Management of Synchronous Locally Advanced Oropharyngeal Carcinoma and Early-Stage Esophageal Carcinoma in a Tertiary Cancer Center: A Case Report
Download
Abstract
Background: Risk factors for squamous cell carcinomas (SCCs) of the head and neck (HN) and esophagus are similar, making synchronous primary tumors in these areas not entirely uncommon. Definitive chemoradiation (CRT) is the standard of care for locally advanced HNSCC and is a preferred option for inoperable esophageal SCC. Simultaneous treatment of both primaries with CRT can present technical challenges.
Case Presentation: We report a case of synchronous oropharyngeal and esophageal SCC primary tumors that were treated simultaneously with definitive chemoradiotherapy.
Introduction
Synchronous malignancy of base of tongue and oesophagus is difficult to diagnose and treat because both the malignancies are aggressive and have a poor survival [1]. In synchronous malignancy, sequencing of treatment is the most important factor survival [2]. Sequencing of treatment is difficult as treatment of one malignancy may delay the treatment of other malignancies which may result in disease progression. The presence of a second primary malignancy can bring with it unique therapeutic challenges and has been associated with inferior clinical outcomes [3,4]. Curative chemoradiation (CRT) is an effective treatment for isolated locally advanced HNSCC and is a next-best alternative therapy in non-operable ESCC [5,6]. Unfortunately, simultaneous CRT treatment of these tumors necessitates the delivery of high-dose radiation to expansive clinical target volumes (CTVs), causing concern for high rates of normal tissue toxicity. This case report has been reported in line with the SCARE Criteria.
Case Report
A 45-year-old male with no known comorbidities, chronic smoker and alcoholic for 15 years, was evaluated for difficulty in swallowing for 2 months (dysphagia grade 2). Patient also had history of significant weight loss. His general condition was fair and clinical examination revealed no significant abnormality. Upper gastrointestinal endoscopy revealed growth in the middle thoracic oesophagus at 30cm from incisors and biopsy was done, suggestive of poorly differentiated squamous cell carcinoma. Computed tomography chest revealed asymmetrical thickening of right lateral wall of mid thoracic oesophagus. Direct laryngoscopy was performed, showing growth present over right base of tongue up to right aryepiglottic fold and the biopsy showed squamous cell carcinoma. Computed tomography neck revealed 30 x 16 mm asymmetrical thickening over base of tongue up to right aryepiglottic fold with no cervical lymphadenopathy. A chest X-ray showed no evidence of lung metastasis. Hence the patient was diagnosed as carcinoma base of tongue cT4aN0M0 with early-stage carcinoma oesophagus.
After a multidisciplinary board discussion, the patient was planned for 2 cycles neoadjuvant chemotherapy followed by chemoradiation to oesophagus and oropharynx simultaneously. Patient received definitive chemoradiation to both the primaries simultaneously using CT-based radiation therapy treatment planning. Patients were immobilized in supine position with thermoplastic head- neck-shoulder mold. Radiotherapy treatment planning goals were achieved for target and normal tissue structures using a dual isocentric, RapidArc technique in Eclipse treatment planning system. For the oesophagus primary, the gross tumor volume (GTV) was defined as the primary tumor revealed in diagnostic chest CT image and for the head and neck primary the GTV was defined as primary tumor and the metastatic lymph nodes noted in clinical examination and diagnostic head and neck CT image data. The radiotherapy dose for the oesophageal disease was
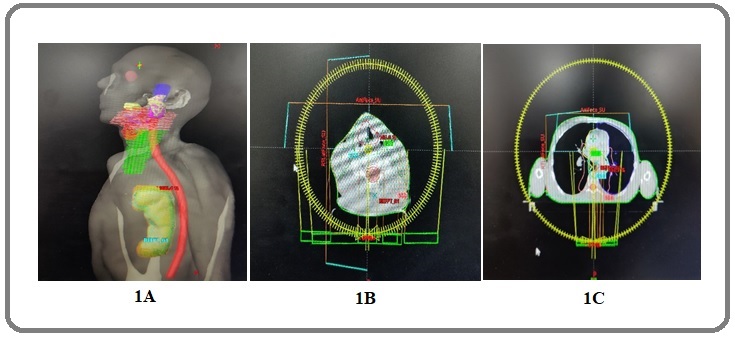
50.4 Gy in 1.8 Gy daily fractions and for the head and neck cancer was 70 Gy in 2 Gy daily fractions. Patient received 2 cycles of weekly Cisplatin 40 mg/m2 as a concurrent chemotherapy. Further chemotherapy deferred because of febrile neutropenia requiring filgrastim support. Patient developed grade 2 dermatitis and grade 2 mucositis during the treatment period. He also had to undergo hospitalisation for management of pneumonia and other treatment related toxicities. Patient came for follow up with no evidence of disease clinically at the end of 4 weeks post radiotherapy. PET CT whole body scan done after 4 months, suggestive of no evidence of disease in whole body (Figure 1).
