Extraskeletal Osteosarcoma Misdiagnosed as Chondroma: A Case Report
Download
Abstract
Extraskeletal osteosarcoma is a rare malignant chondro-osseous neoplasm that arises outside the skeletal system. It accounts for less than 1% of all soft tissue sarcomas. We report a case of a 60-year-old male who presented with an isolated, primary subcutaneous tumor on the dorsal aspect of his left foot. Radiological imaging initially suggested an extraskeletal chondroma. However, following surgical excision and pathological analysis, the diagnosis of extraskeletal osteosarcoma was confirmed. This report describes the clinical and pathological findings of extraskeletal osteosarcoma in this case.
Introduction
Extraskeletal osteosarcoma (ESOS) is a malignant chondro-osseous neoplasia that is not associated with the skeletal system. It is characterized by bone matrix or osteoid formation. It may contain osteoblastic component as well as chondroblastic and fibroblastic components. Although extraskeletal osteosarcoma is histologically similar to primary osteosarcoma of bone; there are significant differences between them in terms of demographic characteristics, imaging characteristics, and prognosis [1].
It was first described in 1941 [2]. Although most of these tumors are located in the deep soft tissue, they can sometimes be localized in the dermis or subcutaneous tissue. When the literature is examined, it has been seen that there are ESOS cases reported in many different localizations such as vesicle seminalis, lymph node, mediastinum, and orbit [3-9].
Case Report
A 60-year-old male patient presented to our hospital due to swelling in the dorsal aspect of his left foot. The patient had a history of diabetes and hypertension. Contrast-enhanced magnetic resonance imaging revealed a 36x21 mm sized, largely calcified, well-circumscribed lesion with peripheral enhancement in post-contrast series in the subcutaneous fat tissue in the dorsal part of the foot at the level of the 2nd metatarsal bone. The described lesion did not appear to invade the extensor tendon or bone structure. The lesion was initially considered an extraskeletal chondroma radiologically (Figure 1A).
Figure 1. Extraskeletal Osteosarcoma. Figure 1A, MRI showing a well-circumscribed lesion in the dorsal part of the foot. Figure 1B, 1C, Low-magnification (×100) photomicrograph with hematoxylin-eosin stain demonstrating chondroid matrix and dense sheets of osteoid. Figure 1D, Low-magnification (×100) photomicrograph with hematoxylin-eosin stain demonstrating fibroblastic differentiation with severe cytological atypia.
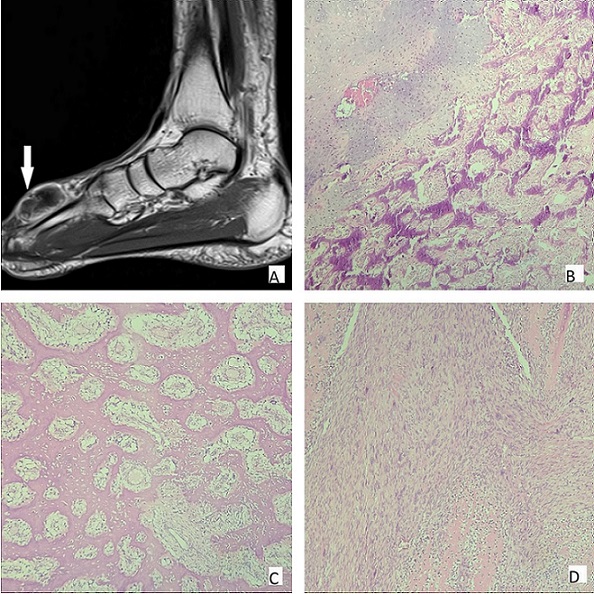
A piece of nodular tissue, 3.8x3.5x1.8 cm, gray-white in color, and bone-hard, was sent to our department. Sampling was done after decalcification. Spindle and polygonal shaped bizarre tumor cells forming widespread neoplastic bone matrix were observed in tissue samples. In addition to osteoblastic differentiation, areas of chondroblastic and fibroblastic differentiation were also present in the tumor (Figure 1B-1D). As a result of the large immunohistochemical panel applied, tumor cells were positive with CD99, bcl-2; focal positive with SMA (smooth muscle actin), desmin, S100, p63; EMA (epithelial membrane antigen) showed negative immune reaction with panCK, CD34. Aberrant staining was observed with p53. 71 mitoses were counted in 10 high-magnification fields. Ki-67 proliferation index was 80%. Malignant neoplasms such as extraskeletal osteosarcoma, mesenchymal chondrosarcoma, synovial sarcoma, and undifferentiated pleomorphic sarcoma were included in the differential diagnosis. As the mass was extraskeletal and showed extensive osteoblastic differentiation, the case was found to be compatible with ESOS. Additional resection was performed because of the positive surgical margins. Adjuvant radiochemotherapy was given after surgery.
Discussion
ESOS accounts for less than 1% of all soft tissue sarcomas and occurs mainly in the middle-aged. Most cases develop de novo, in some cases, radiation exposure is a predisposition factor [10]. Due to their rarity, the diagnosis and treatment of ESOS remain controversial.
On radiographs, extraskeletal osteosarcoma is often seen as a soft tissue mass with variable amounts of mineralization. Osteoid matrix formation or calcification is seen in approximately half of the lesions. An increase can be observed over time. Matrix mineralization is best evaluated on computed tomography (CT) rather than radiography or magnetic resonance imaging (MRI). On MRI, the tumor is usually a well-circumscribed heterogeneous mass and isointense to skeletal muscle on T1- and T2-weighted images [1].
