The Incidence of Unnecessary Pancreatic Resections for Non-Cancerous Lesions: A Retrospective Study in a Thai Tertiary Hospital
Download
Abstract
Background: Pancreatic and peri-ampullary cancers are aggressive malignancies requiring surgical intervention. However, certain non-cancerous conditions can mimic these cancers on imaging, leading to unnecessary pancreatic resections. This retrospective study investigated the incidence of non-cancerous lesions removed during pancreatic resections for suspected pancreatic or peri-ampullary cancers in a tertiary hospital in Thailand.
Materials and Methods: This retrospective review was conducted on 148 patients who underwent pancreatic resection between January 2013 and December 2017 at Srinagarind Hospital, Khon Kaen University. Medical and pathological data were analyzed to determine the proportion of patients with non-cancerous lesions.
Results: Nine patients (6.1%) had a postoperative diagnosis of a non-cancerous condition not requiring surgical intervention. The rate of unnecessary resections was significantly higher in patients undergoing distal pancreatectomy or enucleation (15%, 4/27) compared to those undergoing pancreaticoduodenectomy (4.1%, 5/121). While clinical features were similar between patients with cancerous and non-cancerous diagnoses for pancreaticoduodenectomy, a significant difference was observed in gender (p=0.031). No significant clinical differences were found between the two groups after distal pancreatectomy or enucleation.
Conclusion: This study highlights the occurrence of unnecessary pancreatic resections for non-cancerous lesions in a Thai setting. The prevalence of these cases, particularly for distal pancreatectomy and enucleation, suggests the need for careful evaluation and diagnostic strategies to minimize unnecessary surgeries. The findings also highlight potential geographical differences in the types of non-cancerous conditions mimicking pancreatic and peri-ampullary cancers, with Eastern countries experiencing a higher prevalence of ampullary and bile duct conditions compared to Western countries. Further research is needed to develop improved diagnostic tools and refine surgical decision-making processes in this complex clinical setting.
Introduction
Pancreatic and peri-ampullary cancer are malignancy that have the potential to be fatal and necessitates surgical intervention. Since pancreatic resection, whether it be pancreaticoduodenectomy or distal pancreatectomy, can result in a wide variety of life-threatening complications, a correct preoperative diagnosis is essential. However, similar to other hepatobiliary lesions [1], some non-cancerous conditions especially those that do not require surgical removal, exhibit imaging features that resemble those of pancreatic and peri-ampullary cancer. Due to the difficulty in obtaining a preoperative histological diagnosis of certain pancreatic diseases.
As a result, patients with imaging findings that make it impossible to rule out pancreatic or peri-ampullary cancer are typically advised to undergo pancreatic resection. Based on prevailing surgical practices and guidelines, it is generally not recommended to obtain routine preoperative histologic proof of primary resectable pancreatic solid lesions [2, 3]. This is due to the associated risks and the limited reliability of most sampling techniques in accurately predicting negative outcomes. However, exceptions may be made in cases where patients are deemed unfit for major surgery or when alternative diagnoses need to be ruled out [2, 3].
As far as we are aware, there is limited evidence regarding the proportion of non-cancerous lesions masquerading as pancreatic and peri-ampullary cancers. Previous studies have demonstrated that the prevalence of incongruity between clinical suspicion and histological findings were various from roughly 4-13% [4, 5]. However, in certain series, this discrepancy might be as high as 35%
[6] and there was no observed trend of reduction over time [4, 7]. It could perhaps be linked to the geographical variability of a prevalent, non-malignant condition. For instance, autoimmune pancreatitis appears to be prevalent in Western countries. Although there have been many reports regarding the topic at hand. The scarcity of data regarding the proportion of non-cancerous lesions that undergo pancreatic resection for suspected pancreatic or peri-ampullary cancer is particularly evident in countries with a high incidence of other types of peri-ampullary cancer, such as cholangiocarcinoma in Southeast Asia.
To gain a better understanding of the non-cancerous lesions that masquerade as pancreatic or peri-ampullary cancer in Eastern country, the purpose of this study was to determine the proportion of non-cancerous lesions undergoing pancreatic resection for suspected pancreatic or peri-ampullary cancer. In particular, we investigated the distinctions in characteristics that exist between benign conditions and pancreatic cancer, categorize to their locations.
Materials and Methods
The retrospective study was conducted over a period spanning from January 2013 to December 2017. We examined the medical and pathological data of 148 individuals who underwent pancreas resection at Srinagarind Hospital, Khon Kaen University.
