Incorporation of a Multidisciplinary Tumor Board (MTB) in Cancer Patient Care: Experiences of a Comprehensive Cancer Care Hospital in Eastern India
Download
Abstract
Background and objective: A multidisciplinary tumor board (MTB) is a critical component of comprehensive cancer care, providing evidence-based treatment recommendations for patients. This analysis aimed to assess the importance of MTB in comprehensive cancer care and evaluate its impact on cancer patient management and treatment compliance.
Materials and method: A one-year audit was conducted on patients discussed at the tumor board of a private comprehensive cancer care hospital in Eastern India between September 2020 and August 2021. Data was collected before, during, and after each MTB meeting.
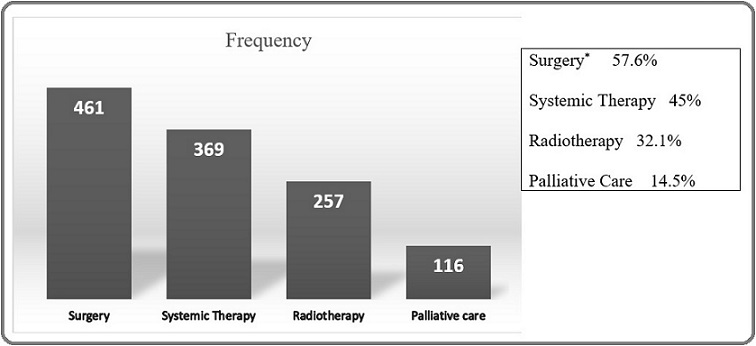
Results: A total of 800 cases were discussed during the audit period. Approximately 60% of cases were presented by surgical oncology, 21% by medical oncology, and the remaining by other departments. The median age of patients was 56 years. The most common tumor type was head and neck cancer (28.5%), followed by gastrointestinal and breast cancers (55.2%). The most common treatment plans included surgical management (57.6%), systemic therapy (45%), radiotherapy (32.1%), and palliative care (14.5%). Treatment compliance exceeded 50%, and after one year, 52.87% of patients were still alive. The audit revealed that more than 20% of the data was missing.
Conclusion: The MTB practice demonstrated improvements in the management of advanced-stage disease and increased treatment compliance. The audit also highlighted the cancer demographics of this region of India. A prospective trial with a larger patient population, comprehensive follow-up data, and reduced missing data points is recommended for future studies to evaluate the true impact of multidisciplinary care.
Introduction
Cancer has become one of the major health problems worldwide as well as in India. It is now second most commonly occurring disease and approximately 10% of world population are suffering from cancer [1]. Due to complex management of cancer, it requires collective opinion from specialised physicians of various departments likes medical oncology, surgical oncology, radiation oncology, radiodiagnosis, pathology and other departments related to cancer management. By definition, multidisciplinary tumour board (MTB) or tumour board committee (TBC) is a team of specialised physicians related to cancer diagnosis and treatment. The decision can be taken either by multidisciplinary clinic which is also called joint clinic where the specialists directly see and examined the patient, or it can be done by formal meeting arranged by the specialists on specific day and time and discuss relevant findings to plan the management [2]. Tumour board practice can provide the following benefits – a) evidence based personalised, precise treatment to the cancer patient, b) participation of interdisciplinary professionals create academic environment helps continued medical education to the senior as well as to the junior physicians, c) ensures good clinical practice in the hospital and d) helps in orientation of the supporting staffs (nursing personals, patient care coordinator etc.) regarding cancer patient management. Multidisciplinary tumour board is properly formed and a common practice in large academic centres of developed countries [3]. But Its practice is inconsistent in developing countries like India [4]. Though there is limited evidence on benefits of multidisciplinary management (MDM) on cancer patient outcomes [5, 6], few studies showed changes in the diagnostic/staging accuracy [7, 8], and improves management plan [9]. One study by Freytag et al showed that higher number of tumour board per case increased overall survival [10]. But later, further analysis failed to show the survival benefits of a higher number of TBC meeting per case due to an immortal time bias [11]. Other benefits like higher treatment rate and more adherence to treatment guidelines were shown by few studies [6, 12]. It can be extrapolated that TBC meeting for cancer management may gain the confidence of the patients and increase the treatment compliance in the developing country like India where treatment non-compliance is a major factor for poor outcome [13]. The evidence of MTB guided treatment audit is very limited in India.