ESOS is the soft tissue equivalent of osteosarcoma in bone. Morphologically, it can appear in many different forms. Tumors usually consist of epitheloid, spindle, or polygonal cells with pleo-morphism and cytological atypia. Osteoblastic, chondroblastic, and fibroblastic differentiation areas can be seen at different rates [10]. The neoplastic bone may grow in lace-like, trabecular, or sheet-like patterns. Tumor necrosis is common. The Special AT-rich sequence-binding protein 2 (SATB2) immunohistochemical stain can be used to detect osteoblastic differentiation [11]. But not specific for osteosarcoma. Osteoid production can also be seen in some non-ESOS high-grade soft tissue sarcomas like dedifferentiated liposarcoma, and undifferentiated pleomorphic sarcoma [12,13]. Bone-forming reactive lesions such as myositis ossificans should also be considered in the differential diagnosis. This may cause difficulties in reaching the correct diagnosis. Focal staining in immunohistochemical studies may also cause confusion. Staining with varying intensity and nonspecificity can be seen with immunohistochemical studies such as SMA, CD99, EMA, and desmin. Although histopathological evaluation is the gold standard for the diagnosis of ESOS, correlation with radiological findings is essential for a definitive diagnosis.
Although there is no standard treatment protocol for ESOS, the cornerstone of treatment is radi-cal surgery and polychemotherapy. Due to the rare nature of this disease, data on the type of chemotherapeutic combinations are not available. There are studies with positive results when treated like traditional osteosarcomas [14]. Adjuvant radiotherapy may be considered in the case of the unresectable or incompletely resected primary tumor [15]. In conclusions, ESOS is a rare malignant mesenchymal neoplasia with few reports in the literature. Radiological findings may be nonspecific. It should be considered in the differential diagnosis when non-skeletal tumors with osteoblastic differentiation are encountered. Since they differ from osteosarcomas of the bone in terms of treatment and prognosis, it is important for disease management to reach the diagnosis by correlation of histological and radiological findings.
References
- Extraskeletal osteosarcoma: spectrum of imaging findings Mc Auley G, Jagannathan J, O'Regan K, Krajewski KM , Hornick JL , Butrynski J, Ramaiya N. AJR. American journal of roentgenology.2012;198(1). CrossRef
- Extraskeletal Ossifying Tumors Wilson H. Annals of Surgery.1941;113(1). CrossRef
- Primary extraskeletal osteosarcoma of the seminal vesicle: a case report and literature review Choi JD , La Choi Y, Kim HS , Seo SI , Jeon SS , Lee HM , Jeong BC . Annals of the Royal College of Surgeons of England.2011;93(4). CrossRef
- Extraskeletal osteosarcoma arising in anterior mediastinum: brief report with a review of the literature Hishida T, Yoshida J, Nishimura M, Ishii G, Nakao M, Nagai K. Journal of Thoracic Oncology: Official Publication of the International Association for the Study of Lung Cancer.2009;4(7). CrossRef
- Extraskeletal osteosarcoma of the pleura:report of a case Shiota H, Yasukawa T, Hirai A, Chiyo M, Yusa T, Hiroshima K. Annals of Thoracic and Cardiovascular Surgery: Official Journal of the Association of Thoracic and Cardiovascular Surgeons of Asia.2013;19(4). CrossRef
- Extraskeletal Osteosarcoma of the Hand Dunbar RM , Sumarriva GE , Duncan SFM , Reith JD , Meyer MS . The Journal of Hand Surgery.2018;43(5). CrossRef
- Extraskeletal osteosarcoma of the orbit: A clinicopathologic case report and review of literature Maeyer VMDS , Kestelyn PAFA , Shah AD , Van Den Broecke CM , Denys HGN , Decock CE . Indian Journal of Ophthalmology.2016;64(9). CrossRef
- [Extraskeletal osteosarcoma in lymph nodes: a case report] Jian W, Zhang YH , Zhang Y, Li RQ . Zhonghua Zhong Liu Za Zhi [Chinese Journal of Oncology].2021;43(6). CrossRef
- Subcutaneous extraskeletal osteosarcoma of the forearm: a case report and review of the literature Healy C, Kahn LB , Kenan S. Skeletal Radiology.2016;45(9). CrossRef
- Extraskeletal osteosarcoma Chung EB , Enzinger FM . Cancer.1987;60(5). CrossRef
- Primary extraskeletal osteosarcoma: a clinicopathological study of 18 cases focusing on MDM2 amplification status Yamashita K, Kohashi K, Yamada Y, Nishida Y, Urakawa H, Oda Y, Toyokuni S. Human Pathology.2017;63. CrossRef
- Nuclear imaging of an extraskeletal retroperitoneal osteosarcoma: respective contribution of 18FDG-PET and (99m)Tc oxidronate (2005:1b) Hamdan A, Toman J, Taylor S, Keller A. European Radiology.2005;15(4). CrossRef
- Retroperitoneal extraskeletal osteosarcoma: imaging findings and transarterial chemoembolization Zhang HJ , Yang JJ , Lu JP , Sheng J, Yuan M, Jiang X, Li YX , Gupta S. Cardiovascular and Interventional Radiology.2010;33(2). CrossRef
- Extraskeletal osteosarcoma has a favourable prognosis when treated like conventional osteosarcoma Goldstein-Jackson SY , Gosheger G, Delling G, Berdel WE , Exner GU , Jundt G, Machatschek JN , et al . Journal of Cancer Research and Clinical Oncology.2005;131(8). CrossRef
- Radiotherapy for local control of osteosarcoma DeLaney TF , Park L, Goldberg SI , Hug EB , Liebsch NJ , Munzenrider JE , Suit HD . International Journal of Radiation Oncology, Biology, Physics.2005;61(2). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2024
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times