Our center is a tertiary care center where the patients are referred for on hepato-pancreato-biliary malignancy. Regarding the treatment plan for patients at our center who were identified as having a pancreatic lesion, at least one method of cross-sectional imaging (CT or MRI) was utilized to make the diagnosis for each individual patient. Those patients with imaging characteristics that could not preclude the possibility of cancer would undergo surgery. Endoscopic ultrasound is typically employed solely in cases where an indeterminate lesion has been identified and the outcome would have an impact on the course of treatment. Once the diagnosis has been made and the resectability has been assessed intraoperatively, the patients underwent pancreatic resection with the intention of achieving gross tumor excision. The selection of the surgical procedure is contingent upon the tumor’s location and the preoperative diagnosis. All surgical specimens were forwarded to the Department of Pathology for pathological evaluation and final staging.
Outcome variables
The primary outcome was the proportion of the patients with conditions did not necessitate surgical intervention, who underwent pancreatic resection for presumed pancreatic or peri-ampullary cancer. The introduction of the concept of “concordant - discordant” was instrumental in establishing a precise outcome parameter. The patients were then divided into “concordant” and “discordant” groups based on whether the postoperative pathological diagnosis revealed conditions that did or did not require surgical resection. In addition, we assessed the disparities in patient characteristics between those who underwent pancreaticoduodenectomy and those who underwent other procedures.
Definition of conditions did not necessitate surgical intervention encompassed various conditions such as a histologically confirmed small (<5mm) low- grade neuroendocrine tumor, branch duct intraductal papillary mucinous neoplasm measuring less than 3 cm, small asymptomatic serous cystic neoplasm, and all asymptomatic benign lesions with no malignant potential. The definitions provided by the International Study Group (ISGPS) were used to classify postoperative pancreatic fistula (POPF) [8], post-pancreatectomy hemorrhage (PPH) [9], and delayed gastric emptying (DGE) [10].
Statistical analyses
The data are displayed as medians (min: max) or counts and percentages. The statistical technique of Kaplan-Meier analysis was utilized to demonstrate survival analysis. The log-rank test was employed to analyze the comparisons made among groups. The analysis excluded patients who experienced perioperative mortality, which was defined as death occurring within 30 days following the surgical procedure. A p-value of less than 0.05 was considered to be statistically significant. All statistical analyses were performed using STATA version 13.
Ethical consideration
This study was approved by the Institutional Review Board (IRB), Office of Human Research Ethics, Khon Kaen University (HE631175) .
Results
Out of the 148 patients who received surgical interventions for preoperative diagnoses of pancreatic cancer, a total of 9 patients (6.1%) were identified to have conditions that did not necessitate surgical intervention upon postoperative pathological diagnosis. The proportion of patients in the discordant group was significantly greater among those who underwent distal pancreatectomy or enucleation (15%, 4/27) than among those who underwent pancreaticoduodenectomy (4.1%, 5/121) (Figure 1).
Figure 1. Proportion of Pancreatic Resection for Non-cancerous Lesions.
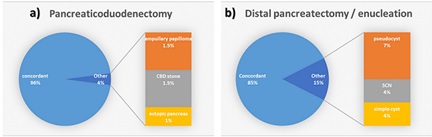
In the cohort of patients who underwent pancreaticoduodenectomy, there were five patients with discordant diagnosis. Among these, the final diagnosis encompassed two ampullary papilloma, two common bile duct stones, and one ectopic pancreas. There were no significant differences in clinical characteristics were observed between the concordant and discordant groups, except for gender (p=0.031). Notably, the discordant group did not include any male patients (Table 1).
