Small Cell Carcinoma of the Anal Canal: A Case Report and Review of Management Challenges
Download
Abstract
Extrapulmonary small cell carcinoma (EPSCC) is an uncommon malignancy, with anal canal involvement being exceptionally rare. Here, we report a case of a 63-year-old HIV-positive male presenting with small cell carcinoma of the anal canal. The case highlights the diagnostic and management challenges associated with this aggressive tumor, particularly given the limited literature and the lack of clear treatment guidelines. The patient’s presentation, treatment course, and the unique considerations are discussed in this case report.
Introduction
Extrapulmonary small cell carcinoma (EPSCC) is very rare with an incidence of 0.1 to 0.4% in the United states and the exact incidence in other regions is unknown [1]. Common sites of involvement include genitourinary, gynecologic, and gastrointestinal (GI) tract [2]. Among GI subsites oesophagus is most frequently involved followed by colorectum, while anal canal site is rare contributing to< 1% of all EPSCC [3]. Inspite of its rarity, it is of clinical importance due to its aggressive nature. Most of the patients present with lungs and liver metastasis at diagnosis even in early stage tumors only involving mucosa or submucosa [4]. In a study by Bernick et al, distant metastases at presentation was seen in 69% of the patients. Also, early relapses are seen in case reports within 10 to 12 months of end of treatment with most patients succumbing to the disease. It has a dismal survival rate of 58% at 6-month and 6% at 5-years [5] in contrast to squamous cell carcinoma of anal canal which has 5 year survival of 50-60% for locoregionally advanced stages [6]. Further, recent studies have shown that GI location of EPSCC is associated with a poor prognosis compared to other sites like head and neck and breast [7]. The impact of anatomic location on outcomes is probably due to earlier diagnosis. Exact ethiopathogenesis is unknown. Association with HIV has been seen like squamous cell carcinoma of anal canal [4, 8-10]. However, there is no evidence that HIV or any other virus contributes to the pathogenesis. Due to its rarity and unusual presentation, diagnosis is usually delayed resulting in delay in initiation of treatment. There is very little literature evidence and management is not clear like that of squamous cell carcinoma anal canal. As it is oncologically similar to small cell carcinoma of lung, it is managed along similar lines. Here we present a case of small cell carcinoma of anal canal who presented to our institute, the challenges we faced in diagnosis and management.
Case Presentation
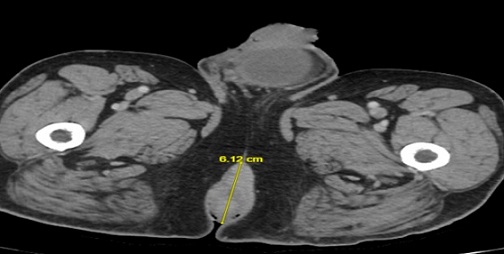
A 63 year old male patient evaluated with a one month history of occasional rectal bleeding and swelling in the anal region. During this period patient experienced increased frequency of bowel movements. There was no significant past or family history. Patient was Retropositive and was on ART. On digital rectal examination there was 3 x 3 cm mass in the anal verge with induration extending 1cm proximal to anal verge. There were no features of bowel obstruction. Contrast enhanced CT imaging revealed an ill defined large exophytic heterogeneously enhancing mass involving anal canal extending posteriorly to the perineum approximately measuring 6.1 x 3.8 cm (Figure 1).
Figure 1. Contrast Enhanced CT Imaging of Pelvis Showing Lesion Involving anal Canal Posteriorly Extending to the Perineum.
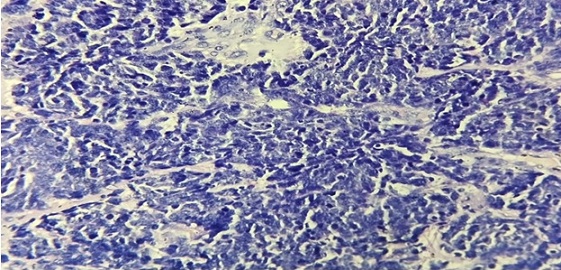
Imaging also showed bilateral metastatic inguinal and bilateral metastatic external iliac lymph nodes. Imaging did not show any other abnormal finding elsewhere. Biopsy was done from the anal canal lesion and FNAC from bilateral inguinal lymph nodes. The histopathology showed small malignant cells with hyperchromatic nuclei and scanty cytoplasm on haematoxylin and eosin staining (Figure 2).
