Reoperative Thyroid Bed Surgery: An Evaluation of Complications and Outcomes
Download
Abstract
Introduction: Secondary surgeries for thyroid cancers are conventionally associated with long term morbidities. This study was conducted to assess the efficacy of our Institutional Surgical Protocol while dealing with such cases, through the complications and levels of disease clearance achieved.
Methods: It was a retrospective observational study; patients who underwent reoperative thyroid surgery from January 2020 to January 2023 were included. All patients were operated as per the Institutional Policy.
Results: 25 patients were included in the study. Secondary surgeries included Central Neck Dissection with Lateral Neck Dissection (40%), Revision thyroidectomy (24%) and Completion thyroidectomy (12%). The pathological diagnoses of the patients were mainly Well differentiated Thyroid cancers like Papillary Carcinoma (72%) and Follicular Carcinoma (12%). Complications following Secondary surgery included Permanent Hypoparathyroidism (4%) and Permanent Vocal cord palsy (4%). Literature shows an incidence of 5-10% and 0-5% respectively. In 60% of patients, there was no uptake in the Postop Iodine scan which displayed complete disease removal.
Conclusion: Our Institutional Protocol results in a significant reduction in post op complications as compared to literature. Adequate disease clearance is ascertained by the lack of uptake in the Postop Iodine Scan.
Introduction
Secondary surgeries for Thyroid cancers like Completion Thyroidectomy or Revision Thyroidectomy with or without Neck Dissection are not rarely performed procedures and have been considered as potential points for complications. The presence of scarred and friable tissue with distorted anatomy pose as a threat for Recurrent laryngeal nerve (RLN) injury and Parathyroid vascular insufficiency [1]. Complications such as Vocal cord paresis/ palsy and Transient/Permanent Hypoparathyroidism are thus associated more with revision cases.
With the start of a Nuclear Medicine Department at our institute (2020), many cases are being referred for Radioiodine treatment. Following evaluation and risk stratification if the disease load seems to have been inadequately cleared, some of these cases end up requiring re-surgery. This is not a desirable procedure for the patient or any surgeon. But we have developed a protocol for addressing such cases.
The aim of this study was to study the rate of complications and levels of disease clearance achieved of such surgeries done with the institutional protocol at our institute.
Materials and Methods
It was a retrospective observational study of thyroid cancer patients treated at a tertiary cancer centre in India. All patients who underwent secondary surgery of the thyroid bed from January 2020 to January 2023 were included in the study.
Patients who underwent primary thyroid surgery from outside and got a histopathological report of malignancy were referred to our Nuclear Medicine Department for further management. The status of residual/recurrent disease was then assessed by biochemical/imaging parameters, risk stratification was done and the patients were sent to the Head & Neck Unit of Surgical Oncology for re-exploration of the thyroid bed (secondary surgery). All surgeries were performed according to the Institutional Protocol (Table 1).
| Preoperative Cross-sectional imaging |
| All cases undergo a Contrast enhanced CT or MRI during evaluation for surgery. The imaging helps to aptly localise and quantify the target tissue in the thyroid bed. |
| Central and Mediastinal nodes are also seen adequately. |
| Intraoperative Nerve Monitoring (IONM) |
| Intermittent IONM aids in identification of the RLN and its branches whose location and course have been altered by the prior procedure. |
| Magnifying Loupes (2.5x) |
| Helps with the meticulous dissection of the Parathyroid glands while maintaining their vasculature and to track the unusual branching patterns of the Recurrent laryngeal nerves. |
| Bipolar cautery |
| When used with saline irrigation, Bipolar cautery only affects the tissue held between its limbs and thus prevents burn injury to vital structures unlike Monopolar cautery. |
Demographics, primary and secondary surgery details were recorded from the case files. Outcome variables like complications (wound infection/dehiscence, permanent hypoparathyroidism, permanent vocal cord palsy palsy), details of Radioiodine treatment and the status of disease at the end of the Postop Iodine scan were also recorded and analysed. All patients were followed up for 6 months.
Operative Definitions
1) Completion Thyroidectomy: Re-exploration of the neck to remove the contralateral thyroid lobe; wherein the contralateral thyroid bed was not addressed earlier.
2) Revision Thyroidectomy: Re-exploration of the neck to remove thyroid tissue; wherein the thyroid bed was addressed earlier (residual/recurrence).
3) Permanent Hypoparathyroidism: Persisting Hypocalcemia 6 months following thyroid surgery.
4) Permanent Vocal cord palsy: Persisting vocal cord palsy 6 months following thyroid surgery.