| Variables | Discordant | Concordant | p value |
| n =5 | n = 116 | ||
| n (%) or mean (SD) | n (%) or mean (SD) | ||
| Age (mean. sd) | 59.5 | 59.33 | 0.9765 |
| Gender (male) | 0 | 64 (55.2%) | 0.031* |
| BMI | 25.21 (16.13-34.29) | 37.22 (22.02-52.41) | 0.7737 |
| DM | 0 | 24 (20.7%) | 0.312 |
| CKD | 0 | 3 (2.59%) | 0.746 |
| HT | 1 (20%) | 28 (24.1%) | 0.961 |
| Location | 0.422 | ||
| - Head | 0 | 19 (16.4%) | 0.38 |
| - Uncinate | 0 | 8 (6.9%) | 0.588 |
| - Neck | 0 | 2 (1.7%) | 0.792 |
| - Common bile duct | 2 (40%) | 37 (31.9%) | 0.439 |
| - Ampulla | 2 (40%) | 46 (39.7%) | 0.563 |
| - Duodenum | 1 (20%) | 5 (4.3%) | 0.06 |
| Preopearative laboratory | |||
| TB | 7.125 (-6.32-20.57) | 6.73 (5.11-8.36) | 0.9284 |
| AST | 63.25 (19.22-107.28) | 91.26 (66.31-114.2) | 0.6456 |
| ALT | 69.25 (-11.59-150.09) | 89.21 (66.08-112.33) | 0.7454 |
| ALP | 269.5 (32.16-506.83) | 402.83 (318.2-487.46) | 0.5532 |
| Alb | 3.78 (2.93-4.62) | 3.67 (3.54-3.8) | 0.7718 |
| Cholesterol | 198.25 (123.68-272.82) | 253.44 (218.2-288.68) | 0.5553 |
| Operative Procedure | |||
| Classic Whipple | 1 (20%) | 19 (16.4%) | 0.643 |
| PPPD | 3 (60%) | 91 (78.4%) | 0.896 |
| PRPD | 0 | 7 (6.0%) | 0.614 |
| Laparoscopic procedure | 0 | 7 | 0.614 |
| EBL (ml) | 627.5 (362.7-892.29) | 558.09 (436.78-679.39) | 0.8338 |
| Postoperative complications | |||
| POPF | 2 (40%|) | 46 (39.7%) | 0.5575 |
| Bile leak | 0 | 5 (4.3%) | 0.7077 |
| Collection | 0 | 3 (2.6%) | 0.746 |
| Chyle leak | 0 | 9 (7.8%) | 0.5642 |
| DGE | 0 | 1 (0.9%) | 0.8527 |
| 30days Mortality | 0 | 3 (2.6%) | 0.7457 |
There were no disparities in clinical characteristics between the concordant and discordant groups of patients who underwent distal pancreatectomy or enucleation (Table 2), except for BMI (p=0.046).
| Variables | Discordant | Concordant | p value |
| n = 4 | n = 23 | ||
| n (%) or mean (SD) | n (%) or mean (SD) | ||
| Age (mean. sd) | 48.5 | 51.08696 | 0.7798 |
| Gender (male) | 2 (50%) | 8 (34.78%) | |
| BMI | 20.02704 | 25.5569 | 0.0466* |
| DM | 0 | 2 (8.7%) | 0.5399 |
| CKD | 0 | 2 (8.7%) | 0.5399 |
| HT | 1 (25%) | 6 (26.09%) | 0.9635 |
| Location | |||
| - Uncinate | 0 | 1 (4.35%) | 0.6709 |
| - Neck | 0 | 2 (8.7%) | 0.5399 |
| - Body | 3 (75%) | 8 (34.78%) | 0.1308 |
| - Tail | 1 (25%) | 12 (52.17%) | 0.3154 |
| Size | 4.425 (1.24-7.6) | 4.00 (2.47-5.55) | 0.8238 |
| Preopearative laboratory | |||
| TB | 0.3 (-0.13-0.73) | 0.43(0.32-0.54) | 0.3747 |
| AST | 25 (3.77-46.22) | 29.67(21.5-37.84) | 0.6664 |
| ALT | 35 (-20.98-90.98) | 21(17.49-24.5) | 0.0335* |
| ALP | 54.33 (16.96-91.7) | 87.24(67.39-107.08) | 0.2157 |
| Alb | 4.1 (2.37-5.82) | 4.32(4.1-4.55) | 0.4859 |
| Cholesterol | 205.67 (80.6-330.72) | 187.52(169.67-205.36) | 0.4738 |
| Operative Procedure | |||
| Distal pancreatectomy | 4 (100%) | 20 (86.96%) | 0.444 |
| Enucleation | 0 | 3 (13.04%) | 0.444 |
| + splenectomy | 4 (100%) | 14 (60.87%) | 0.125 |
| Laparoscopic procedure | 0 | 5 (21.74%) | 0.302 |
| EBL (ml) | 442.5 (-156.89-1041.89) | 257.39 (183.25-331.53) | 0.1115 |
| Postoperative complications | |||
| POPF | 3 (75%) | 11 (47.83%) | 0.315 |
| Collection | 0 | 0 | |
| Chyle leak | 0 | 1 (4.35%) | 0.671 |
| 30days Mortality | 0 | 1 (4.35%) | 0.671 |
The BMI of patients in the concordant group was observed to be higher in comparison to the discordant group, with values of 25.6 and 20.0, respectively. All of the lesions in the discordant group were identified as cystic lesions, comprising two pseudocysts, one asymptomatic small SCN, and one simple cyst.