Figure 1. A, Three-dimensional View of Contouring in Sagittal View for Both Esophagus and Oropharyngeal Disease; B, Shows the isodose lines of a RapidArc plan in axial section for oropharyngeal tumor; C, Shows the isodose lines of a RapidArc plan in axial section for esophageal tumor.
Discussion
The multifocal development of squamous cell carcinoma (SCC) is frequently observed in the upper aerodigestive tract (UADT) including the head and neck region and the oesophagus. The association of these cancers is observed both synchronously and metachronously [7]. These cancers are highly aggressive and until relatively recently were usually associated with a dismal prognosis. Regarding the treatment strategy, surgical resection has been the gold standard of treatment for localized UADT cancer. However, this surgery is extremely invasive and is also associated with high rates of mortality and morbidity, especially in patients with oesophageal cancer and pharyngeal cancer [8,9]. Patients with synchronous squamous cell carcinoma of the oesophagus (ESCC) and head and neck cancer (HNC) often require for extremely complex and invasive surgical procedures in order to resect both lesions. The surgical procedures for synchronous double cancer therefore represent an important clinical problem.
On the other hand, squamous cell carcinoma of the UADT is relatively sensitive to radiation and anticancer drugs such as 5-fluorouracil, cisplatin and paclitaxel. Definitive chemoradiotherapy is frequently indicated for ESCC while invasive esophagectomy is normally avoided [10]. For patients with HNC, the preservation of the vocal function can be achieved if HNC is cured after definitive chemoradiotherapy (CRT). Definitive CRT for synchronous ESCC and HNC is controversial due to the larger radiation field and associated toxicity [11]. In our institute, simultaneous definitive CRT has been applied in the treatment of synchronous ESCC and HNC. Another problem is that salvage treatment, which is frequently troublesome, may be indicated in cases with either residual or recurrent cancer after definitive CRT. Definitive CRT has proven to be a viable treatment option for isolated ESCC, with 2-year local control (LC) rates of 41–57% [5,12]. It is also an effective organ preservation therapy in isolated locally advanced laryngeal SCC6. However, long-term toxicity rates remain high for CRT in both of these primary sites. In oesophageal CRT, Cooper et al. reported grade ≥3 late toxicity rates of 29%, most of which (22%) directly involved the esophagus [5]. Unfortunately, these toxicities can significantly affect quality of life as illustrated by this case report.
The extent of high-dose RT fields should be of primary consideration. Because of the rich lymphatic network of the oesophagus, a large longitudinal field expansion around the oesophageal primary is required (3–5 cm superiorly and inferiorly) to encompass microscopic disease. Selection of RT dose and fractionation schedule is also crucial in striking a balance between tumor control and toxicity. Delivery of 70 Gy to gross tumor over 7 weeks in 2-Gy daily fractions with cisplatin chemotherapy is a standard curative regimen in locally advanced HNSCCs. Given the larger field sizes, the use of altered fractionation should be approached with caution when treating synchronous tumors, especially if concurrent chemotherapy is given or if the patient is elderly (as in our case) or of poor performance status (KPS). In such cases, the increased acute toxicity rates experienced with altered fractionation may outweigh potential LC benefits. For ESCC, the results of early trials led to the adoption of 50.4 Gy in 28 fractions as the standard for definitive CRT in our study [5,13]. Specifically, the INT 0123 trial was a CRT dose escalation study (64.8 vs 50.4 Gy) that showed no improvement in LC (50 vs 55%) and an increased treatment-related mortality (10 vs 2%, 11 vs 2 patients) in the high-dose arm [13].
Very few studies have been done so far to assess the treatment outcome, prognosis and treatment related toxicities in synchronous oesophageal and head and neck squamous cell carcinoma receiving curative concurrent chemoradiotherapy. Chen Y et al. retrospectively compared clinical outcome and prognosis of locally advanced ESCC with synchronous HNSCC patients who underwent chemoradiotherapy as curative treatment with patients of isolated ESCC. Compared to 60 matched isolated ESCC patients, synchronous ESCC and HNSCC patients had significantly worse prognosis (13.5 months versus 17.2 months, P = 0.01), more grade 3–4 toxicity, and higher percentage of treatment interruption. For synchronous ESCC and HNSCC group, the 1-year and 2-year survival rates were 52% and 13%, respectively [14]. Guillot et al 20 retrospectively reviewed 22 patients with multiple synchronous squamous cell carcinomas of the upper aerodigestive tract who had been treated with neoadjuvant chemotherapy followed by radiotherapy or surgery. Twelve patients were free of disease after locoregional treatment and mean survival was 17 months [15].
