Vulvar Melanoma in the Elderly Treated with Surgery and Rradiotherapy: A Case Report
Download
Abstract
Although rare, vulvar melanoma is the second most common histological type of vulvar cancer, representing around 10% of all malignant tumors involving the vulva presenting typically in post-menopausal women. The data on vulvar melanoma consists almost entirely of case studies and small retrospective series. A standardized approach to the diagnosis and management of vulvar melanoma is not available. In this paper, a case of vulvar melanoma in remission is described and a review of the current literature is presented. A 73-year-old, G5P5 (5-0-0-5), complained of a 3-year history of intense vaginal pruritus. A biopsy was done at the site of the hyperpigmented patch revealing vulvar melanoma. CT scan was done before surgery and revealed negative lymph node invasion nor metastasis. The patient underwent a radical vulvectomy followed by adjuvant radiotherapy which offered remission of disease for 5 years.
Introduction
Cancer of the vulva is not a common disease and accounts for at least 1 % of malignant neoplasms among women. Although rare, vulvar melanoma is the second most common histological type of vulvar cancer, representing around 10% of all malignant tumors involving the vulva presenting typically in post-menopausal women. Malignant melanomas of the vulva are rare tumors located in areas of the body not exposed to radiation and due to lack of body awareness, usually patients present with the disease at a late stage and have a poor overall prognosis and high recurrence rate. The data on vulvar melanoma consists almost entirely of case studies and small retrospective series. A standardized approach to the diagnosis and management of vulvar melanoma is not available. In this paper, a case of vulvar melanoma in remission is described and a review of the current literature is presented.
Case Report
A 73-year-old, G5P5 (5-0-0-5), known hypertensive for more than 10 years, maintained on Amlodipine 10mg/tablet one tablet once a day presented for gynecologic consultation due to intense vaginal pruritus. Past medical, family history, sexual history, and social history are non-contributory. She has an OB score of G5P5 (5-0-0-5) all carried to term by normal spontaneous delivery.
History started 3 years before admission when she experienced intense pruritus on the left labia majora with no associated foul-smelling vaginal discharges, masses, and scales on the affected area. Persistence prompted a consult with an obstetrician-gynecologist where a workup was done. She was managed as a case of candidiasis, given appropriate medications, and advised. Recurrence of signs and symptoms for 3 years prompted recurrent visits to an obstetrician-gynecologist with interventions providing temporary relief. 1 month before admission, there was noted persistence of the condition, now with a note of a soft, hyperpigmented patch on the vulvar area with irregular borders, initially about 1 cm in widest diameter with a note of gradual involvement of adjacent areas. There was associated erythema, and excoriation of the adjacent labia majora with minimal vaginal bleeding.
On physical examination, there were multiple pigmented flat patches scattered on the labia majora, with irregular borders measuring approximately 1.0 x1.0cm (Figure 1).
Figure 1. The Vulvar Area was Hyperemic with Excoriations, with Multiple Pigmented Flat Patches with Irregular Borders Measuring Approximately 1.0 x 1.0cm Scatted on the Labia Majora.

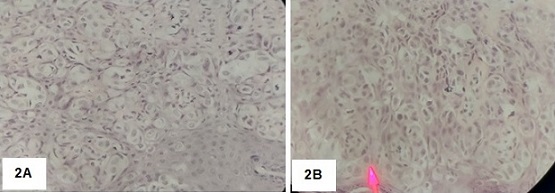
Speculum examination, bimanual examination, and digital examinations were all normal. Biopsy was done at the site of the hyperpigmented patch revealing vulvar melanoma (Figure 2A and 2B), hence she was referred to a Gyne-Oncologist for further management. Biopsy revealed a vulvar melanoma.
Figure 2. 2A and 2B. Melanocytes Showing Cytological atypia with Nuclear Enlargement, Increased Nuclear-cytoplasmic Ratios, Pleomorphism and Prominent nucleol.
CT scan was done prior to surgery and revealed negative lymph node invasion nor metastasis. The patient underwent radical vulvectomy. On surgical exploration, a 9.0cm x 9.0cm x 0.8cm layer of skin and subcutaneous tissue was removed (Figure 3, 4).
Figure 3. 9.0 9.0 x 0.8cm Layer of Skin and Subcutaneous Tissue with Irregularly Pigmented Flat Spots.

Figure 4. Post-vulvectomy Showing no Lesions on the Remaining Vulva.

