Pediatric Mesenchymal Hamartoma of the Liver: A Diagnostic Dilemma
Download
Abstract
Background and objective: Benign liver tumors are relatively uncommon in children. Mesenchymal hamartoma (MH) is a benign liver tumor and the second most common benign pediatric hepatic tumor after infantile hemangioma. It is most frequently observed in children under 2 years of age. Diagnosis can be challenging due to non-specific clinical symptoms and the lack of definitive laboratory studies. Histological evaluation of tissue is essential for definitive diagnosis. This case report describes a rare case of mesenchymal hamartoma in a 2-year-old child, highlighting the diagnostic challenges.
Case presentation: A previously healthy 2-year-old male was referred to our institution for evaluation of a liver mass. He suffered from a 10-week history of loss of appetite and abdominal distension. He reported no fever or trauma. Physical examination revealed a large, non-tender hepatomegaly without shifting dullness. Abdominal ultrasound showed a solitary right lobe mass. Further imaging with a CT scan of the abdomen revealed a large, multi-loculated lesion in the right lobe of the liver with arterial enhancing intervening septae. The lesion compressed and displaced the right portal vein and right hepatic vein. Laboratory evaluation revealed normal liver function tests, serum alpha-fetoprotein (AFP), and other blood parameters. Differential diagnoses included liver cyst, hydatid cyst, and biliary cystadenoma. After multidisciplinary discussion, a surgical approach was chosen to obtain a definitive histological diagnosis and address the cystic liver lesion. The patient underwent a right hepatectomy with r section of the 14 × 12 cm mass. No major peri-operative complications developed, and the patient was discharged on postoperative day 6. Pathological review of the resected mass revealed a mixture of bile ducts, vessels, irregular liver cell plates, and loose mesenchyme containing variable-sized cysts, consistent with mesenchymal hamartoma. The patient remains asymptomatic at follow-up.
Conclusion: Benign liver tumors in children are relatively rare. The diagnosis of mesenchymal hamartoma can be challenging due to non-specific symptoms, normal laboratory findings, and potential for complications arising from local compression. Advanced imaging can be helpful, but differentiating it from other tumors such as undifferentiated embryonal sarcoma can be difficult based on imaging alone. Surgical excision remains the gold standard for definitive diagnosis and treatment.
Introduction
Background
Benign tumors of the liver are relatively rare in children. Mesenchymal hamartoma (MH) is a benign tumor of the liver. It is the second most common benign pediatric hepatic tumor after infantile hemangioma [1]. Mostly it is seen in children less than 2 years of age. The diagnosis of this tumor is difficult because of nonspecific clinical symptoms and lack of definitive laboratory studies. The precise diagnosis of mesenchymal hamartoma relies on histological evaluation of the tissue. Mesenchymal hamartoma of liver are a very rare clinical entity and it is relevant to keep a high index of suspicion in paediatric age group.Various studies have shown surgical excision is the gold standard to diagnose and treat these conditions [4-5]. We hereby present a rare case in a 2 year old child with mesenchymal hamartoma and its diagnostic challenges.
‘This case report has been reported in line with the SCARE Criteria.
Patient Information
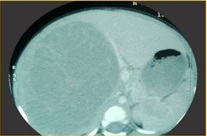
A 2 year old previously healthy male of Hindu religion was referred to our institution for evaluation of a liver mass. By history,his parents informed that he developed loss of apetite and abdominal distension since last 10 weeks. He had no history of fever/trauma. There was no past history of any surgical intervention. There was no relevant drug history or family history of similar illness. On clinical evaluation,he was found to have huge non-tender hepatomegaly with no shifting dullness present.Ultrasound abdomen showed solitary right lobe mass. On further imaging, CT scan of the abdomen was done which showed a large multiloculated lesion in right lobe liver with arterial enhancing intervening septae within.The lesion was compressing and displacing right portal vein and right hepatic vein (Figure 1,2).
Figure 1. CT Abdomen Showing Right Hepatic Mass.
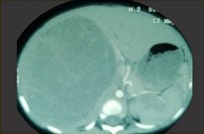
Figure 2. CT Abdomen Showing Large Righ Hepatic Mass Abutting Middle Hepatic Vein .
At that time, laboratory evaluation showed normal liver function tests with a prothrombin time (PT) of 11.6 sec; (INR) 1.1; fibrinogen 435 mg/dL; (ALT) 21 U/L; (AST) 26 U/L; and (GGT) 10 U/L. His inflammatory markers were slightly elevated with CRP 5.4 and ESR 30. His alpha-fetoprotein (AFP) was normal (4.4 IU/mL) and serum CEA level was normal (0.24 ng/ml). Antibodies to Entamoeba histolytica and Echinococcus were negative. Diffential diagnosis of complex cystic lesion of liver ,biliary cystadenoma were kept in mind. Hydatid cyst and amoebic abscess were ruled out as their antibodied were found negative in this case. To reach at final diagnosis, histological evaluation of representative liver lesion tissue was required.
