Radical Radiotherapy for Primary Extranodal Lymphoma of the Tonsil: A Case Report
Download
Abstract
Primary non-Hodgkin’s lymphoma (NHL) typically arises within lymph nodes, but 20-30% of cases involve extranodal sites. NHL of Waldeyer’s ring is uncommon, with the palatine tonsils being the most frequently affected site. Diffuse large B-cell lymphoma (DLBCL) is the most common high-grade, rapidly growing NHL, accounting for approximately 80% of cases in some studies. For aggressive, localized extranodal lymphoma, systemic therapy is the primary treatment modality unless patients are unfit or decline such treatment. This case report describes a 71-year-old man who presented with left tonsillar swelling, dysphagia, and voice change for 10 days. He was diagnosed with localized primary extranodal NHL - DLBCL of the left tonsil. Due to his advanced age and multiple comorbidities, he was deemed unfit for chemotherapy. He received radical radiotherapy as the primary treatment. During treatment, he experienced symptom relief and responded well to the radiation therapy. He is currently under regular follow-up.
Introduction
The malignant lymphomas are neoplastic transformations of cells that reside predominantly in lymphoid tissue. Primary non-Hodgkin’s lymphoma (NHL) usually arises within the lymphnodes, but 20-30% account for extranodal sites [1,2]. The Extranodal Lymphoma’s are defined as lymphomas arising in an extranodal organ or tissue. Overall, approximately one third of non-Hodgkin lymphomas (NHL) present in an extranodal site [3]. Non-Hodgkin’s lymphoma (NHL) of the Waldeyer’s ring is a clinical rarity. Among these tumors, palatine tonsils are most frequently involved. NHL of primary extranodal type involving the oral cavity as well as oropharynx amounts to 13% with almost 70% fraction occurring in the tonsils [4]. Most common high-grade rapidly growing NHL is diffuse large B-cell lymphoma (DLBCL), reaching about 80% in some of the studies [4,5]. For aggressive localized ENL, systemic therapy is the primary treatment modality unless patients are unfit for, or refuse, such therapy. For patients unsuitable for aggressive salvage chemotherapy, or who have residual, relapsed, or progressive disease after such therapy, a dose of 45 to 55 Gy may be required to provide acceptable rates of local disease control [6]. Here, we report a rare case of localized Primary Extra nodal NHL - DLBCL of left tonsil, unfit for chemotherapy treated by radical radiotherapy.
Case report
A 71 years old gentleman came with complaints of swelling in the left tonsillar fossa since 10 days, which was sudden in onset, associated with difficulty while swallowing food, and change in voice since 5 days. There was no history of weight loss, night sweats, or prolonged fever. The patient had multiple comorbidities like Diabetes Mellitus, hypertension, chronic atrial fibrillation, COPD & history of CVA – stroke with left hemiplegia, prostatomegaly with prostatism. On ENT examination, there was a swelling in left tonsillar fossa approximately measuring 4 x 3 cm (Figure 1).
Figure 1. Clinical Picture Showing Left Tonsillar Swelling..

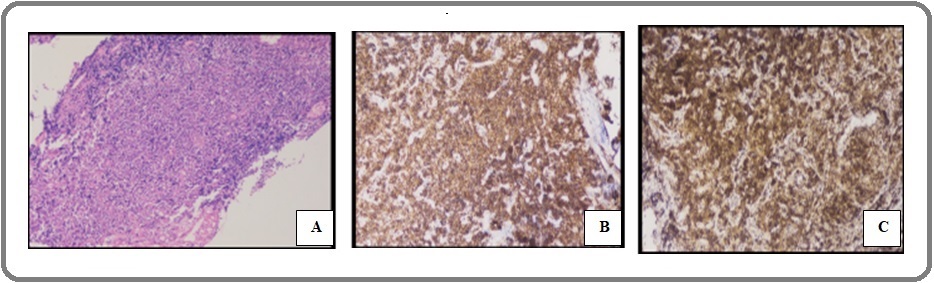
There was also left level II lymph node palpable approximately measuring 1x 1 cm which was hard, mobile and non tender. Biopsy from left tonsillar mass showed as lymphoproliferative lesion with possibility of lymphoma. On IHC – the atypical cells were positive for CD 20, BCL2, CD10, BCL6 , CD5, MUM 1 & cMYC while being negative for CD3 & p40, Ki 67 – 90%: Suggestive of Diffuse large B cell lymphoma – germinal centre type (Figure 2).
Figure 2. Showing Histopathology as DLBCL, A) H and E stain, B) IHC – CD 20 Positive and C) IHC – BCL2 Positive.

