Clinicopathological Spectrum of Head and Neck Lesions By FNAC at a Tertiary Care Centre in Barpeta, Assam – A Retrospective Study
Download
Abstract
Background: Various neoplastic and non-neoplastic lesions arising from lymph nodes, salivary glands, thyroid gland, soft tissue and metastatic deposits comprises the wide spectrum of lesions in the head & neck region. The Foundation of Head and Neck Cancer (FHNC) helps in differentiating non-neoplastic lesions from neoplastic and further from benign and malignant lesions. The aim of this study was to evaluate the role and diagnostic accuracy of FNAC in diagnosis of palpable head and neck lesions.
Materials and methods: A total of 360 cases were included in the study. Out of the 360 cases, 122 (33.89%) cases were sent for histopathological examination and the results were correlated histologically. Aspirations were done by using 10 ml syringe and 22/23-gauge needles. Smears were stained with May Grunwald Giemsa (MGG). Cytomorphological diagnosis was given.
Results: Out of 360 patients of head and neck lesions studied, lymph node (40.56%) was the predominant site aspirated with reactive lymphoid hyperplasia being the commonest lesion. Soft tissue constitutes 31.11% cases followed by thyroid lesions with 19.72% cases, salivary gland 7.22% cases, and oral cavity 1.39% cases. FNAC was inconclusive in 4.17% cases.
Conclusion: Head and neck lesions are common lesions located superficially that can be easily diagnosed on cytology. Although excisional biopsy is the gold standard for diagnosing head and neck malignant lesions, FNAC plays a vital role as a quick and inexpensive diagnostic procedure with high diagnostic accuracy. It distinguishes between inflammatory/infection and neoplastic lesions, avoiding needless procedures and expediting therapy. FNAC is a low-cost, accurate diagnostic method that may be used as a first-line examination.
Introduction
Fine Needle Aspiration Cytology (FNAC) provides several benefits and applications in the head and neck region. Early identification of benign from malignant disease is advantageous since it considerably impacts treatment planning [1]. Neck lesions can provide a diagnostic difficulty for clinicians. Visible neck lesions can be caused by several inflammatory and neoplastic illness affecting the various neck components. The correct diagnosis of the lesion is critical for successful patient care. Radiology does not always assist and may be ineffective [2]. Fine needle aspiration cytology is a valuable diagnostic technique for evaluating neck lesions. It is a low-risk, cost effective, and minimally intrusive technique that gives critical information for patient management. It has a growing body of data supporting its use in the diagnosis of solid head and neck lesions [3]. FNAC also lessens the need for surgical intervention while also providing valuable information to guide histological diagnosis and serves as the first-line examination for the identification of head and neck lesions [4].
The head and neck region is the most common site overall for FNAC. Wide variety of lesions such as epidermal cysts, cervical lymphadenopathy, lipomas, lymph nodes, thyroid swellings or tubercular lymphadenitis are types of head and neck masses that might be painful or painless, adherent or fluctuant. Apart from the similar location of these lesions, they have unique prognoses and pathological characteristics [5]. This study examines the epidemiology of head and neck masses in the defined population, focusing on the use of fine needle aspiration and cytology in diagnosing the lesions. The aim of this study was to: to study the spectrum of distribution of head and neck lesions, to evaluate the role of FNAC and its utility in diagnosis of palpable head and neck lesions, and to study diagnostic accuracy of FNAC in detecting malignant lesions by histopathological correlation wherever possible.
Materials and Methods
This is a retrospective study conducted with a total of 360 cases which were referred for FNAC with head and neck lesions in the Cytology section of Department of Pathology, Fakhruddin Ali Ahmed Medical College and Hospital. The study was conducted during the period of September 2021 to August 2022 after ethics committee clearance from the parent institution vide letter number FAAMC&H/P.Est./I.E.C./26/Pt.-1/2022/97. Out of the 360 cases, 122 cases were sent for histopathological examination and the results were correlated histologically. Aspirations were done by using 10 ml syringe and 22/23-gauge needles. Smears were stained with May Grunwald Giemsa (MGG). Cytomorphological diagnosis was given.
For histopathological examination, formalin fixed tissue paraffin blocks were stained with Haematoxylin and Eosin stains. The data were divided into five large groups which represent the nature of origin of the neck masses. The groups are: a) Salivary glands, b) Cervical lymph nodes, c) Thyroid gland, d) Lymph node e) Soft tissue and f) Oral cavity. The cytological features were correlated with the histomorphological features and the efficacy of FNAC was evaluated.