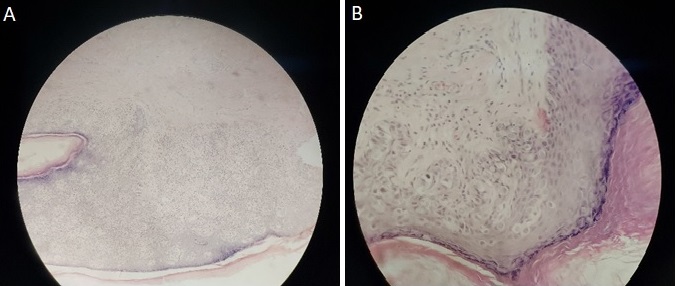
The final diagnosis is Vulvar melanoma Clark Stage IV (Figure 5).
Figure 5. (A and B). Malignant Melanoma, Superficial Spreading Type, Infiltrating up to the Reticular Dermis, with a Maximum Tumor Thickness of 2mm, Pathologic Stage pT2a .
She then received pelvic radiation therapy for 18 fractions. Twenty-eight fractions were advised however radiation was discontinued due to side effects of loose bowel movement and severe abdominal pain. 10 months post-operation, a repeat abdominal CT Scan showed unremarkable findings. She had no evidence of disease for 5 years now (Table 1).
| Date | Imaging Modality | Result |
| 30-Oct-2019 | Plain whole abdominal CT Scan | Negative for presence of suspicious masses nor metastasis |
| 11-Jun-2022 | Plain whole abdominal CT Scan | Negative for presence of suspicious masses nor metastasis |
Discussion
Cancer of the vulva represents 3-5% of malignant neoplasms of the female genital tract with an incidence of 1-2 cases per 100,000 women per year [1]. Squamous cell carcinoma is the most common type of vulvar cancer which represents up to 90% of all vulvar cancers, while vulvar melanoma accounts for only 5-10% [2]. The average age at presentation for vulvar melanoma is approximately 60 years old [3]. The nature of their anatomical location with potentially low self-awareness, social awareness, and public awareness, contributes to the advanced stage at diagnosis and poor overall prognosis, with a 15% 5-year survival [4]. Pruritus is the most reported symptom of vulvar cancers, and less commonly, vulvar bleeding, discharge, or dysuria. Melanomas occur more commonly in the labia majora, followed by the labia minora and clitoris. Index patient initially presented with intense pruritus on the left labia majora with no other associated signs and symptoms such as bleeding, discharges, excoriation, and ulceration. However, three years later, still with intense pruritus, now with irregular patches of discoloration and excoriation, suspicious of a vulvar melanoma.
The pathogenesis of vulvar melanoma remains to be unknown. Unlike cutaneous melanomas, vulvar melanoma is unrelated to chronic sun exposure and damage from ultraviolet light. According to C. Wolmuth, et al., vulvar melanomas harbor a c-KIT mutation which appears to be a characteristic of vulvar melanomas and distinguishes them from vaginal melanomas. However, there is limited data to determine its prognostic significance and the benefit of targeted therapy for vulvar melanomas harboring this type of mutation. A number of risk factors in the occurrence of vulvar melanoma have been identified: (1) Age. Vulvar melanoma is a disease that has an average onset of 68 years old, with risk of onset increasing with age. Index patient at the time of diagnosis was 70 years old. (2) Family history of cutaneous melanoma appears to be a risk factor for vulvar melanoma [5]. (3) UV radiation may be involved indirectly by causing cell-mediated systemic alteration of the immune response which creates a more favorable environment for the development of vulvar melanomas [6].
Imaging is important in the initial evaluation of patients with vulvovaginal melanoma because of its high propensity for metastasis. Pelvic MRI may provide information regarding the extent of local spread and may assist in decisions regarding surgical management [7]. A CT/PET scan may be used to assess regional and distant metastasis [8]. CT scan was done as a more cost-effective approach to assess the presence of local and distant metastasis.