Statistical Analysis
A descriptive analysis of the patient profiles, primary surgery details, pathological types of disease, reoperative procedures, complications and iodine scans were performed.
Results
25 patients were included in the study. The mean age was 49.4 years. There were 9 male patients and 16 female patients. The details of the primary and secondary surgeries are given in Table 2. Twelve patients had undergone Total Thyroidectomy and 7 patients had Hemithyroidectomy. Secondary surgeries included Central Neck Dissection (CND) with Lateral Neck Dissection (LND) (40%), Revision thyroidectomy (24%) and Completion thyroidectomy (12%).
The pathological diagnoses of the patients were mainly Well differentiated Thyroid cancers like Papillary Carcinoma (72%) and Follicular Carcinoma (12%). There were some cases of Medullary Carcinoma (8%) and Anaplastic Carcinoma (4%) also (Table 2).
| Primary Surgery | No. | % |
| Hemithyroidectomy | 7 | 28 |
| Total Thyroidectomy | 12 | 48 |
| TT + Central Neck Dissection | 3 | 12 |
| TT + CND + Lateral Neck Dissection | 3 | 12 |
| Secondary Surgery | ||
| Completion Thyroidectomy | 3 | 12 |
| CT + CND | 2 | 8 |
| CND + LND | 10 | 40 |
| CT + CND + LND | 2 | 8 |
| Revision Thyroidectomy | 6 | 24 |
| Pathological Variants | ||
| Pathology | ||
| Papillary CA | 18 | 72 |
| Follicular CA | 3 | 12 |
| Medullary CA | 2 | 8 |
| Anaplastic CA | 1 | 4 |
| Hurthle Cell CA | 1 | 4 |
| Complications of Reoperative Surgery | ||
| Complications | ||
| Permanent Hypoparathyroidism | 1 | 4 |
| Permanent Vocal Cord Palsy | 2 | 8 |
| Wound dehiscence/infection | 0 | 0 |
(TT,Total Thyroidectomy; CND, Central Neck Dissection; CT, Completion Thyroidectomy; LND, Lateral Neck Dissection)
Complications following Secondary surgery of the thyroid bed included Permanent Hypoparathyroidism (4%) and Permanent Vocal cord palsy (4%). In both patients with palsy, the Recurrent Laryngeal Nerve had to be resected due to tumor infiltration from the diseased gland and central compartment node respectively (Table 2).
Efficacy of disease clearance was monitored using the levels of uptake in the Postoperative Radioiodine scan. There was no uptake in 60% of patients, which displays complete disease removal (Table 3).
| Radio Iodine Scan | No. | % |
| No Uptake | 15 | 60 |
| Uptake in Neck | 7 | 28 |
| Not Applicable | 3 | 12 |
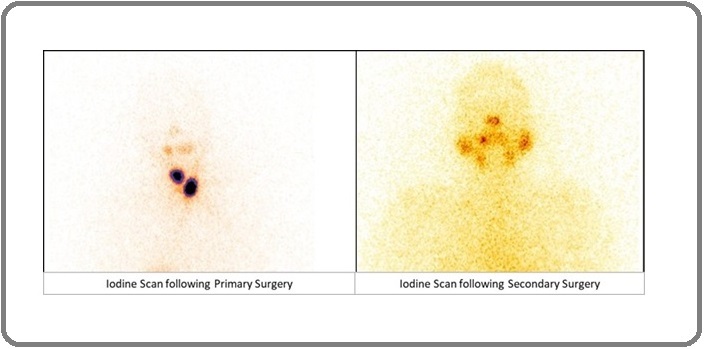
Figure 1 shows the Iodine scans of a patient before and after the Secondary Surgery. In 3 patients the Iodine scan couldn’t be applied due to their pathological subtypes (Medullary, Anaplastic cancers).
Figure 1. The 1st Picture Depicts Iodine Scan Following Primary Surgery with Disease in the Thyroid Bed and Lateral Compartment of Neck. The 2nd picture shows iodine scan following secondary surgery (CND + LND) with complete clearance of disease in neck.
Discussion
Nearly 30% of the patients with Differentiated thyroid cancer (DTC) present with tumor recurrence in the thyroid bed, central neck, lateral neck or the mediastinum [2]. The American Thyroid Association (2015) have suggested some variables to consider while deciding how to manage a case of DTC with recurrent or persistent nodal disease [3].