Results
In the present study on head and neck lesions among patients, our investigation yielded intriguing findings regarding the distribution and characteristics of various pathologies (Table 1).
| Distribution | ||
| Site or Organ | Number | Percent |
| Lymph Node | 146 | 40.56 |
| Soft Tissue | 112 | 31.11 |
| Thyroid | 71 | 19.72 |
| Salivary Gland | 26 | 7.22 |
| Oral Cavity | 5 | 1.39 |
| Total | 360 | 100.00 |
A striking observation was the prevalence of lymph nodes as the primary site for aspiration, representing 40.56% of the cases studied. Close behind were soft tissue lesions, constituting 31.11%, while thyroid lesions accounted for 19.72%, salivary gland lesions for 7.22%, and oral cavity lesions for 1.39%. A subset of cases, approximately 4.17%, resulted in inconclusive findings through fine-needle aspiration cytology (FNAC).
Age-related patterns emerged as a distinctive feature in our analysis. The 21 to 30 years age group exhibited a higher incidence of lymph node, thyroid, and soft tissue pathologies, indicating a potential susceptibility in this demographic (Table 2).
| Cancer | Age group | Total | ||||||||
| 1-10 | 11-20 | 21-30 | 31-40 | 41-50 | 51-60 | 61-70 | 71-80 | 81-100 | ||
| Lymph Node | 14 | 22 | 31 | 15 | 22 | 20 | 13 | 4 | 5 | 146 |
| Soft Tissue | 12 | 21 | 29 | 18 | 17 | 11 | 3 | 1 | 0 | 112 |
| Thyroid | 1 | 6 | 21 | 10 | 16 | 10 | 7 | 0 | 0 | 71 |
| Salivary Gland | 0 | 4 | 6 | 1 | 3 | 9 | 2 | 1 | 0 | 26 |
| Oral | 0 | 1 | 1 | 1 | 0 | 2 | 0 | 0 | 0 | 5 |
| Total | 27 | 55 | 89 | 45 | 58 | 50 | 25 | 6 | 5 | 360 |
Conversely, salivary gland and oral pathology lesions were more prevalent among individuals aged 51 to 60 years, suggesting a different age-related trend for these particular conditions.
A closer examination of specific aspirated sites revealed cervical lymph nodes as the predominant location, with reactive lymphoid hyperplasia (33.56%) and metastatic squamous cell carcinoma (26.03%) being the most prevalent diagnoses.
Soft tissue lesions presented a diverse spectrum, with epidermal cysts emerging as the most frequent diagnosis (33.04%). In the lesions of thyroid swellings, colloid goitre took precedence, constituting a substantial 66.20% of cases. Salivary gland lesions, on the other hand, featured pleomorphic adenoma as the leading diagnosis, comprising 46.15% of cases (Table 3).
| Site | FNAC Finding | Cases | Percentage |
| Lymph Node | Reactive Lymphoid Hyperplasia | 49 | 33.56 |
| (n=146) | Inflammatory lesions | 52 | 35.62 |
| Acute suppurative lesion | 22 | 15.07 | |
| Granulomatous lymphadenitis | 28 | 19.18 | |
| Inflammatory lesion | 2 | 1.37 | |
| Neoplastic lesions | 41 | 28.08 | |
| Hodgkins Lymphoma | 2 | 1.37 | |
| Metastatic SCC | 38 | 26.03 | |
| Lymphoproliferative Lesion | 1 | 0.68 | |
| Inconclusive | 4 | 2.74 | |
| Soft Tissue | Inflammatory lesions | 11 | 9.82 |
| (n=112) | Acute suppurative lesion | 6 | 5.36 |
| Inflammatory lesion | 5 | 4.46 | |
| Benign lesions | 93 | 83.03 | |
| Benign cystic lesion | 25 | 22.32 | |
| Benign Spindle Cell Lesion | 3 | 2.68 | |
| Epidermal Cyst | 37 | 33.04 | |
| Lipomatous lesion | 19 | 16.96 | |
| Sebaceous cyst | 1 | 0.89 | |
| Vascular Lesion | 8 | 7.14 | |
| Malignant lesions | 2 | 1.78 | |
| Malignant epithelial neoplasm | 1 | 0.89 | |
| Metastatic Carcinoma | 1 | 0.89 | |
| Inconclusive | 6 | 5.36 | |
| Thyroid | Inflammatory lesions | 11 | 15.5 |