Dermoscopy, which is the use of skin surface microscopy to evaluate skin lesions may be used as a diagnostic tool for vulvar melanomas, however, due to its availability only to dermatologists, an excisional biopsy is required for the diagnosis of all suspicious lesions, particularly for patients over the age of 50 [9]. Tumor thickness, defined by Breslow’s Depth of invasion is the most important determinant of melanomas. Breslow thickness is a measurement of the vertical thickness of the tumor measured histopathologically from the epidermal granular layer to the deepest dermal invasive melanoma cell [2]. There are several histologic subtypes for melanoma namely: superficial spreading, nodular, lentiginous, spindle cell, amelanotic, epitheloid, and mixed spindle and epitheloid. For vulvar melanomas, the most common histologic subtype is superficial spreading, followed by the nodular type [5]. The superficial spreading is described as flat, and irregular in shape and color, with different shades of black and brown, while the nodular type usually starts as a raised area that is blackish-blue or bluish-red. The lesions in this case are described as flat, irregular patches, in shades of black, like that of a superficial spreading type.
The International Federation of Gynecology and Obstetrics (FIGO) staging applied for vulvar carcinomas is not appropriate for vulvar melanomas. Hence, micro-staging for cutaneous melanomas are applied (Table 2) namely: Breslow classification which measures the vertical thickness of the lesion in millimeters; Clark classification which describes the anatomic level of skin invasion, and Chung Classification, which is a modified Clark classification.
| Level | Breslow 1 | Clark 1 | Chung |
| I | Tumor thickness < 0.75mm | In situ melanoma; all tumor is above epidermal basement membrane | In situ melanoma; all tumor is above epidermal basement membrane |
| II | Tumor thickness 0.75-1.50mm | Tumor extends through the basement membrane into papillary dermis | Tumor invasion = 1mm |
| III | Tumor thickness 1.51-2.25mm | Tumor fills the papillary dermis and extends to the reticular dermis but does not invade it | Tumor invasion = 1-2mm |
| IV | Tumor thickness 2.26-3.0mm | Tumor extends into the reticular dermis | Tumor invasion >2mm |
| V | Tumor thickness >3.0mm | Tumor extends into the subcutaneous fat | Tumor extends into the subcutane- ous fat |
The index patient was diagnosed with Vulvar Melanoma Clark Stage IV which includes invasion into the reticular dermis but not into the subcutaneous tissue.
The primary treatment for localized vulvar melanoma is surgical excision. It consists of a wide local excision with a surgical margin of 1cm for lesions <2mm thick and 2cm for 2mm thick. A vulvectomy is done to the case due to the extent of the lesion. Historically, melanoma of the vulva has been treated with radical vulvectomy which is the removal of the labia majora, labia minora, and clitoris [10]. ; However due to its psychosexual sequelae and surgical morbidities associated, a more conservative approach is favored [11]. In the current series, wide local excision was associated with significantly less blood loss and a shorter hospital stay rather than vulvectomy with or without inguinofemoral lymphadenectomy [10]. The 5-year survival rate remains relatively unchanged, despite the shift in surgical practice towards localized excision [12].
Previously, sentinel lymph node biopsy was a standard treatment for vulvar melanomas. Sentinel lymph node biopsy can help obtain regional involvement while avoiding extended lymph node dissection. The objective of the sentinel lymph node procedure is to detect occult lymph node metastases, and a lymphadenectomy should be performed for locoregional control and prevention of distant metastases only when the sentinel lymph nodes contain metastases [13]. However, the role of lymphadenectomy in sentinel-lymph-node-positive cases remains controversial [3]. Node dissection is not done for this patient due to its absence in the CT scan.
Neoadjuvant chemotherapy and radiation have been studied to decrease tumor bulk prior to surgical resection. Adjuvant radiation is used to control local disease for positive margins and lymph nodes. Systemic therapy for an unresectable disease should include molecular testing to direct immunotherapy and targeted therapy, specifically analyses of c-KIT, BRAF and NRAS mutations [14]. Interferon-alpha is the only FDA approved adjuvant treatment. However, Janco, JMT., et al noted no survival difference for those treated with adjuvant chemotherapy or immunotherapy and a reduced survival for those who received radiation. Patient underwent completed 18 fractions of pelvic radiation therapy, however, discontinued due to its side effects. Despite being unable to complete 28 fractions, the patient remained disease-free for five years.