MTB discussion on cancer patient management is not very common practice in the privet hospitals of eastern India. So, the initiation of TBC meeting in a non-government medical college and hospital with comprehensive cancer care in the eastern India helps to ensure evidence-based management of the cancer patients. By this audit of TBC meeting cancer patients will help to understand the demographic of cancer patients including the involvement of the various clinical departments, treatment compliance of the cancer patients and the reason for non-compliance, and role of patient care coordinator for the management of cancer patients.
Materials and Methods
This study includes the patients presented in the TBC meeting at Kalinga Institute of Medical Sciences (KIMS) - Cancer Center (KCC) from August 2020 to July 2021 (for 12 months). The data is collected prospectively before and after each tumour board meeting. Patients’ confidentiality is maintained during data collection and various codes were used to indicate the important data.
The TBC meeting data includes the name of the departments presented the cases, contact number, patient’s demographics, short history of the illness, performance status (Eastern Cooperative Oncology Group – ECOG) including physical examination result, important points of histopathology and radiology report, relevant laboratory results, primary diagnosis, staging include both pathological as well as clinical, initial plan by respective departments followed by management decision taken by MTB.
It is a single tumour board committee (TBC) meeting where all types of cancer patients are discussed. The TBC meeting is mainly participated by surgical oncology, medical oncology, radiation oncology, radiology, and pathology departments and occasionally by some other departments like gastro-intestinal surgery, gynaecology & obstetrics, otorhinolaryngology etc. The meeting is usually conducted once a week on a specific day and time. The case lists are prepared beforehand on a preformed excel sheets with all available details including initial plan of management by primary physicians. After the meeting one important data is completed by entering the recommended management plan decided by the MTB. Subsequently the treatment details and follow up data are collected from hospital records with the help of PCC. Due to multiple reasons some patients are unable to continue treatment or follow up in this hospital and they are lost to follow up after sometimes. Those patients are tracked down by PCC and the treatment related information are collected as much as possible. This information is used to complete the master chart, but still few patients are unreachable, and they are truly lost to follow up. Each patient data was assessed as per the TBC meeting master chart points.
Statistical Analysis
The data were recorded in a preformed Excel spreadsheets prospectively before or after tumour board for discussion and data collection. Later, for analysis, the variables were extracted from tumour board master chart on an another excel sheet and organised properly. The entered data were sanitised and checked multiple times for any errors. The missing data for any parameter was considered properly for analysis. As it is an audit without any standard arm for comparison, range, median and percentage were obtained from the analysis. The follow up outcome was analysed from 1st registration date at oncology department to last follow up date (in case of lost to follow up patients) or date of death. From this analysis range and median follow up were derived.
Results
Eight hundred cases were presented in the tumour board from August 2020 to July 2021. Among them 573 (71.63%) patients were new cases, and 227 (28.37%) patients were discussed more than once in the MTB. Approximately 60% cases were presented by surgical oncology team, 21% by the medical oncology and rest of the cases by the radiation oncology and other departments (Table 1).
| Refer From [S.O, M.O, R.O, Others] | Frequency | Percent |
| S. O | 479 | 59.88 |
| M. O | 168 | 21 |
| R. O | 68 | 8.5 |
| OTHERS | 85 | 10.63 |
| Total | 800 | 100 |
[Surgical oncology – 59.88%, S. O – Surgical Oncology, M.O – Medical Oncology, R.O – Radiation Oncology, TBM – tumour board meeting]
Regarding patient characteristics, the median age of patients was 56 years. The highest number of patients were within the age range from 41 years to 60 years, approximately 44% and 33% of patients were above the age of 60 years. Male and female ratio was almost similar 51.38% and 48.62% respectively (Table 2).
| Age Group | ||
| Age | Frequency | Percent |
| <20 | 20 | 2.5 |
| 21-40 | 159 | 19.9 |
| 41-60* | 351 | 43.9 |
| 61-70# | 181 | 22.6 |
| >70# | 88 | 11 |
| Missing | 1 | 0.1 |
| Total | 800 | 100 |
| Gender£ | ||
| M | 411 | 51.38 |
| F | 389 | 48.63 |
| Total | 800 | 100 |
[*Productive age group 41-60 years – 43.90%, # above 60 year 33.60%; £ Male, female ratio – 51: 49 - almost equal; Male – M, Female – F]
The most common tumour was head & neck cancer, constituted 28.5% followed by gastro-intestinal and breast cancer 20% and 14.87% respectively. Head & neck, gastro-intestinal and hepato-biliary malignancies consisted of 57% of all malignancies (Table 3).