Figure 2. Haematoxylin and Eosin Staining Demonstrating Small Malignant Cells with Hyperchromatic Nuclei and Scanty Cytoplasm.
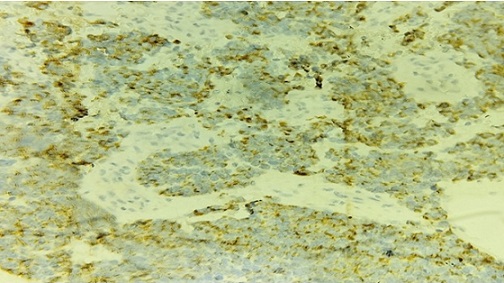
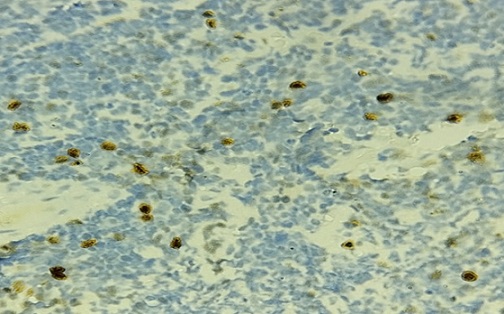
On immunostaining, the malignant cells were strongly positive for Synatophysin (Figure 3) and showed weak focal positivity for CK (Figure 4).
Figure 3. IHC Showing Positive Immunoreactivity for Synaptophysin.

Figure 4.IHC Showing Weak Focal Positivity for Cytokeratin.
There was negative staining for p63 and Chromogranin. Ki 67 was 30-40% (Figure 5).
Figure 5. Negative IHC Staining for p63 and Chromogranin.
In view of these findings it was reported as Small cell carcinoma. FNAC from bilateral inguinal lymph nodes were reported as metastatic small cell carcinoma. Case was staged as T3N1cM0 after staging work up.
Since it was a non metastatic disease, case was discussed in Multispeciality Board and patient was offered radical intent treatment. Patient was treated with Definitive chemoradiation. Radiotherapy dose given was 54 Gy in 30 fractions. During the course of RT patient was given 2 cycles of concurrent chemotherapy with Cisplatin and Etoposide combination. After completion of Definitive chemoradiation patient was given two more cycles of adjuvant chemotherapy with Cisplatin and Etoposide. After completion of treatment patient was on follow up. After eight months, patient did not turn up for further follow up. During the follow up period there were no findings suggestive of disease recurrence.
Discussion
Anal cancers are relatively rare and when diagnosed are usually squamous cell carcinomas (74%) or adenocarcinomas (19%) for which the treatment is well established. Less commonly seen histologies are basaloid carcinoma, melanoma and leiomyosarcoma. Small cell carcinomas is extremely rare with less than 1% of anal cancers [11].
A review of literature showed only 544 cases of gastro-intestinal small cell carcinomas reported in English literature till 2004. In a study in US veterans population by Mabye et al, no small-cell cancer was seen among 204 anal cancer patients. However, Boman et al reported the highest number of cases, accounting for 13 of 188 cases. Similarly in our institute out of the 19 patients who underwent curative treatment only one patient had a one patient had small cell carcinoma, rest all were Squamous cell carcinoma.
The predominant literature on this disease is largely limited to a handful of case reports. Though extremely rare, is clinically important because of its tendency for early relapse despite initial good response to treatment. Small cell carcinoma is a high-grade poorly differentiated malignancy with neuroendocrine differentiation. They constitute an aggressive group of malignancy and commonly arises in lungs constituting 20% of all lung cancers. In lungs, they arise from argyrophilic cells in the basal layer of squamous epithelium. They may be associated with ectopic production of hormones, including parathormone, secretin, granulocyte colony stimulation factor, and gastrin releasing peptide and often present with systemic symptoms.
Some authors feel these carcinomas are similar to other neuroendocrine tumors, while others suggest an embryologic origin that is still unproven. Three theories have been forwarded to explain the origin of EPSCC: They arise from enteric neuroendocrine cells from the neural crest, pleuripotent stem cells derived from endoderm, or from cells that arise from organ specific cancers when certain clones reach end stages of genetic change [11, 12]. The exact histogenesis however is controversial; however, the second and third theories seems attractive because they provide a reason for why EPSCC of the GI tract. Many reports of EPSCC arising throughout the GI tract describe the lesions occurring next to or within adenomas [13]. It is not known if any life-style-related risk factors exist. Smoking is frequently associated with SCLC, but approximately 30% of patients with EPSCC are nonsmokers [14]. Association with HIV infection has also been reported [4, 8-11].While there is a strong association of HPV and HIV with the development of squamous cell carcinoma of anal canal, the risk factors for development of anal small cell carcinoma are not well established. In our case too, the patient was HIV positive on ART and treatment was initiated after checking if CD4 count was adequate.