The reported 5-year survival rate of vulvar melanomas ranges from 10 to 63%. The average time for local recurrence is 5.25 years. Older patients have and increased risk of recurrence [14]. Close surveillance is indicated due to the high recurrence rate for vulvar melanoma. Since there is no research or consensus on an appropriate follow-up schedule, the regimen for vulvar squamous cell carcinoma has been adopted for vulvar melanoma. It consists of physical examinations every 3-4 months for the first two years after diagnosis and biannually in the third through fifth years [14]. According to the Clinical Practice Guidelines, for stages I and II, follow-up should be done every 6-12 months for 5 years then yearly thereafter. For stages III and IV, follow-up is done every 3-12 months for 2 years, then every 3-12 months for 3 years then annually thereafter. A chest X-ray, CT scan, or PET/ CT may be done every 4-12 months, while a brain MRI may be requested for high-risk patients. The patient was seen 5 years after the initial diagnosis, with unremarkable physical examination and CT scan results.
In conclusion, Vulvar melanoma is the second most common type of vulvar cancer with an average age of presentation at 60 years old. The lack of body awareness and social awareness contributes to the diagnosis at the advanced stage with a poor prognosis. Its pathogenesis remains to be unknown. Imaging may aid in the assessment of the extent of the disease, as well as surveillance. Surgical excision remains to be the mainstay of treatment for vulvar melanomas. There are limited data on utilizing Radiotherapy, Chemotherapy, and Immunotherapy as treatment.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors. The authors declare no conflict of interest.
References
- Modern treatment of vulvar cancer Merlo S. Radiology and Oncology.2020;54(4). CrossRef
- Surgical Management of Vulvar Melanoma: A Case Series Sánchez-Prieto M, Fargas F, Tresserra F, González-Cao M, Baulies S, Fábregas R. Case Reports in Oncology.2021;14(2). CrossRef
- Management of vulvar and vaginal melanomas: current and future strategies Leitao MM . American Society of Clinical Oncology Educational Book. American Society of Clinical Oncology. Annual Meeting.2014. CrossRef
- Malignant Melanoma of the Vulva and Vagina: A US Population-Based Study of 1863 Patients Wohlmuth C, Wohlmuth-Wieser I, May T, Vicus D, Gien LT , Laframboise S. American Journal of Clinical Dermatology.2020;21(2). CrossRef
- Vulvar and Vaginal Melanomas-The Darker Shades of Gynecological Cancers Dobrică El, Vâjâitu C, Condrat CE , Crețoiu D, Popa I, Gaspar BS , Suciu N, Crețoiu SM , Varlas VN . Biomedicines.2021;9(7). CrossRef
- Population-based incidence rates of malignant melanoma of the vulva in Germany Stang A, Streller B, Eisinger B, Jöckel KH . Gynecologic Oncology.2005;96(1). CrossRef
- MRI Staging in Locally Advanced Vulvar Cancer: From Anatomy to Clinico-Radiological Findings. A Multidisciplinary VulCan Team Point of View Gui B, Persiani S, Miccò M, Pignatelli V, Rodolfino E, Avesani G, Di Paola V, et al . Journal of Personalized Medicine.2021;11(11). CrossRef
- Gynecologic tumor board: a radiologist's guide to vulvar and vaginal malignancies Chow L, Tsui BQ , Bahrami S, Masamed R, Memarzadeh S, Raman SS , Patel MK . Abdominal Radiology (New York).2021;46(12). CrossRef
- Vulvar Malignant Melanoma: A Narrative Review Falcicchio G, Vinci L, Cicinelli E, Loizzi V, Arezzo F, Silvestris E, Resta L, et al . Cancers.2022;14(21). CrossRef
- Vulvar melanoma reconsidered Look KY , Roth LM , Sutton GP . Cancer.1993;72(1). CrossRef
- Vulvar cancer: surgical management and survival trends in a low resource setting Kumar N, Ray MD , Sharma DN , Pandey R, Lata K, Mishra A, Wankhede D, Saikia J. Journal of the Egyptian National Cancer Institute.2020;32(1). CrossRef
- Vulvar and vaginal melanoma: case series and review of current management options including neoadjuvant chemotherapy Janco JMT , Markovic SN , Weaver AL , Cliby WA . Gynecologic Oncology.2013;129(3). CrossRef
- Vulvar melanoma: is there a role for sentinel lymph node biopsy? Hullu JA , Hollema H, Hoekstra HJ , Piers DA , Mourits MJE , Aalders JG , Zee AGJ . Cancer.2002;94(2). CrossRef
- Diagnosis and Management of Vulvar Malignant Melanoma: An Uncommon and Aggressive Mucosal Melanoma Chen C, Schwartz MR , Holder AM . ACS Case Reviews in Surgery.2021;3(4):38-41.
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2024
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times