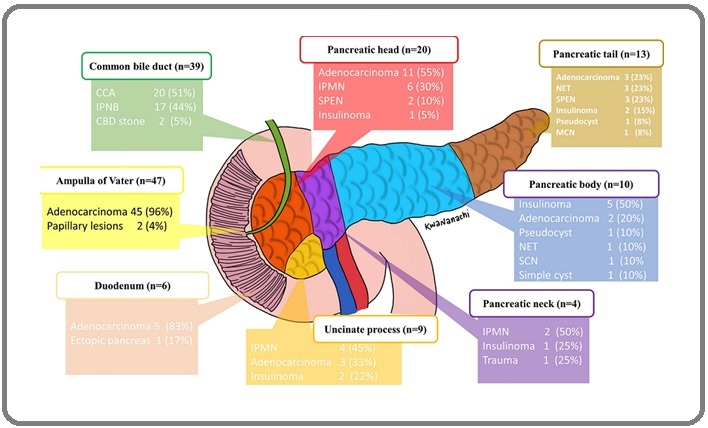
According to the location of the tumor, there were no discordant diagnoses among patients with lesions in the head, neck, and uncinate process of the pancreas. (Figure 2).
Figure 2. Schematic Illustration of Disease Necessitates Pancreatic Resection According to Location of the Lesions.
Discussion
This study revealed that a mere 6.1% of individuals preoperatively diagnosed with pancreatic and peri-ampullary cancer, who underwent pancreatic resection did not necessitate surgical resection, as confirmed by a pathological examination. This is a comparatively lower incidence rate in relation to previous research, which reported rates of unanticipated benign conditions following pancreatic resection ranging from 4% to 35% [4-6]. However, this variability may be attributed to the criteria used to define the disorders, which may not necessitate surgical resection. It is noteworthy that pancreatitis emerged as the most commonly misdiagnosed condition in Western countries [4, 7]. However, our study did not observe any instances of patients undergoing pancreatic resection for autoimmune pancreatitis. While prior findings from Western countries have indicated that the majority of benign diseases mimicking cancerous lesions are inflammatory in nature, our study did not identify any inflammatory disorders in the group we referred to as ‘discordant’.
The lower frequency of pancreaticoduodenectomy for non-cancerous lesions compared to distal pancreatectomy can be attributed to the apprehension over a higher surgical risk associated with the former procedure, as well as the ease of assessment using endoscopy. However, a significant proportion of patients still received unnecessary pancreaticoduodenectomy. This is due to the limited ability of imaging techniques and endoscopy to provide a conclusive diagnosis, thereby making it difficult to rule out the presence of malignancy. Although our findings did not yield statistically significant results, it is important to acknowledge that the discordant group had a lower body mass index, as well as lower rates of underlying diabetes mellitus and hypertension. The rationale is relatively clear, as it is commonly seen that pancreatic cancer is often accompanied by the development of new-onset diabetes mellitus. In contrast to earlier publications indicating that pancreatic conditions constitute the majority of cases undergoing pancreaticoduodenectomy for benign conditions [11], our study revealed that ampullary and bile duct lesions were the prevailing etiologies. Remarkably, there was no biliary stricture in our study, despite the notably high frequency of bile duct tumors in our geographical area [12]. All conditions of bile duct pathology that resembled malignant lesions in our study were found to be related with choledocholithiasis, which is consistent with earlier findings [11].
Given the expected lower risk associated with distant pancreatectomy and the emergence of minimally invasive surgical techniques, it is reasonable to expect an increased incidence of unnecessary distal pancreatectomy. There are several reasons why, based on our findings, the size of the lesion was not able to effectively distinguish between cancerous and non-cancerous lesions. Firstly, the majority of indications for surgical excision are not based just on the size of the lesion, but rather on its characteristics. Additionally, the distal pancreas is situated silent regions, hence allowing for the detection of only larger lesions. Remarkably, all of the lesions observed in the discordant group within our series had cystic characteristics. This finding elucidates the rationale behind the notable increase in the incidence of postoperative pancreatic fistula (POPF) seen within the discordant group. Cystic lesions are typically observed along with a soft texture of the pancreas and a small size of the pancreatic duct. These findings prompt us to reconsider the notion that pancreaticoduodenectomy is solely associated with surgical challenges, as it is no longer linked to postoperative morbidity as previously seen.