Nakahara et al (1993) reported a 48-year-old HIV positive homosexual male with CD4 cell count of 530/μl presenting with upfront metastatic small-cell anal cancer that responded well to chemotherapy [4]. Chapet et al (2001) presented two women with small-cell anal cancer that metastasized quickly despite chemotherapy and radiation. Although the evolution was unfavorable in the latter cases, the first patient who was HIV positive had a complete response from chemotherapy with cisplatin and etoposide.
Pathologically these tumors are poorly differentiated carcinoma with unique cytoarchitectural features. These tumors are mostly immunoreactive for markers of neuroendocrine differentiation like Chromogranin, Synaptophysin and Neuron specific enolase [5]. In our case also the malignant cells were strongly positive for Synaptophysin.
These cancers commonly presents with widespread dissemination. Even patients with initial local disease progress rapidly with distant systemic metastases to lungs or liver. Our patient presented with locoregional disease with bilateral inguinal nodes without development of lung or liver metastasis. This is probably because of typical presentation with perianal mass and bleeding PR resulting in early diagnosis and treatment initiation.
Due to the rarity of this tumour entity, there are no prospective trials to guide management. As small cell carcinomas of anal canal are oncologically similar to their counterparts in lungs they are treated along the same lines, which concurrent chemoradiation. RT doses given are usually 54 Gy in 30 fraction with 2 cycles concurrent cisplatin and etoposide. Other agents like cyclophosphamide, doxorubicin with cisplatin have also been used. Consolidation chemotherapy is considered with possible improvement in DFS.
A single-center retrospective study of 120 patients with predominantly non-metastatic EPSCC had comparable survival to patients with limited disease small cell lung cancer treated at the same institution [14]. Another retrospective study of 5,747 patients with EPSCC from the National Cancer Database between 2006–2014 found that concurrent chemoradiation improved overall survival compared to chemotherapy or radiation alone [15]. These findings have led to the adoption of the treatment approach for small cell lung carcinoma to the management of EPSCC. There is typically a good response to chemoradiation that is shortly followed by relapse or rapid progression to lung or liver with a median survival of only 6-12 months [1]. The response to chemotherapy is usually 70% to 90% but transient. Many patients had rapid disease progression and nearly all patients had an overall survival of less than 12 months from diagnosis.
In our case, the patient had initial good response to concurrent chemoradiation with 54 Gy and 2 cycles 4 weekly Cisplatin/Etoposide. In other case reports too, similar RT dose of 54 Gy/30 fractions to primary and 47Gy/27 fractions to inguinal nodes was administered with 2 to 3 cycles Cisplatin/Etoposide [14]. Our patient tolerated the treatment well without treatment breaks, and no grade 3 toxicity other than dermatitis.
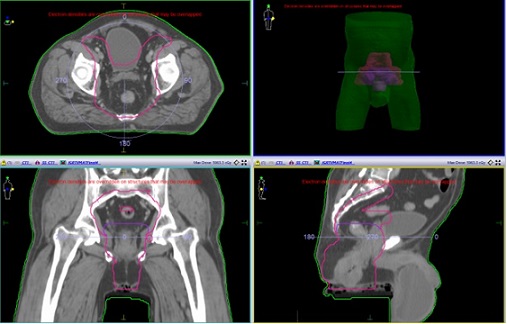
Chuang et al (2021) [7] treated the patient with a higher dose of 59 Gy in 32 fractions (45 Gy followed by 14 Gy boost to gross tumor) using helical tomotherapy to cover mesorectum, bilateral inguinal, external and internal iliac, and common iliac lymph nodes, along with 2 cycles concurrent Cisplatin/ Etoposide. Given concern for high risk of relapse, the patient was treated with an additional four cycles of consolidation chemotherapy with cisplatin / etoposide [7]. The patient did not have recurrence or relapse at 3 years follow up. In our patient also the treatment volume included mesorectum, bilateral inguinal, external and internal iliac, presacral and common iliac lymph nodes to a dose of 45 Gy followed by 9 Gy boost to deliver a total dose of 54 Gy to Gross tumor in the anal canal and gross nodes in bilateral inguinal region as shown in Figure 6.
Figure 6. Figure Showing Low Dose and High Dose Planning Target Volumes Treated to 45 Gy and 54 Gy Respectively.
