Malignant Tumor of the Mandible – Secondary Leading to Primary: A Case Report with the Review of the Literature
Download
Abstract
Metastatic adenocarcinoma of jaw-bone accounts for 1-3% and is commonly seen in the fifth and sixth decades. Most metastases of the oral cavity from primary locations have been described in the lungs, breasts, kidneys, and colon in adult patients. Oral Clinicians apart from diagnosing systemic diseases like diabetes, gastrointestinal disorders etc, could be the first ones to diagnose malignancies of different parts of the body before any oncologist and general physicians. Specialized imaging like PET/CT aids in diagnosing the primary tumor in such cases. To increase the survival time of such patients extensive mandibulectomy followed by other multimodal treatment options like palliative care should be considered. Here, in this paper, we aim to present a case of a young 24-year- old female with a metastatic tumor of the mandible that ultimately gave us the roadmap for diagnosing the primary tumor of the breast and also to review the literature of such cases.
Introduction
Metastases in the oral cavity are rare and account for only 1 to 3% of all malignant lesions in this area. The primary locations from which more metastases have been described in the oral cavity are the lungs (30.6% ), breasts (22.2% ), liver (15.5%), prostate (9 % or), thyroid glands (8.1% ), kidneys (7.3% ), skin (2.3% ), soft tissues (2%), colon (2% ) and gastrointestinal (0.6%) [1]. Nearly, 90% of metastatic tumors occur in jaw bones, especially the premolar-molar region of the mandible, whereas metastases to soft tissues are extraordinarily rare and account for 0.1% of all oral malignancies [2]. The primary site differs according to oral site colonization. In men, the primary tumor of the lung followed by the prostate gland and kidney commonly affects both the jawbones and oral mucosa. In women, the breast is the most common primary tumor site affecting the jawbones and soft tissues (41% and 24.3%, respectively), followed by the adrenal and female genital organs. In the jawbones, most patients complain of swelling, pain, and paraesthesia which developed in a relatively short period [3]. Through this case report we wish to highlight Although metastases in the oral cavity are an uncommon pathology, early diagnosis is needed so that in the event that it is the first manifestation, it allows the primary tumor to be diagnosed as soon as possible.
Case Report
A 24-year-old female patient reported to the department of Oral Medicine and Radiology with a complaint of pain and swelling in her left lower back tooth region for 6 months. The size of the swelling progressively increased to the present size which was approximately 1.5x1cm anteroposteriorly and mesiodistally in its greatest dimension. Intraoral examination showed a diffuse swelling located on the facial and lingual interdental papillae of teeth 34 and 35. The surface of the swelling was smooth reddish pink in color with no signs of pus discharge (Figure 1).
Figure 1. Intraoral Firm Swelling in the Interdental Region of [34,35].

On palpation swelling was firm in consistency with the rise in temperature and tender, bleeding on probing was absent. The patient’s medical history was insignificant.
An intraoral periapical radiograph showed rarefaction in the interdental region of 34 & 35 with loss of lamina dura at the distal aspect of 34 and mesial aspect of 35 and displacement of teeth. Further, CBCT examination revealed an ill-defined osteolytic lesion with ragged and irregular margins and a cupping defect at the level of cervical thirds of the alveolus in the sagittal section (Figure 2A) with effacement of buccal and lingual cortical plates in the axial section (Figure 2B).
Figure 2. A, Sagital Section in CBCT; B, Axial Section in CBCT.

Based on history, clinical and radiographic examination differential diagnosis of Peripheral/Central Giant cell lesion, primary intra-osseous carcinoma of odontogenic origin.
An Incisional biopsy was done and multiple soft and hard tissue specimens were sent for microscopic examination. Histopathological examination was consistent with the features of malignant neoplasm possibly adenocarcinoma. Adenocarcinoma arising centrally within the mandible, or metastatic adenocarcinoma is probable in this region. To rule out metastatic adenocarcinoma a whole-body PET San (positron Emission tomography) was done. The PET scan showed an increased FDG (fluorodeoxyglucose) in various parts of the body like the right breast and liver. The scan also showed multiple nodal metastases including paratracheal, para-pre aortic, and inguinal lymph nodes. The lesion in the upper outer quadrant of the right breast showed the highest uptake on the scan (Figure 3).