Reoperative thyroid surgery can be challenging because of anatomic changes after primary surgery, especially in the central neck, and is associated with high complication rates in inexperienced hands. Table 4 summarises the incidence of complications for such secondary surgeries from studies done over the past 30 years.
| Author | Year | No. of Patients | Permanent Hypoparathyroidism (%) | Permanent Vocal cord palsy (%) |
| Deo et al [4] | 2023 | 182 | 2.70 | 1.60 |
| Medas et al [5] | 2019 | 152 | 10 | 4.60 |
| Benkhadoura et al [6] | 2017 | 73 | 0 | 1.40 |
| Kranthikumar et al [7] | 2016 | 53 | 16.60 | 0 |
| Cayonu et al [8] | 2014 | 61 | 4.90 | 0 |
| Phelan et al [9] | 2012 | 117 | 2 | 0 |
| Kurmann et al [10] | 2012 | 118 | 3.80 | NM |
| Pironi et al [11] | 2008 | 76 | NM | 3.90 |
| Lefevre et al [12] | 2007 | 685 | 2.50 | 1.50 |
| Myint Tun et al [13] | 2003 | 25 | NM | 4 |
| Moley et al [14] | 1999 | 132 | NM | 3.70 |
| Chao et al [15] | 1997 | 115 | 1.70 | 1.70 |
| Levin et al [16] | 1992 | 116 | 3.40 | 1.70 |
Most of these studies have included procedures done for non-malignant diseases also, our study focusses specifically surgeries done for thyroid cancers.
The Permanent Hypoparathyroidism rates range from 5-10% in the described studies. Higher incidence of hypocalcemia is attributed by the authors to extensive dissection done to clear recurrent or metastatic disease, thereby compromising vasculature of the parathyroid glands. In our study, we were able to restrict permanent hypoparathyroidism to just one patient (4%); the use of magnifying loupes and meticulous dissection using bipolar forceps helped us preserve the parathyroids.
Permanent vocal cord palsy ranged in literature from 0-5%. The authors who couldn’t prevent injury to the RLN ascribed it to the postop fibrosis, distorted anatomy and the requirement of extensive resections indicated in reoperative cases. We reported an incidence on 8%. In both our cases, the tumor had infiltrated the nerve grossly and resection of the nerve was required to ensure oncological safety. The cases were of Anaplastic and Medullary carcinoma, known for their aggressive nature. In other cases, the use of Intraoperative nerve monitoring helped us track the contorted courses of the RLN and diligent dissection helped clear the disease without causing trauma.
The use of Cross-sectional imaging in thyroid cancers is traditionally indicated for invasive tumours (to rule out posterior capsular or mediastinal extension, tracheal or oesophageal involvement) and in clinically apparent multiple or bulky lymphadenopathy (cervical or mediastinal). But our protocol helped us to map out the disease preoperatively, thereby reducing complications.
Numerous studies have established the role of IONM in preventing RLN injury during routine thyroid surgery. Wilhelm et al studied 5446 patients and found out that routine use of IONM reduced the long-term vocal cord dysfunction from 3.7% to 2.2% (p<0.01) [17]. Wojtczak et al studied 711 patients and concluded that the risk factors causing complications in thyroid surgery are not significant for any increase in the rate of vocal fold paralysis with IONM, as compared to direct vision [18]. But we at our institute do not use IONM for routine thyroid surgeries where the anatomy is usually constant. We have found its utility more in operations where the normal planes and nerve course have been violated by prior dissection.
Loupes and microscopes are also essentially becoming a part of thyroid surgery. D’Orazi et al studied 782 patients over 10 years and concluded that surgical loupes (4.5x) and microsurgical technique essentially reduced postop complications in thyroid surgery [19].
A recent metanalysis by Sapalidis et al advocated the use of magnification techniques for identification of RLN and parathyroid glands to be as safe as direct vision but didn’t find them to decrease the risk of RLN injury and hypocalcemia as compared with direct vision [20]. Limitations of our study included the retrospective nature and the limited sample size.
In conclusion, Following our Institutional Protocol for all cases of Reoperative surgery of the thyroid bed resulted in a significant reduction in post op complications as compared to literature. Adequate disease clearance was ascertained by the lack of uptake in the Postop Iodine Scan.
References
- Morbidity following central compartment reoperation for recurrent or persistent thyroid cancer Kim MK , Mandel SH , Baloch Z, Livolsi VA , Langer JE , Didonato L, Fish S, Weber RS . Archives of Otolaryngology--Head & Neck Surgery.2004;130(10). CrossRef
- Reoperative thyroid surgery. Surgery of the Thyroid and Parathyroid Glands. 2021 Freeman JL , Sewell AB, , Hales NW , Randolph GW . .