| (n=71) | de Quervain Thyroiditis/Granulomatous Thyroiditis | 2 | 2.82 |
| Lymphocytic Thyroiditis/Hashimotos Thyroiditis | 8 | 11.27 | |
| Inflammatory lesion | 1 | 1.41 | |
| Benign lesions | 54 | 76.06 | |
| Benign cystic lesion | 2 | 2.82 | |
| Colloid Goitre Bethesda Cat 2 | 47 | 66.2 | |
| Follicular Neoplasm Bethesda Cat 4 | 5 | 7.04 | |
| Malignant lesions | 6 | 8.46 | |
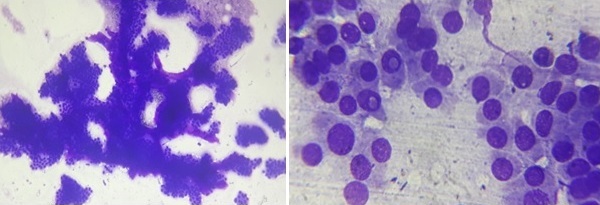
| Papillary Thyroid Carcinoma (Figure 2) | 3 | 4.23 | |
| Anaplastic Carcinoma of Thyroid | 1 | 1.41 | |
| Inconclusive | 2 | 2.82 | |
| Salivary Gland | Inflammatory lesions | 6 | 23 |
| (n=26) | Acute suppurative lesion | 4 | 15 |
| Chronic sialoadenitis | 2 | 8 | |
| Benign lesions | 12 | 46 | |
| Pleomorphic Adenoma | 12 | 46 | |
| Malignant lesions | 7 | 27 | |
| Adenoid Cystic carcinoma | 2 | 8 | |
| Acinic Cell Carcinoma (Figure 1-Left) | 2 | 8 | |
| Salivary duct carcinoma (Figure 1-Right) | 2 | 8 | |
| Mucoepidermoid Carcinoma | 1 | 4 | |
| Inconclusive | 1 | 4 | |
| Oral Cavity | Benign lesions | 2 | 40 |
| (n=05) | Benign cystic lesion | 1 | 20 |
| Vascular Lesion | 1 | 20 | |
| Malignant lesions | 3 | 60 | |
| Squamous cell carcinoma | 1 | 20 | |
| Inconclusive | 2 | 40 |
To further enrich our understanding, histopathological correlation was conducted for 122 cases. The outcomes demonstrated a noteworthy alignment with cytological diagnoses in 97 cases, underscoring the reliability of cytological assessments (Table 4).
| Histopathological correlation | |||
| Site/Organs | Positive correlation | Negative correlation | Percentage Correlation |
| Lymph Node | 6 | 7 | 46.15 |
| Soft Tissue | 33 | 8 | 80.49 |
| Thyroid gland | 40 | 5 | 88.89 |
| Salivary Gland | 16 | 3 | 84.21 |
| Oral cavity | 2 | 2 | 50.00 |
| Total | 97 | 25 | 79.51 |
However, 25 cases exhibited disparities, emphasizing the nuances and challenges in diagnosing certain lesions solely through cytology. Intriguingly, soft tissue, thyroid, oral cavity and salivary gland lesions exhibited a strong correlation with histopathological findings, implying a robust diagnostic consistency in these cases. In contrast, lymph node lesions presented a less consistent correlation, signifying potential complexities in accurately characterizing these lesions through histopathology.
Our diagnostic approach achieved an impressive 95.90% accuracy rate, with robust sensitivity of 82.61%, indicating adept identification of positive cases. Specificity excelled at 98.99%, minimizing false positives. Positive predictive value stood at 95.0%, ensuring reliability of positive diagnoses, while a 96.08% negative predictive value minimized false negatives, collectively affirming the effectiveness of our method.
This detailed study not only contributes to our understanding of the intricate landscape of head and neck pathology but also provides valuable insights for clinicians and pathologists. The documentation of various lesions in corresponding tables serves as a comprehensive reference for future research and diagnostic endeavours. By highlighting age-related patterns and specific aspirated sites, our findings offer a nuanced perspective that can guide clinicians in tailoring their diagnostic approach based on demographic and anatomical considerations.
The correlation analysis further accentuates the need for a multifaceted diagnostic strategy, combining both cytological and histopathological assessments for a comprehensive evaluation of head and neck lesions.