Figure 3. FDG Avid Enhancing Lesion is Seen in the Upper Outer Quadrant of the Right Breast (1.6cm x 1.6cm, SUV max: 6.4)..
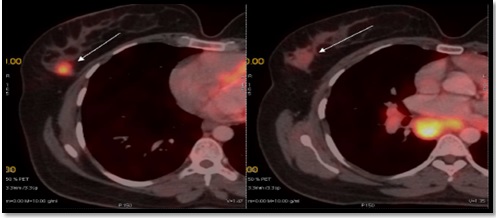
Soft tissue density lesion was seen along the body of the mandible on the left side causing erosions (Figure 4).
Figure 4. FDG Avid Irregular Soft Tissue Density Lesion (2.0cm x 1.5cm, SUV max: 5.6) Causing Erosions is Seen along the Body of Mandible on Left Side. It is involving the underlying buccal mucosa. Medially, it is abutting the left lateral border of tongue.
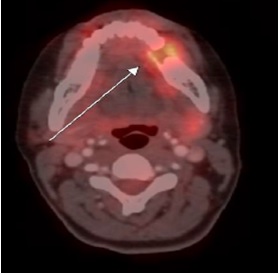
Correlating the PET scan and other investigations a final diagnosis of adenocarcinoma of the right breast with the metastatic lesion to the mandible and other body parts were made.
Discussion
Adenocarcinoma is a malignant neoplasm of epithelial cells of the glands. According to the literature, studies from a variety of primary tumors revealed the most common histological type of mandibular bone metastases was adenocarcinoma which is in agreement with the data from our report [4]. Adenocarcinomas also make up 70 percent of cancer of unknown origin [5]. Tumour progression depends upon the formation of new blood vessels (angiogenesis) and revascularization which are a prerequisite for tumor outgrowth. Because of rich network capillaries, malignant cells are easily entrapped in the oral soft tissues. The proliferating capillaries show uneven basement membrane and thus tumour cells can penetrate more easily [6]. Hirschberg et al suggested that inflammation plays an important role in attracting metastatic cells to the gingiva [7]. In total, <1% of mandibular malignancies are metastatic lesions of a primary tumor originating in another region of the body. The metastases from primary cancers are more often to the long bones, vertebrae and ribs but metastasis may also occur in oral soft tissues, jawbones, or both which are rare as consistent with our case. Soft tissue metastasis may erode the underlying bone, whereas bone metastasis may extend into the overlying soft tissues Therefore, in many instances determining the primary site of involvement may prove difficult. In the current sample, the epicentre of the metastatic deposit appeared to be within the bone. According to Zhen Cai et al, patients with oral and maxillofacial region metastasis were diagnosed in their fifth to seventh decades and are mostly located in the mandible in 80-90% of cases, with the molar region being the most frequently involved site, followed by premolar region angle-ramus, condyle and least common being coronoid process [8]. The current case is unique as the patient’s age was 25 years old, had a female predominance and metastases were located in the premolar region. Commonly, metastases to the jaws often have vague or innocuous symptoms. In our study, the most common jaw symptom was pain and swelling. Hashimoto et al. postulated that these are favorable sites for early metastasis due to the presence of hematopoietic cells in normal adults. These hematopoietically active sites may serve as a favorable niche attracting metastatic tumour cells. Only in the advanced stages of the disease did tumour cells appear in the anterior part of the mandibular body. In contrast, the adult maxilla lacks active hemopoiesis, which may result in tumours metastasising to the mandible much more frequently. The identification of oral and maxillofacial metastasis on routine radiographic examination, particularly in the early stages, may be difficult. It has been reported in the literature that in a significant number of cases, no apparent radiological change could be visualised in histologically confirmed jawbone metastases. In contrast, poorly demarcated lesions generally suggest an infectious or malignant neoplastic process [9]. In the majority of cases, metastatic lesions follow the status quo and present with poorly demarcated, osteolytic changes and radiological signs of destruction. This includes root resorption, cortical destruction and soft tissue infiltration as concurrent