- Management of recurrent/persistent nodal disease in patients with differentiated thyroid cancer: a critical review of the risks and benefits of surgical intervention versus active surveillance Tufano RP , Clayman G, Heller KS , Inabnet WB , Kebebew E, Shaha A, Steward DL , Tuttle RM . Thyroid: Official Journal of the American Thyroid Association.2015;25(1). CrossRef
- Re-operative surgery for differentiated thyroid cancer: A single institutional experience of 182 cases Deo S, Bansal B, Bhoriwal S, Bal CS , Mishra A, Sharma J, Singh S, et al . European Journal of Surgical Oncology: The Journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology.2023;49(10). CrossRef
- Complications after reoperative thyroid surgery: retrospective evaluation of 152 consecutive cases Medas F, Tuveri M, Canu GL , Erdas E, Calò PG . Updates in Surgery.2019;71(4). CrossRef
- Recurrent laryngeal nerve injury and hypoparathyroidism rates in reoperative thyroid surgery Benkhadoura M, Taktuk S, Alobedi R. Turkish Journal of Surgery.2017;33(1). CrossRef
- Safety of Completion Thyroidectomy for Initially Misdiagnosed Thyroid Carcinoma Kranthikumar G, Syed N, Nemade H, Pawar S, Chandra Sekhara Rao LM , Subramanyeshwar Rao T. Rambam Maimonides Medical Journal.2016;7(3). CrossRef
- Surgical approach and outcomes for revision surgery of the central neck compartment Cayonu M, Acar A, Eryilmaz A, Oguz O. The Journal of Craniofacial Surgery.2014;25(5). CrossRef
- Revision Thyroid Surgery: Are There More Complications? Phelan E, Randolph GW . Otolaryngology–Head and Neck Surgery.2012;147(2_suppl). CrossRef
- Morbidity rate of reoperation in thyroid surgery: a different point of view Kurmann A, Herden U, Schmid SW , Candinas D, Seiler CA . Swiss Medical Weekly.2012;142. CrossRef
- [Reoperative thyroid surgery: personal experience and review of the literature] Pironi D, Panarese A, Candioli S, Manigrasso A, La Gioia G, Romani AM , Arcieri S, Mele R, Filippini A. Il Giornale Di Chirurgia.2008;29(10).
- Reoperative surgery for thyroid disease Lefevre JH , Tresallet C, Leenhardt L, Jublanc C, Chigot J, Menegaux F. Langenbeck's Archives of Surgery.2007;392(6). CrossRef
- Reoperative thyroid surgery in hospital universiti sains malaysia Tun M, Salekan K, Sain AHM . The Malaysian journal of medical sciences: MJMS.2003;10(1).
- Preservation of the recurrent laryngeal nerves in thyroid and parathyroid reoperations Moley JF , Lairmore TC , Doherty GM , Brunt LM , DeBenedetti MK . Surgery.1999;126(4).
- Reoperative thyroid surgery Chao TC , Jeng LB , Lin JD , Chen MF . World Journal of Surgery.1997;21(6). CrossRef
- Reoperative thyroid surgery Levin KE , Clark AH , Duh QY , Demeure M, Siperstein AE , Clark OH . Surgery.1992;111(6).
- Routine use of intraoperative nerve monitoring is associated with a reduced risk of vocal cord dysfunction after thyroid cancer surgery Wilhelm A, Conroy PC , Calthorpe L, Frye W, Sosa JA , Roman S. BMC surgery.2023;23(1). CrossRef
- Proving the Superiority of Intraoperative Recurrent Laryngeal Nerve Monitoring over Visualization Alone during Thyroidectomy Wojtczak B, Marciniak D, Kaliszewski K, Sutkowski K, Głód M, Rudnicki J, Bolanowski M, Barczyński M. Biomedicines.2023;11(3). CrossRef
- Use of loupes magnification and microsurgical technique in thyroid surgery: ten years experience in a single center D'Orazi V, Panunzi A, Di Lorenzo E, Ortensi A, Cialini M, Anichini S, Ortensi A. Il Giornale Di Chirurgia.2016;37(3). CrossRef
- Comparison between Magnification Techniques and Direct Vision in Thyroid Surgery: A Systematic Review and Meta-Analysis Sapalidis K, Papanastasiou A, Fyntanidou V, Aidoni Z, Michalopoulos N, Katsaounis A, Amaniti A, et al . Medicina (Kaunas, Lithuania).2019;55(11). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2024
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times