| Subsites | Frequency | Percent |
| H/N* | 228 | 28.5 |
| GI* | 160 | 20 |
| Breast | 119 | 14.87 |
| GYN | 75 | 9.37 |
| HB | 68 | 8.5 |
| Hematolymphoid | 39 | 4.87 |
| GU | 33 | 4.13 |
| Lung | 23 | 2.87 |
| LE | 15 | 1.87 |
| Skin | 9 | 1.13 |
| UE | 7 | 0.87 |
| CUP | 7 | 0.87 |
| CNS | 6 | 0.75 |
| Thorax | 4 | 0.5 |
| RP | 2 | 0.25 |
| Double malignancy | 2 | 0.25 |
| Unknown | 3 | 0.37 |
| Total | 800 | 100 |
[*Head & Neck cancer / GI cancer – 228/160; H/N – Head & Neck, GI – Gastro-intestinal, HB – Hepato-biliary, GU – Genio-urinary, LE – Lower extremity, UE – upper extremity, CUP – Carcinoma of unknown origin, CNS – Central-nervous system, RP – Retro- peritoneal]
441 patients (55.12%) were presented with advanced staged [Stage III & IV] disease. Whereas only 8.37% and 16.13% of patients were present in stage I and stage II disease respectively. 20.37% of staging data was missing due to multiple reasons (Table 4).
| Stages | |||||
| Subsites | I | II | III | IV | Missing |
| HN | 37 | 36 | 32 | 86 | 37 |
| GI | 4 | 18 | 38 | 69 | 31 |
| Breast | 6 | 43 | 27 | 29 | 14 |
| GYN | 14 | 5 | 21 | 20 | 15 |
| HB | 1 | 9 | 6 | 35 | 17 |
| Hemat | 2 | 11 | 6 | 8 | 12 |
| GU | 1 | 4 | 6 | 19 | 3 |
| LUNG | - | - | 2 | 19 | 2 |
| MISC | 2 | 3 | 4 | 11 | 35 |
| Total | 67 (8.37%) | 129 (16.13%) | 142 (17.75%) * | 299 (37.37%) * | 163 (20.37%) # |
[*Stage 3 & 4 – 57.74%, # missing data 20.37%; TNM AJCC 8th edition, FIGO etc. H/N – Head & Neck, GI – Gastro-intestinal, HB – Hepato-biliary, GU – Genio-urinary, Hemat – Haematolymphoid, MISC – miscellaneous]
The treatment plan was decided by tumor board committee (TBC) and 57.6% patients were advised for surgery, 45% systemic therapy, 32.1 % radiotherapy and 14.5% palliative care (Figure 1).
Figure 1. Treatment Plan as Per Tumour Board’s Recommendations.
Those patients received treatment either at KIMS Cancer Centre (KCC) or outside hospital. 420 patients (52.5%) received treatment at KCC, and 214 patients (26.75%) took treatment at outside hospitals whereas 20.75% patients’ status were unknown. After 2 years, at the time of analysis median follow up was 7.2 months. Among 800 patients, 423 patients (52.87%) were still alive with or without disease and 125 patients (15.63%) were died and rest of the patients (31.5%) were loss to follow up (Table 5).
| Treatment taken | ALIVE# | DEATH | LOST TO FOLLOW UP (LTF) | Frequency (Percent) |
| KIMS* | 291 | 58 | 71 | 420 (52.5) |
| Outside KIMS | 131 | 66 | 17 | 214 (26.75) |
| Unknown | 1 | 1 | 164 | 166 (20.75) |
| Total | 423 (52.87%) | 125 (15.63%) | 252 (31.5%) | 800 (100) |
[* treatment compliance – 52.5%; # alive 52.87%; KIMS - Kalinga Institute of medical Sciences]
Discussion
This analysis gave us some notable information about patient care and patient compliance at private comprehensive cancer care hospital in eastern India. This study showed that multidisciplinary tumour board acts as a place for group consultation regarding each stapes of cancer management [14]. It ensures more evidence-based treatment in this part of India where the concept of tumour board and multidisciplinary care of cancer patient is not very common practice. There is no supporting published article on tumour board audit from this geographic area.
Tumour board practice was started in this hospital for the first time and 800 patients were discussed in 1st year.