In conclusion, this unique case highlights the utility of dual isocentric and hybrid RapidArc techniques for treating synchronous oropharyngeal and oesophageal SCCs. In this setting, field size and dose/fractionation selections are integral in striking a balance between toxicity and tumor control. Patients with oesophageal carcinoma with a synchronous second primary in the head and neck region can safely be treated with definitive radiotherapy. But it is associated with higher rate of treatment related toxicities leading to increased inpatient admission. Because of limited published literature, this report may be helpful to understand the disease and treatment outcome of patients with oesophageal carcinoma with a synchronous second primary in head and neck region.
Acknowledgments
Not Applicable
Presentation or Awards at a meeting
Not Applicable
Source of Support and Funding
The authors declare that we have not received any funding in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Conflict of Interest statement
The authors declare no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Patients’ consent form
Required consent was taken from the patient.
References
- Epidemiology and Survival of Esophageal Cancer Patients in an American Cohort Nassri A, Zhu H, Muftah M, Ramzan Z. Cureus.2018;10(4). CrossRef
- Multiple primary tumours: challenges and approaches, a review Vogt A, Schmid S, Heinimann K, Frick H, Herrmann C, Cerny T, Omlin A. ESMO open.2017;2(2). CrossRef
- Synchronous second primary cancers in patients with squamous esophageal cancer: clinical features and survival outcome Lee JS , Ahn JY , Choi KD , Song HJ , Kim YH , Lee GH , Jung HY , et al . The Korean Journal of Internal Medicine.2016;31(2). CrossRef
- Chemoradiotherapy for Synchronous Multiple Primary Cancers with Esophageal Squamous Cell Carcinoma: a Case-control Study Li Q, Zhu Y, Zhang W, Yang H, Liang Y, Hu Y, Qiu B, Liu M, Liu H. Journal of Cancer.2017;8(4). CrossRef
- Chemoradiotherapy of locally advanced esophageal cancer: long-term follow-up of a prospective randomized trial (RTOG 85-01). Radiation Therapy Oncology Group Cooper JS , Guo MD , Herskovic A, Macdonald JS , Martenson JA , Al-Sarraf M, et al . JAMA.1999;281(17). CrossRef
- Long-term results of RTOG 91-11: a comparison of three nonsurgical treatment strategies to preserve the larynx in patients with locally advanced larynx cancer Forastiere AA , Zhang Q, Weber RS , Maor MH , Goepfert H, Pajak TF , et al . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2013;31(7). CrossRef
- Surgical strategies for esophageal cancer associated with head and neck cancer Morita M, Saeki H, Ito S, Kimura Y, Yamashita N, Ando K, Hiyoshi Y, et al . Surgery Today.2014;44(9). CrossRef
- In-hospital mortality after a surgical resection for esophageal cancer: analyses of the associated factors and historical changes Morita M, Nakanoko T, Fujinaka Y, Kubo N, Yamashita N, Yoshinaga K, Saeki H, et al . Annals of Surgical Oncology.2011;18(6). CrossRef
- Salvage pharyngolaryngectomy with total esophagectomy following definitive chemoradiotherapy Niwa Y, Koike M, Fujimoto Y, Oya H, Iwata N, Nishio N, Hiramatsu M, et al . Diseases of the Esophagus: Official Journal of the International Society for Diseases of the Esophagus.2016;29(6). CrossRef
- Salvage esophagectomy after definitive chemoradiotherapy for synchronous double cancers of the esophagus and head-and-neck Yoshida R, Morita M, Ando K, Masuda T, Saeki H, Oki E, Sadanaga N, et al . Diseases of the Esophagus: Official Journal of the International Society for Diseases of the Esophagus.2010;23(1). CrossRef
- Localized synchronous squamous cell carcinomas of the esophagus and hypopharynx treated with definitive concurrent chemoradiotherapy with a unified radiotherapy plan Wallach JB , Rosenstein MM , Kalnicki S. Current Oncology (Toronto, Ont.).2014;21(2). CrossRef
- Chemoradiation followed by surgery compared with chemoradiation alone in squamous cancer of the esophagus: FFCD 9102 Bedenne L, Michel P, Bouché O, Milan C, Mariette C, Conroy T, Pezet D, et al . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2007;25(10). CrossRef
- INT 0123 (Radiation Therapy Oncology Group 94-05) phase III trial of combined-modality therapy for esophageal cancer: high-dose versus standard-dose radiation therapy Minsky BD , Pajak TF , Ginsberg RJ , Pisansky TM , Martenson J, Komaki R, Okawara G, et al . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2002;20(5). CrossRef
- Treatment Outcomes of Patients with Locally Advanced Synchronous Esophageal and Head/Neck Squamous Cell Carcinoma Receiving Curative Concurrent Chemoradiotherapy Chen YH , Lu HJ , Chien CY , Lo CM , Wang YM , Chou SY , et al . Scientific Reports.2017;7. CrossRef
- Neoadjuvant chemotherapy in multiple synchronous head and neck and esophagus squamous cell carcinomas Guillot T, Spielmann M, Kac J, Luboinski B, Tellez-Bernal E, Munck JN , Bachouchi M, et al . The Laryngoscope.1992;102(3). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2023
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times