One notable discovery of our study is the presence of a significantly greater proportion of intraductal tumors in both the pancreas (intraductal papillary mucinous neoplasm of the pancreas, or IPMN-P) and the bile duct (intraductal papillary neoplasm of the bile duct, or IPNB). A total of 17 cases of IPNB and 12 cases of IPMN-P were identified. It is widely recognized that our region is a known endemic area for IPNB, as we have published one of the most extensive studies on the subject [13]. Nevertheless, there is currently no available report on the prevalence of IPMN-P in our specific location. It is postulated that there may exist a genetic association between IPNB and IPMN-P, as a considerable number of cases have been seen when both conditions manifest together [14]. Given that IPNB is widely recognized as a malignant condition [15], it is deemed reasonable to perform pancreaticoduodenectomy as a treatment approach for every cases of IPNB of common bile duct. The criteria utilized for determining the need for excision of IPMN-P at our center aligns with those employed by other centers [16].
As the safety of pancreatic resection improves with time, it is doubtful that the rate of pancreatic resection for non-cancerous tumors would decrease. It is widely recognized that cross-sectional imaging alone lacks the ability to distinguish between benign and malignant diseases clearly [5]. The use of more invasive endoscopic techniques, such as endoscopic retrograde cholangiopancreatography or endoscopic ultrasound, does not contribute to a reduction in the occurrence of non-cancerous lesions [7]. Even conducting a biopsy. The determination of malignancy cannot be reliably ruled out with an appropriate level of certainty [3]. There continues to exist a necessity for a multimodal strategy with a comprehensive assessment encompassing a meticulous analysis of the patient’s medical history, thorough physical examination, examination of serum tumor markers, and diagnostic imaging may be the sole resolution for this matter. The main cause of contributing to unnecessary pancreatic resection is an insufficient preoperative evaluation and a lack of a multidisciplinary approach to patient care [4]. These causes can be avoided. In referral hospitals such as our medical center, it is common to see inadequate imaging received from the primary hospitals. It is recommended that the availability of high-quality cross-sectional imaging be ensured prior to establishing a diagnosis for the patient. Additionally, in challenging cases, it is advisable to conduct multidisciplinary team meetings [4]. The incorporation of supplementary molecular markers in preoperative biopsy procedures may prove to be advantageous in the future [17]. However, their role at present is still unclear.
To the extent of our current understanding, this research represents the inaugural investigation aimed at establishing the proportion of unnecessary pancreatic resections undertaken for non-cancerous lesions within the region which has a high prevalence of bile duct tumors. Furthermore, we have included all individuals who underwent pancreatic resection, irrespective of the particular type of resection, in order to provide a comprehensive representation of the entire spectrum of pancreatic diseases. However, it is important to acknowledge that there were certain limitations that need to be considered. The retrospective design of the study may create selective bias, despite the fact that the criteria for pancreatic resection were established prospectively. Moreover, the available patient data did not include information regarding surgical exploration without pancreatic resection. This lack of data prevents us from determining if the decision not to do pancreatic resection was based on intraoperative evidence indicating advancement of the disease or a benign appearance of the lesions. All previous studies, including our own, have exclusively examined patients who have undergone pancreatic resection, but have not assessed the potential risk of non-resected malignant lesions in the follow-up cohort. In the future, it is recommended that a prospective research be conducted to evaluate the compromise between the potential hazards of unnecessary resection and the risk of missing cancerous lesions in patients with pancreatic and peri-ampullary lesions, regardless of whether they have had resection.
In conclusion, pancreatic resection for non-cancerous condition might be an inevitable circumstance. There exist variations in the spectrum of non-cancerous diseases that mimic pancreatic or peri-ampullary cancer between Western and Eastern countries. Pancreatic conditions, particularly inflammatory conditions, were shown to be prevalent in Western countries, but in Eastern countries, ampullary and bile duct conditions were more commonly observed in the patient undergoing pancreaticoduodenectomy and benign cystic lesion were more common in the patient undergoing distal pancreatectomy. The greater incidence of bile duct tumors in our geographical area did not have an impact on the frequency of unnecessary pancreatic resections.