FDG PET CT scan showed as FDG avid soft tissue mass lesion is noted involving left para-oropharyngeal / tonsillar region measuring 3.1 x 3.8 x 6.2 cm with SUV max 10.7 & FDG avid left cervical level II lymph node measuring 1.05 x 0.6 x 1.4 cm with SUV max 4.9 (Figure 3).
Figure 3. Axial Section of FDG Avid Lesion in Left Tonsillar Region and Level II Lymph Node.
No evidence of metabolic active disease in rest of the body. Bone marrow aspiration & biopsy showed no evidence of infiltrative disorder. Serum LDH was 129 U/L. Hence he was diagnosed as Primary Extra nodal NHL - localized DLBCL of left tonsil stage II E. He was very high risk candidate for chemotherapy with respect to elderly age, multiple comorbidities, history of covid pneumonia with lung damage in CT scan, Ki 67 – 90% so high possibility of tumor lysis syndrome; hence he was considered for radical radiotherapy with the consent of patient & their attenders. He received external beam radiotherapy with 6 MV photon using Tomotherapy (Helical IGRT) technique with Radixact X9 machine to a dose of 50.4 Gy in 28 fractions @ 1.8 Gy per fraction, 5 days a week from Monday to Friday. During the treatment he had symptomatic relief. He tolerated the treatment well. He responded to the radical radiotherapy well & now he is on regular follow up.
Discussion
Malignant lymphomas in majority of the cases arise from lymph nodes. However, 24–48% of them arise in extranodal sites [4]. Non-Hodgkin’s lymphomas (NHL) are a heterogeneous group of lymphoproliferative disorders originating in B-lymphocytes, T-lymphocytes or natural killer (NK) lymphocytes. Guevara-Canales et al. reviewed 215 articles to conclude that Waldeyer’s ring along with gingiva was the most commonly affected site with palatine tonsil being the most common [5]. It is usually unilateral and may involve ipsilateral regional lymph nodes (stage II). Primary tonsillar lymphoma occurs in <1% of all head & neck malignancies. The lymphoma has peaks in the 6th and 7th decades of life and the incidence is male predominant [5]. The nonspecific clinical signs and symptoms include but are not limited to fullness in the throat, sore throat, pain or difficulty in swallowing, earache, cervical lymphadenopathy, swelling in tonsils, or snoring. Advanced disease may also show fever, weight loss, and night sweats, albeit rare. Mild-to-moderate tonsillar enlargement on clinical presentation can easily be misdiagnosed for tonsillitis when it is the only presenting feature in this cohort of cases [7].
The etiology of diffuse large B-cell lymphoma remains unknown. They may originate de novo or with underlying immunodeficiencies which is a significant risk factor [8]. No evidence of immunodeficiency state was found in our patient, his HIV was non reactive.
Most tonsillar lymphomas published are that of B-cell type, and the most common histologic type has been reported to be DLBCL. Diagnosis of lymphoma is based on the histopathology result. Immunohistochemical staining in biopsy material allows to differentiate forms of lymphoma. Disease staging is completed with imaging evaluation. Positron emission tomography completes the CT evaluation as it provides metabolic activity information [9]. MRI is useful to evaluate the skull base, cranial cavity, cranial nerve infiltration, sinuses, and infratemporal fossa. All baseline investigations like complete blood counts along with bone marrow biopsy are equally mandatory.
Castillo et al found that primary extranodal sites of disease were associated with good prognosis in patients with DLBCL in the rituximab era and reported that, based on multivariate analysis, the head and neck region was the site of involvement associated with a better survival (HR 0.79, 95% CI 0.70–0.89; P<0.001 % compared to gastrointestinal, pulmonary, and liver/pancreas localization [10].
For aggressive localized ENL, systemic therapy is the primary treatment modality unless patients are unfit for, or refuse, such therapy. As is the case with nodal aggressive NHL, RT is often used to consolidate the results of systemic therapy, and it reduces the risk of local failure, potentially translating into an improvement in progression-free and overall survival [6]. In our case, the patient was unfit for systemic therapy in view of elderly age & multiple comorbidities, hence was considered for radical radiotherapy .
For radiation treatment, preplanning PET/CT scans are recommended. For patients with aggressive lymphomas, prechemotherapy images should be available, and for lymphomas close to the skull base, MRI scans are important for detecting possible intracranial extension. CTV is determined by the prechemotherapy GTV, but often the entire involved structure (e.g the whole tonsillar fossa from the level of the soft palate to the level of the vallecula) is included because of uncertainty about the exact extent of initial involvement. Uninvolved structures are not included in the CTV, and neck nodes are treated only if involved. PTV margin depends on immobilization; with optimal fixation it is normally 4 to 5 mm [6].