By this audit we came to know that the disease prevalence is almost similar in both sexes and highest number of patients (44%) were in productive life (40 years - 60years) which are younger age group of people as per worldwide data. But at the same time life expectancy in India is average which is around 70 years in 2019 as per published data [15]. Among the departments, surgical oncology had presented the highest number of patients followed by medical oncology. Head & neck cancer had highest number of cases followed by gastro-intestinal (GI) cancer and breast cancer which is not matching with the prevalence scenario of India or world. Among GI cancer, stomach cancer has highest prevalence, total number was 67 (8.37%) which is also higher than the predicted prevalence (6.3%) of India [16]. The conflicting presentation of cancer incidence is suggestive of differential referral of particular type of cancer and lack of participation of the other departments. In this analysis we noted locally advanced cases were discussed more in the TBC owing to complex nature of their management. More than 50% of patients were presented in advanced staged disease due to complex nature of disease and require opinion from multidisciplinary team for proper management. During analysis the following reasons were found out for more than 20% missing data in the staging parameter – i) patients were treated outside without proper staging workup, ii) incomplete treatment followed by recurrence, and iii) patients discussed in the TBC before complete staging work up. The highest number of recommendations of TBC were surgery, which was approximately 57.6% as the surgical oncology had presented the highest number of cases, followed by systemic therapy which was 45%. In this analysis we found that 32.1% patients were advised for radiotherapy which is higher than actual radiotherapy utilisation rate (aRTU) of India. Being a low- and middle-income country (LMIC), in India where optimal radiotherapy utilisation rate should be more than 50%, but actual radiotherapy utilisation rate is 28% [17]. Treatment compliance in cancer patients is not up to the mark in this part of the country and its true picture is unknown due to lack of published literatures. In one study [13] on head and neck cancer patients from north India has shown treatment compliance in a tertiary cancer centre approximately is 56%. The reasons of non-compliance are illiteracy, poor socio-economic conditions, long distance from hospital etc [18]. But in our hospital treatment compliance of cancer patient after TBC meeting is approximately 80%. Despite 26.75% of patients being treated outside hospital, more than 50 % of patients took treatment in this hospital. Which is a good number for an upcoming comprehensive cancer centre. 20.75% of patients’ data were missing as they discontinued follow up here after 1st visit/ TBC meeting and could not be traced out for further details. This problem can be managed by proper documentation of contact details of the patients, utilisation of manpower and good coordination with the patients during their treatment with the help of the patient care coordinator [19]. In this study patients’ follow up ranges from 0 to 3.7 years and median follow up was 7.2 months. At the time of analysis more than 50 % of patients were alive given that most of the patients had advanced staged disease. Approximately 15% of patients were dead at the time of analysis and the cause of death were disease progression more than 95% of cases. 31.5% of patients were lost to follow-up after or during taking treatment and that can also be improved by proper coordination with the patient. One of the biggest limitations of this analysis was missing data (approximately 20%), which should not be more than 10% to make a successful audit. Follow up should be robust with proper documentation and it needs participation of all the clinical departments who are practicing oncology.
This audit has few salient features which may impact the practice of oncology in this region in future. Incorporation of tumour board meeting in the management of cancer patients will become common practice. Because of that more and more of patient will get evidence-based treatment. As the stomach cancer incidence is comparatively high in this region and most of the patient comes in locally advanced stage, we can design a study trial on neoadjuvant treatment for this type of patients. This TBC meeting patient list is working as a type of cancer registry with follow up details, by which in future with a greater number of patients we shall have robust analysis and shall be able to find out it’s true impact on cancer management.
In conclusion, an advanced, complex treatment plan benefits greatly from a multidisciplinary tumor board decision, which is advised for the care of cancer patients. With enhanced treatment compliance among tumour board patients, this audit from eastern India has demonstrated the regional pattern of cancer incidence and presentation in this area. With the right use of personnel (a patient care coordinator), compliance can be improved. The meeting has daily participation from the key oncology departments, but it will be more effective if the other departments attend as well. The true impact of multidisciplinary care should be evaluated in the future in a prospective trial with a larger patient population and full follow-up information (missing data should be fewer than 10%).
References
- Max Roser and Hannah Ritchie (2021) - "Burden of Disease". Published online at OurWorldInData.org. Retrieved from: 'https://ourworldindata.org/burden-of-disease' .