with the current sample. The radiographic density of metastatic tumours to bone is dependent on the nature or origin of the primary tumour, and whether the malignant cells secrete osteoblast or osteoclast-stimulating factors. In approximately 18% of cases, metastasis can present with increased radio density, frequently arising from prostatic or breast origin. In the current sample, metastases from breast origin presented as either an osteolytic or osteogenic lesion. CBCT imaging is also advantageous in illustrating minor bony changes when compared to panoramic radiography, CBCT revealed an ill-defined osteolytic lesion with ragged and irregular margins with perforation, thinning and effacement of the buccal and lingual cortical plates with cupping defect noted. Imaging modalities are unable to view soft tissue involvement and extension. Adjunct special investigations of suspicious lesions are important, as metastasis to the oral and maxillofacial region can be the first sign of a primary malignant tumour. PET/CT imagining has higher sensitivity and specificity to detect bony changes, compared with CT and MRI. Additionally, a PET/CT scan can detect 30% of primary tumours missed by conventional imaging, and therefore is recommended for metastatic lesions of the unknown primary site. Jaw metastasis is indicative of advanced disease and is associated with a poor prognosis, where a significant number of patients succumb to the disease within a year [10]. This young female patient underwent PET Scan and came out with the presence of a widespread tumour and oral metastatic disease which gives the patient a grave prognosis as the mean survival rate from the appearance of the lesion was 4 months.
In conclusion, despite poor prognosis and low survival rate of patients with metastatic adenocarcinoma of the oral cavity early diagnosis and specialized imaging like PET/CT can help patients to detect the primary tumour. Even segmental mandibulectomy, supportive therapies and palliative care can also extend the survival time of such patients.
References
- Incidence rate of metastases in the oral cavity: a review of all metastatic lesions in the oral cavity Oliver-Puigdomènech C, González-Navarro B, Polis-Yanes C, Estrugo-Devesa A, Jané-Salas E, López-López J. Medicina Oral, Patología Oral y Cirugía Bucal.2021;26(5). CrossRef
- Metastatic oral soft-tissue lesions: An incidental finding in four cases Akheel M, Tomar SS , Hussain SMDJ . South Asian Journal of Cancer.2013;2(3). CrossRef
- Metastatic tumours to the oral cavity – Pathogenesis and analysis of 673 cases Hirshberg A, Shnaiderman-Shapiro A, Kaplan I, Berger R. Oral Oncology.2008;44(8). CrossRef
- Metastatic tumors in the jaw bones: A retrospective clinicopathological study of 12 cases at Tertiary Cancer Center Nawale K, Vyas M, Kane S, Patil A. Journal of Oral and Maxillofacial Pathology.2016;20. CrossRef
- Adenocarcinoma. [Updated 2022 Sep 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan Mullangi S, Lekkala MR. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562137/..
- Metastatic tumors to the jaws and oral cavity Kumar GS , Manjunatha BS . Journal of Oral and Maxillofacial Pathology : JOMFP.2013;17(1). CrossRef
- Metastases to the oral mucosa: analysis of 157 cases Hirshberg A, Leibovich P, Buchner A. Journal of Oral Pathology & Medicine: Official Publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology.1993;22(9). CrossRef
- A retrospective study of six patients with mandibular metastatic carcinoma Cai Z, Zhu C, Wang L, Zhu L, Zhang Z, Zhu H, Wang Y. Oncology Letters.2016;11(6). CrossRef
- Pathological characteristics of metastatic carcinoma in the human mandible Hashimoto N, Kurihara K, Yamasaki H, Ohba S, Sakai H, Yoshida S. Journal of Oral Pathology.1987;16(7). CrossRef
- Radiological spectrum of metastasis to the oral and maxillofacial region Nel C, Uys A, Robinson L, Nortjé CJ . Oral Radiology.2022;38(1). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2023
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times