In our patient, Radiotherapy dose given was 54 Gy in 30 fractions with 2 cycles of concurrent chemotherapy with Cisplatin and Etoposide followed by two more cycles of adjuvant chemotherapy with Cisplatin and Etoposide. Patient was disease free for eight months, after which he did not turn up for further follow up. However, local or distant relapse might have been seen if there was longer follow-up. Radiotherapy can also be considered for palliation. Prognosis remains poor because of the aggressive nature of the malignancy.
While small cell carcinoma of the lungs has a predilection for central nervous system involvement, EPSCC has been shown to have a lower risk of CNS metastases [1]. Therefore, prophylactic cranial irradiation has not been widely adopted in the treatment of EPSCC.
In conclusion, small cell anal carcinoma is a rare an poorly understood entity with sparse data to guide management of this aggressive disease. Risk of relapse is high despite treatment with concurrent chemoradiation. An aggressive approach with addition of consolidation chemotherapy to chemoradiation may offer prolonged disease-free survival and improved overall survival. Further studies will be required to delineate the risk factors and better define the treatment approach for this rare entity.
References
- Extrapulmonary small-cell carcinoma compared with small-cell lung carcinoma: a retrospective single-center study Cicin I, Karagol H, Uzunoglu S, Uygun K, Usta U, Kocak Z, Caloglu M, et al . Cancer.2007;110(5). CrossRef
- Small-cell carcinomas of the gastrointestinal tract: a review Brenner B, Tang LH , Klimstra DS , Kelsen DP . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2004;22(13). CrossRef
- Small cell carcinoma of the esophagus. The Massachusetts General Hospital experience, 1978 to 1993 Huncharek M, Muscat J. Chest.1995;107(1). CrossRef
- Small cell carcinoma of the anus in a human HIV carrier: report of a case Nakahara H, Moriya Y, Shinkai T, Hirota T. Surgery Today.1993;23(1). CrossRef
- Neuroendocrine carcinomas of the colon and rectum Bernick PE , Klimstra DS , Shia J, Minsky B, Saltz L, Shi W, Thaler H, et al . Diseases of the Colon and Rectum.2004;47(2). CrossRef
- Neuroendocrine cancers of the colon and rectum. Results of a ten-year experience Saclarides TJ , Szeluga D, Staren ED . Diseases of the Colon and Rectum.1994;37(7). CrossRef
- Locally advanced anal small cell carcinoma with durable complete response to chemoradiation followed by consolidation chemotherapy: case report and literature review Chuang J, Wang C, Parekh V, Fakih M. Journal of Gastrointestinal Oncology.2021;12(6). CrossRef
- Small cell cancer of the anal canal--case report of a rare tumor Meyer A, Bruns F, Richter K, Grünwald V, Karstens JH . Anticancer Research.2007;27(2).
- Small Cell Carcinoma of Anal Canal - A Rare Case Report Surag , Neeralagi C, Prasath A, Kumar P, Reddy B. Journal of Clinical and Diagnostic Research : JCDR.2016;10(9). CrossRef
- Detection of human papillomavirus in small cell carcinomas of the anus and rectum Cimino-Mathews A, Sharma R, Illei PB . The American Journal of Surgical Pathology.2012;36(7). CrossRef
- Should extrapulmonary small cell cancer be managed like small cell lung cancer? Brennan SM , Gregory DL , Stillie A, Herschtal A, Mac Manus M, Ball DL . Cancer.2010;116(4). CrossRef
- The cytochemistry and ultrastructure of polypeptide hormone-producing cells of the APUD series and the embryologic, physiologic and pathologic implications of the concept Pearse AG . The Journal of Histochemistry and Cytochemistry: Official Journal of the Histochemistry Society.1969;17(5). CrossRef
- Small-cell carcinoma of the gastrointestinal tract: a retrospective study of 64 cases Brenner B, Shah MA , Gonen M, Klimstra DS , Shia J, Kelsen DP . British Journal of Cancer.2004;90(9). CrossRef
- Extrapulmonary small cell carcinoma of the anal canal: a case report and review of the literature Eberhardt JM , Brown K, Lo S, Nagda S, Yong S. Case Reports in Medicine.2012;2012. CrossRef
- Extrapulmonary small cell carcinoma: Prognostic factors, patterns of care, and overall survival Mandish SF , Gaskins JT , Yusuf MB , Little BP , Dunlap NE . European Journal of Surgical Oncology: The Journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology.2020;46(9). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2024
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times