- Tumor boards: optimizing the structure and improving efficiency of multidisciplinary management of patients with cancer worldwide El Saghir NS , Keating NL , Carlson RW , Khoury KE , Fallowfield L. American Society of Clinical Oncology Educational Book. American Society of Clinical Oncology. Annual Meeting.2014. CrossRef
- Implementing a Multidisciplinary Tumor Board in the Community Practice Setting Lesslie M, Parikh JR . Diagnostics (Basel, Switzerland).2017;7(4). CrossRef
- Role of multidisciplinary neuro-oncology tumour boards in cancer management Bajwa MH , Bakhshi SK , Shamim MS . JPMA. The Journal of the Pakistan Medical Association.2021;71(9).
- Multidisciplinary cancer conferences: a systematic review and development of practice standards Wright FC , De Vito C, Langer B, Hunter A. European Journal of Cancer (Oxford, England: 1990).2007;43(6). CrossRef
- The impact of multidisciplinary team meetings on patient assessment, management and outcomes in oncology settings: A systematic review of the literature Pillay B, Wootten AC , Crowe H, Corcoran N, Tran B, Bowden P, Crowe J, Costello AJ . Cancer Treatment Reviews.2016;42. CrossRef
- Quality of care management decisions by multidisciplinary cancer teams: a systematic review Lamb BW , Brown KF , Nagpal K, Vincent C, Green JSA , Sevdalis N. Annals of Surgical Oncology.2011;18(8). CrossRef
- Is it worth reorganising cancer services on the basis of multidisciplinary teams (MDTs)? A systematic review of the objectives and organisation of MDTs and their impact on patient outcomes Prades J, Remue E, Hoof E, Borras JM . Health Policy (Amsterdam, Netherlands).2015;119(4). CrossRef
- Improving decision making in multidisciplinary tumor boards: prospective longitudinal evaluation of a multicomponent intervention for 1,421 patients Lamb BW , Green JSA , Benn J, Brown KF , Vincent CA , Sevdalis N. Journal of the American College of Surgeons.2013;217(3). CrossRef
- Higher number of multidisciplinary tumor board meetings per case leads to improved clinical outcome Freytag M, Herrlinger U, Hauser S, Bauernfeind FG , Gonzalez-Carmona MA , Landsberg J, Buermann J, et al . BMC cancer.2020;20(1). CrossRef
- Multidisciplinary tumor boards and their analyses: the yin and yang of outcome measures Engelhardt M, Ihorst G, Schumacher M, Rassner M, Gengenbach L, Möller M, Shoumariyeh K, et al . BMC cancer.2021;21(1). CrossRef
- Multidisciplinary clinic care improves adherence to best practice in head and neck cancer Kelly SL , Jackson JE , Hickey BE , Szallasi FG , Bond CA . American Journal of Otolaryngology.2013;34(1). CrossRef
- Analysis of 2167 head and neck cancer patients' management, treatment compliance and outcomes from a regional cancer centre, Delhi, India Mohanti BK , Nachiappan P, Pandey RM , Sharma A, Bahadur S, Thakar A. The Journal of Laryngology and Otology.2007;121(1). CrossRef
- Practice and Impact of Multidisciplinary Tumor Boards on Patient Management: A Prospective Study Charara RN , Kreidieh FY , Farhat RA , Al-Feghali KA , Khoury KE , Haydar A, Nassar L, Berjawi G, Shamseddine A, El Saghir NS . Journal of global oncology.2016;3(3). CrossRef
- Max Roser, Esteban Ortiz-Ospina and Hannah Ritchie (2013) - "Life Expectancy". Published online at OurWorldInData.org. Retrieved from: 'https://ourworldindata.org/life-expectancy' .
- Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries Sung H, Ferlay J, Siegel RL , Laversanne M, Soerjomataram I, Jemal A, Bray F. CA: a cancer journal for clinicians.2021;71(3). CrossRef
- Radiotherapy utilization in developing countries: An IAEA study Rosenblatt E, Fidarova E, Zubizarreta EH , Barton MB , Jones GW , Mackillop WJ , Cordero L, et al . Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2018;128(3). CrossRef
- Compliance With Radiotherapy Treatment in an Apex Cancer Center of India R Khanna N, Ghosh Laskar S, Gupta T, Agarwal JP . JCO global oncology.2022;8. CrossRef
- The patient care coordinator role: an innovative delivery model for transforming acute care and improving patient outcomes Skillings LN , MacLeod D. Nursing Administration Quarterly.2009;33(4). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2024
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times