Discussion
Head and neck cancers are the most prevalent malignancy among men in India, ranking second overall. With 119,992 new cases and 72,616 fatalities in 2018, India has the largest number of oral cavity cancer patients in the world [6, 7]. Fine Needle Aspiration Cytology (FNAC) stands as a pivotal tool in the comprehensive assessment of head and neck swellings, offering a minimally invasive approach for cytological insights. The historical roots of FNAC trace back to the early 20th century, with its formal inception by Dr. Martin and Dr. Ellis in the 1930s. Since then, FNAC has evolved, becoming instrumental in diagnosing various lesions [8]. The significance of FNAC in this context is underscored by several key studies that collectively contribute to a broader understanding of the spectrum of lesions encountered and the diagnostic accuracy achieved through this technique [9-11].
A noteworthy study by Sharma PC et al. [12], conducted in 2016, titled “Spectrum study and diagnostic accuracy of fine needle aspiration cytology of head and neck swellings,” provides an extensive exploration into the diverse array of head and neck lesions identified through FNAC. By investigating both the spectrum of cases and the diagnostic precision achieved, the study contributes valuable insights into the efficacy of FNAC as a diagnostic tool in the intricate landscape of head and neck pathology [9].
Complementing this, the research conducted by Vedashree M et al. [10] in 2017, on palpable pathological lesions in the head and neck region, expands our understanding of FNAC’s role in diagnosing these lesions. This study delves into the prevalence and nature of palpable lesions within a tertiary care setting, offering a nuanced perspective on the diagnostic utility of FNAC in characterizing these lesions [10].
Figure 1. Cytopathology Images of Acinic Cell Carcinoma (Left) and Salivary Duct Carcinoma (Right) of Salivary Gland.
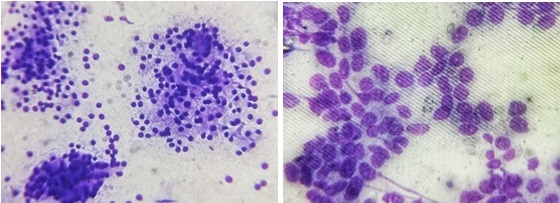
Figure 2. Cytopathology Images of Papillary Carcinoma of Thyroid Showing Characteristic Papillary Architecture (Left) and Nuclear Pseudoinclusions (Right).
Additionally, Solanki P et al. [11], in their 2012 study titled “Fine needle aspiration cytology as a diagnostic procedure in head and neck swellings, contributes further insights into the diagnostic landscape. This study adds depth to the understanding of FNAC’s role in the context of head and neck swellings, enriching our knowledge of its application as a diagnostic procedure [11].
Collectively, these studies form a comprehensive body of work that not only elucidates the intricacies of head and neck lesions but also underscores the importance of FNAC in enhancing diagnostic accuracy in this crucial clinical domain.
In the present study, the primary age group in this study encompasses individuals aged 21 to 30 years, aligning with the demographic focus in studies conducted by Suryawanshi Kishor et al. [12] and Shiladaria PB et al. [4]. Within the scope of the present investigation, involving 360 cases of head and neck lesions, the most prevalent site for aspiration was the lymph node, accounting for 40.56% of cases. Consistent findings were reported by Rajbhandari M et al. [14], Patel Deval N et al. [13], Suryawanshi Kishor et al. [12], Shiladaria PB et al. [4], and Kumawat CP et al. [15]. Among lymph node lesions, the predominant condition in our study was reactive lymphoid hyperplasia, corroborating the observations made by Rajbhandari M et al. [14] and Patel Deval N et al. [13].
Salivary gland lesions constituted 7.22% of total cases, with pleomorphic adenoma being the most frequent diagnosis at 46.15%. Similar conclusions were drawn in a study conducted by Patel Deval N et al. [13].
Thyroid pathology accounted for 19.72% of cases, with all thyroid lesions categorized under the Bethesda system for reporting thyroid cytopathology. Category II, colloid goitre emerged as the predominant finding in this study, consistent with the results reported by Patel Deval N et al. [13], Suryawanshi Kishor et al. [12], and Shiladaria PB et al. [4].
Soft tissue lesions predominantly exhibited a cystic nature, with epidermal cyst being the most frequent diagnosis at 33.04% of cases, followed by benign cystic lesions at 22.32%. Similar outcomes were noted in studies conducted by Suryawanshi Kishor et al. [12] and Shiladaria PB et al. [4], respectively.
