sarraf M, Leichman L, Brindle J, Vaitkevicius V, Cooper J, Byhardt R, Davis L, Emami B. The New England Journal of Medicine.1992;326(24). CrossRef
- Palliative chemoradiotherapy versus radiotherapy alone for dysphagia in advanced oesophageal cancer: a multicentre randomised controlled trial (TROG 03.01) Penniment MG , De Ieso PB , Harvey JA , Stephens S, Au HJ , O'Callaghan CJ , Kneebone A, et al . The Lancet. Gastroenterology & Hepatology.2018;3(2). CrossRef
- Effectiveness of several external beam radiotherapy schedules for palliation of esophageal cancer Walterbos NR , Fiocco M, Neelis KJ , Linden YM , Langers AMJ , Slingerland M, Steur WO , Peters FP , Lips IM . Clinical and Translational Radiation Oncology.2019;17. CrossRef
- Short-Course External Beam Radiotherapy Versus Brachytherapy for Palliation of Dysphagia in Esophageal Cancer: A Matched Comparison of Two Prospective Trials Jeene PM , Vermeulen BD , Rozema T, Braam PM , Lips I, Muller K, Kampen D, et al . Journal of Thoracic Oncology: Official Publication of the International Association for the Study of Lung Cancer.2020;15(8). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2023
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times