References
- Benign Diseases Masquerading as Cholangiocarcinoma: Can we Differentiate before Surgery? Wannasri T, Luvira V, Wongwattanachai A, Titapun A, Srisuk T, Kamsa-ard S, Tipwaratorn T, et al . Asian Pacific Journal of Cancer Care.2022;7. CrossRef
- When to perform a pancreatoduodenectomy in the absence of positive histology? A consensus statement by the International Study Group of Pancreatic Surgery Asbun HJ , Conlon K, Fernandez-Cruz L, Friess H, Shrikhande SV , Adham M, et al . Surgery.2014;155(5). CrossRef
- Preoperative tissue diagnosis for tumours of the pancreas Hartwig W, Schneider L, Diener MK , Bergmann F, Büchler MW , Werner J. The British Journal of Surgery.2009;96(1). CrossRef
- The Rate of Avoidable Pancreatic Resections at a High-Volume Center: An Internal Quality Control and Critical Review Surci N, Rösch CS , Kirchweger P, Havranek L, Boetticher P, Fischer I, Wundsam HV , Biebl M, Függer R. Journal of Clinical Medicine.2023;12(4). CrossRef
- Unexpected benign histopathology after pancreatoduodenectomy for presumed malignancy: accepting the inevitable Gomes RM , Bal M, Patkar S, Goel M, Shrikhande SV . Langenbeck's Archives of Surgery.2016;401(2). CrossRef
- Pancreaticoduodenectomy for suspected but unproven malignancy Thompson JS , Murayama KM , Edney JA , Rikkers LF . American Journal of Surgery.1994;168(6). CrossRef
- Increased Incidence of Benign Pancreatic Pathology following Pancreaticoduodenectomy for Presumed Malignancy over 10 Years despite Increased Use of Endoscopic Ultrasound Yarandi SS , Runge T, Wang L, Liu Z, Jiang Y, Chawla S, Woods KE , et al . Diagnostic and Therapeutic Endoscopy.2014;2014. CrossRef
- The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al . Surgery.2017;161(3). CrossRef
- Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition Wente MN , Veit JA , Bassi C, Dervenis C, Fingerhut A, Gouma DJ , Izbicki JR , et al . Surgery.2007;142(1). CrossRef
- Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS) Wente MN , Bassi C, Dervenis C, Fingerhut A, Gouma DJ , Izbicki JR , Neoptolemos JP , et al . Surgery.2007;142(5). CrossRef
- Pancreaticoduodenectomy (Whipple resections) in patients without malignancy: are they all 'chronic pancreatitis'? Abraham SC , Wilentz RE , Yeo CJ , Sohn TA , Cameron JL , Boitnott JK , Hruban RH . The American Journal of Surgical Pathology.2003;27(1). CrossRef
- Decreasing trends in cholangiocarcinoma incidence and relative survival in Khon Kaen, Thailand: An updated, inclusive, population-based cancer registry analysis for 1989-2018 Kamsa-Ard S, Santong C, Kamsa-Ard S, Luvira V, Luvira V, Suwanrungruang K, Bhudhisawasdi V. PloS One.2021;16(2). CrossRef
- Long-term outcome of surgical resection for intraductal papillary neoplasm of the bile duct Luvira V, Pugkhem A, Bhudhisawasdi V, Pairojkul C, Sathitkarnmanee E, Luvira V, Kamsa-Ard S. Journal of Gastroenterology and Hepatology.2017;32(2). CrossRef
- Simultaneous Extensive Intraductal Papillary Neoplasm of the Bile Duct and Pancreas: A Very Rare Entity Luvira V, Pugkhem A, Tipwaratorn T, Chamgramol Y, Pairojkul C, Bhudhisawasdi V. Case Reports in Surgery.2016;2016. CrossRef
- Morphological Classification of Intraductal Papillary Neoplasm of the Bile Duct with Survival Correlation Luvira , Somsap K, Pugkhem A, Eurboonyanun C, Luvira V, Bhudhisawasdi V, Pairojkul C, Kamsa Ard S. Asian Pacific journal of cancer prevention: APJCP.2017;18(1). CrossRef
- Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY , Levy P, Ohtsuka T, Salvia R, et al . Pancreatology: official journal of the International Association of Pancreatology (IAP) ... [et al.].2017;17(5). CrossRef
- Molecular markers for diagnostic cytology of neoplasms in the head region of the pancreas: mutation of K-ras and overexpression of the p53 protein product Es JM , Polak MM , Berg FM , Ramsoekh TB , Craanen ME , Hruban RH , Offerhaus GJ . Journal of Clinical Pathology.1995;48(3). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2024
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times