In our study, the statistical outcomes demonstrated a commendable accuracy of 95.90%, aligning closely with findings from comparable international studies. Notably, our sensitivity and specificity, at 82.61% and 98.99%, respectively, mirrored results reported by Suryawanshi Kishor., et al. [12], who achieved 93.02% accuracy with 81.81% sensitivity and 96.87% specificity. Similarly, Rajbhandari, M., et al. [14] reported an accuracy of 87.40%, with sensitivity and specificity at 86% and 97%, reinforcing the consistency of our results with established international research. In conclusion, the cytopathological exploration of head and neck lesions, coupled with meticulous histopathological correlation, emerges as an indispensable diagnostic approach. This integrative methodology plays a pivotal role in elucidating the nature of lesions, facilitating precise diagnosis, and guiding therapeutic interventions. Within this diagnostic landscape, Fine Needle Aspiration Cytology (FNAC) stands out as a highly effective and minimally invasive tool. Its efficacy in head and neck lesions lies in its ability to provide nuanced insights, contributing significantly to the overall diagnostic accuracy. The seamless integration of cytological and histopathological data enhances our understanding, enabling clinicians to make informed decisions for optimal patient care.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors.
Conflict of Interest
The authors declare no conflict of interest.
References
- Cytological correlation of spectrum of head and neck lesions with epidemiological and diagnostic parameters Mannan R, Piplani S, Sharma S, Manjari M, Gupta S. Indian J Pathol Oncol.2017;4(1):92-7.
- Fine needle aspiration cytology of neck lesion-an experience at tertiary care hospital in central Gujarat Chauhan S, Darad D, Dholakia A. National journal of medical research.2012;30;2(03):255-9.
- Carotid Body Tumor Diagnosed by On-Site FNA: a Case Report Nagiredla P, Tummidi S, Patro MK . Indian Journal of Surgical Oncology.2019;10(2). CrossRef
- Role of FNAC in evaluation and diagnosis of head and neck lesions: A retrospective study at tertiary care center Shiladaria D, Khant D. International Journal of Clinical and Diagnostic Pathology.2019;2. CrossRef
- Review of Head and Neck Masses in the Indian Population Based on Prevalence and Etiology With an Emphasis on Primary Diagnostic Modalities Bhasker N. Cureus.2021;13(7). CrossRef
- Epidemiology and survival analysis of head and neck cancer: Results from comprehensive care center in North India Badola A, Mehta P, Mehra S, Sood S. Oral Oncology Reports.2023;6. CrossRef
- A Study of Head and Neck Cancer Patients with Reference to Tobacco Use, Gender, and Subsite Distribution Chauhan R, Trivedi V, Rani R, Singh U. South Asian Journal of Cancer.2022;11(1). CrossRef
- Biopsy by needle puncture and aspiration Martin HE , Ellis EB . Annals of Surgery.1930;92(2). CrossRef
- Spectrum study and diagnostic accuracy of fine needle aspiration cytology of head and neck swellings Sharma PC , Hazari RA , Patle YG , Sharma RK . 18.2016;1:5.
- The spectrum of various palpable pathological lesions in head and neck region in a tertiary care hospital – FNAC study Vedashree MK , Girish M, Maruthi CV CV. Indian Journal of Pathology and Oncology.;4(1).
- Fine Needle Aspiration Cytology as A Diagnostic Procedure in Head and Neck Swellings Solanki PK , Patel AP , Taviad PP , Chaudhari VP , Patel SM . National Journal of Community Medicine.2012;3(03).
- Spectrum of FNAC in palpable head and neck lesions in a tertiary care hospital in India-a 3 years study Kishor S, Damle R, Dravid N, Yogesh T. Indian Journal of Pathology and Oncology.2015;2.
- Fine needle aspiration cytology role in head and neck lesions Patel DN , Patel PB , Patel HV , Gandhi TJ . International Archives of Integrated Medicine.2015;2(8).
- The correlation between fine needle aspiration cytology and histopathology of head and neck lesions in Kathmandu University Hospital Rajbhandari M., Dhakal P., Shrestha S., Sharma S., Shrestha S., Pokharel M., Shrestha I., Shrestha B., Makaju R.. Kathmandu University medical journal (KUMJ).2013;11(44). CrossRef
- Cytological Spectrum of Lesions in Neck Swelling with Histopathological Correlation in RUHS Medical College and Hospital Kumawat CP , Gupta YK , Singh A. 2022;14(11):282-7.
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2024
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times