Intervention
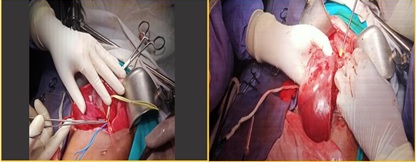
Pediatric surgery consultation was sought for multidisciplinary care, and plan for surgical excision of mass with right hepatectomy was made in our tertiary care hospital with complete paediatric ICU care backup. Team of 4 surgeons including 2 chief surgeons and two superspeciality residents in oncosurgery performed the surgery. Patient was optimized for surgery with proper pre-operative anaesthesia check-up.He was given preoperative antibiotic 4 hours before surgery and was kept nil per oral for 6 hours before surgery. Surgery was done after placing patient position in supine position with arms abducted at 90 degree.Preoperative central venous access and arterial line were placed. He was intubated after sedation and ryle’s tube and foley’s catheter were introduced.Abdomen was prepared with 10 percent betadine paint and finally sterile draping was done. Roof top incision was made with operative findings of presence of 14× 12 cm right hepatic lesion occupying segment [5-7]. There was no metastasis elsewhere in abdomen.Thompson retractors were applied and liver was mobilised after dividing right triangular ligament. Hilar plate lowering was done and right hepatic artery and right portal vein were looped with umblical tape. Cholecystectomy was perfomed. Right hepatic vein was identifed after dissecting hepatocaval ligament. Finally right hepatic artery and right portal vein were divided and suture with 4-0 monofilament prolene suture. Line of demarcation was seen over liver making the way for liver transection along that line. Combination of harmonic scalpel and CUSa were used for liver transection and major right hepatic duct and minor portal vein radicals were ligated with fine monofilament prolene suture. Subsequently right hepatectomy with resection of 14× 12 cm mass was done after dividing right heaptic vein with white vascular stapler (Figure 3).
Figure 3. Intraoperative Pictures with Right Hepatectomy.
Hemostasis was confirmed and drain was placed in subheaptic space. Abdomen was closed in layers.Patient was shifted to paediatric ICU. He was kept in Paediatric ICU for 2 days and was allowed orally from second day postoperatively.
Follow up
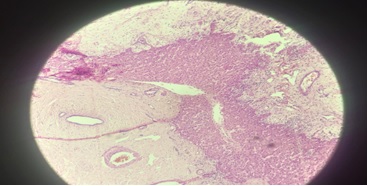
Recovery was uneventful and he was discharged from hospital on postoperative day 6. The pathological review of the resected mass showed mixture of bile ducts,vessels,irregular liver cell plates and loose mesenchyme containing variable sized cysts. The mesenchyme consists of stellate cells in a loose matrix. (hematoxylin and eosin stain with 200x magnification), consistent with a mesenchymal hamartoma (Figure 4).
Figure 4. Histopathology Slide Consistent with Features of Hamartoma.
He remained on regular follow-up after every 3 months to our OPD and had no complaints at present.He remained on follow -up to us from last 2 years.
Discussion
Benign tumors of the liver are relatively rare in children. Mesenchymal hamartoma was first described in the literature by Edmondson in 1956 [2]. The diagnosis of mesenchymal hamartoma still remains a challenge with non –specific complaints,normal laboratory findings. A delay in diagnosis can lead to complications from local compression [3]. Advance imaging can diagnose this entity if index of suspicion is high. Differentiating between mesenchymal hamartoma and other tumors such as an undifferentiated embryonal sarcoma is difficult based on imaging alone [4]. The precise diagnosis of mesenchymal hamartoma relies on histological evaluation of the tissue. However, because of the risk of recurrence and malignant transformation, the gold standard for the diagnosis and treatment of mesenchymal hamartoma is complete surgical excision [5]. We performed surgical excision of liver tumor to reach at the final diagnosis and were able to attain good outcome with the help of multidisciplinary team approach.The limitation in our case report is that we don’t have a good interventional radiologist to exactly target the area of thickened intervening septae to get biopsy preoperatively.The implication of this case report falls on the all paediatric population patient diagnosed to have large complex cystic lesion of liver where high high index of suspicion is required to keep mesenchymal hamartoma also as differential diagnosis.
Declarations
Ethical approval
Ethical approval was waived by the local Ethics Committee as it is part of routine care.
Informed Consent
Taken from the patient.
Consent for Publication
Not Applicable.
Availability of data and material
Not Applicable.
Funding
No funds, grants, or other support was received
Financial interests
The authors have no relevant financial or non-financial interests to disclose.
References
- Hepatic Mesenchymal Hamartoma: A Short Review Siddiqui MA , McKenna BJ . Archives of Pathology & Laboratory Medicine.2006;130(10). CrossRef
- “Differential diagnosis of tumors and tumor-like lesions of liver in infancy and childhood,” H. A. Edmondson . Archives of Pediatrics & Adolescent Medicine.1956;91(2):168-186.
- Liver transplantation for a giant mesenchymal hamartoma of the liver in an adult: Case report and review of the literature Li J, Cai J, Guo Q, Li J, Sun X, Hu Z, Cooper DK , Shen Z. World Journal of Gastroenterology : WJG.2015;21(20). CrossRef
- Mesenchymal hamartoma or embryonal sarcoma of the liver in childhood: a difficult diagnosis before complete surgical excision Wildhaber BE , Montaruli E, Guérin F, Branchereau S, Martelli H, Gauthier F. Journal of Pediatric Surgery.2014;49(9). CrossRef
- Differential diagnosis and management of liver tumors in infants Fernandez-Pineda I, Cabello-Laureano R. World Journal of Hepatology.2014;6(7). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2023
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times