For diffuse large B-cell lymphoma (DLBCL) and peripheral T-cell lymphoma (PTCL) involving extranodal sites, 30 to 36 Gy is an appropriate dose after a complete response (CR) to first-line chemotherapy. A dose of 30 to 36 Gy is also appropriate for patients who have had a CR to salvage chemotherapy for relapsed or refractory disease [11]. Patients with gross residual disease benefit from a higher dose (40-45 Gy) [12]. For patients unsuitable for aggressive salvage chemotherapy, or who have residual, relapsed, or progressive disease after such therapy, a dose of 45 to 55 Gy may be required to provide acceptable rates of local disease control [6]. Our patient received external beam radiotherapy with 6 MV photon using Tomotherapy (Helical IGRT) technique with Radixact X9 machine to a dose of 50.4 Gy in 28 fractions @ 1.8 Gy per fraction, 5 days a week from Monday to Friday with radical intent. During the treatment he had symptomatic relief. He responded to the radical radiotherapy well & now is on regular follow up.
In conclusion, primary lymphoma of the tonsil is a rare entity but common in extra nodal lymphoma. Diffuse large B-cell lymphoma is the most commonly found histological subtype. For aggressive lymphoma, systemic therapy followed by radiotherapy is the standard treatment. Radical radiotherapy can be considered the treatment option in primary extra nodal localized tonsillar DLBCL in the patient who are unfit for chemotherapy or refuse for it.
References
- Extranodal malignant lymphomas of the head and neck Clark RM , Fitzpatrick PJ , Gospodarowicz MK . The Journal of Otolaryngology.1983;12(4).
- Lymphoma: an unusual oral presentation Spatafore CM , Keyes G, Skidmore AE . Journal of Endodontics.1989;15(9). CrossRef
- The epidemiology of non-Hodgkin's lymphoma: comparison of nodal and extra-nodal sites Newton R, Ferlay J, Beral V, Devesa SS . International Journal of Cancer.1997;72(6). CrossRef
- Primary diffuse large B-cell lymphoma of the tonsil: is a higher radiotherapy dose required? Laskar S, Bahl G, Muckaden MA , Nair R, Gupta S, Bakshi A, Gujral S, Shet T, Shrivastava SK , Dinshaw KA . Cancer.2007;110(4). CrossRef
- Systematic review of lymphoma in oral cavity and maxillofacial region Guevara-Canales JO , Morales-Vadillo R, Faria PEA , Sacsaquispe-Contreras SJ , Leite FPP , Chaves MGAM . Acta odontologica latinoamericana: AOL.2011;24(3).
- Modern radiation therapy for extranodal lymphomas: field and dose guidelines from the International Lymphoma Radiation Oncology Group Yahalom J, Illidge T, Specht L, Hoppe RT , Li Y, Tsang R, Wirth A. International Journal of Radiation Oncology, Biology, Physics.2015;92(1). CrossRef
- Diffuse large B-cell lymphoma arising de novo in unilateral tonsil Hemalatha AL , Sushma HM , Indira CS , et al . National J Lab Med.2014;3(4):12-14. CrossRef
- Tanos de Lacerda JC, Mesquita RA. Plasmablastic lymphoma of oral mucosa type: A case report Barroso Duarte EC , da Silveira-Júnior JB , Gomez RS , Pinto Paes RA . Oral Oncol Extra [Internet].2005;41(6):121-124. CrossRef
- Malignant lymphoma of the head and neck Zapater E E, Bagán JV , Carbonell F, Basterra J. Oral Diseases.2010;16(2). CrossRef
- Sites of extranodal involvement are prognostic in patients with diffuse large B-cell lymphoma in the rituximab era: an analysis of the Surveillance, Epidemiology and End Results database Castillo JJ , Winer ES , Olszewski AJ . American Journal of Hematology.2014;89(3). CrossRef
- Reduced dose radiotherapy for local control in non-Hodgkin lymphoma: a randomised phase III trial Lowry L, Smith P, Qian W, Falk S, Benstead K, Illidge T, Linch D, et al . Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2011;100(1). CrossRef
- Involved-field radiotherapy before high-dose therapy and autologous stem-cell rescue in diffuse large-cell lymphoma: long-term disease control and toxicity Hoppe BS , Moskowitz CH , Filippa DA , Moskowitz CS , Kewalramani T, Zelenetz AD , Yahalom J. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2008;26(11). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2024
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times