Management of Oligometastatic Gynecological Cancer: Use of Systemic Chemotherapy to Select Patients for Curative Treatment
Download
Abstract
Introduction: Oligometastatic cancer is a growing field in oncology, offering potential curative-intent treatments for highly selected patients with a limited number of metastases beyond the primary tumor. The definition of oligometastatic cancers varies according to tumor type. Careful selection of patients is important. We describe the role of short-course systemic chemotherapy in selecting patients for curative treatment of gynecological malignancies.
Methods: Three cases of gynecological cancers with oligometastatic disease treated with systemic chemotherapy followed by radiotherapy and/or surgery are reported and discussed.
Results/Discussion: All three patients had a complete or very good partial response to 3 cycles of carboplatin and paclitaxel, followed by either surgery or curative radiotherapy. All patients are alive and disease-free when writing this report, with follow-up periods ranging from 10 to 33 months after primary diagnosis.
Conclusion: This case series highlights the feasibility and potential benefits of curative-intent treatments in carefully selected oligometastatic cancer patients with underlying gynecological malignancies. Challenges in defining the optimal treatment approach and sequencing of therapies remain, emphasizing the importance of personalized plans and ongoing research. Integrated care and multidisciplinary team discussions were crucial in tailoring treatment plans.
Introduction
Oligometastatic cancer (OMC) is an intermediate state between locoregional and metastatic cancer and has drawn much attention recently [1]. The theory of OMC was proposed based on the presumption that local treatment, when added to standard systemic treatment may result in long-term disease control, and hence improve the outcomes of these patients [2]. Stereotactic ablative radiotherapy (SABR), when added to cytotoxic chemotherapy, targeted therapy, or immunotherapy is practiced widely, is now considered a treatment strategy, and is supported by guidelines [3]. However, consensus about the definition, the biomarker for identification, and the diagnosis of OMC in various cancers is lacking [4].
The largest series with the longest follow-up data comes from the SABR-COMET study [5]. Patients with cancers of the breast, lung, colorectum, prostate, and a few other sites, who had between 1 and 5 metastatic lesions, and whose primary malignancy was under control were randomly assigned standard of care with or without SABR. The 5-year overall survival improved from 17.7% to 42.3%. However, there was a mix of patients, and the overall sample size consisted of only 99 patients. There are a few other reports on the outcomes of treatment of OMC (reviewed in Palma 2020). Most of these studies were reported on patients with either prostate or non-small cell lung cancer. Recently, Mohamed et al. [6] reported the outcomes of patients with oligometastatic or recurrent cancer of the head and neck and identified p16-positive squamous cell cancer, metachronous OMC, and a longer time to progression as positive predictors of OS. Hu et al. [7] reported that patients with single-organ metastases from pancreatic cancer had a longer OS (11 vs 7 months) if chemotherapy was added to the local therapy. Furthermore, patients with lung metastasis did better than patients with liver metastasis.
There are only a few studies about the definition and treatment outcomes of OMC in gynecological malignancies. Recently, a meta-analysis showed the addition of SBRT in OMC with underlying gynecological malignancies was associated with favorable response and local control rates [8] however, there was a high rate of progression outside the field of radiation. Despite the growing body of research on OMC, there remains a scarcity of studies investigating its definition and treatment outcomes specifically in gynecological malignancies. By sharing our experience, we aim to highlight the importance of careful selection of patients using response to chemotherapy as a marker for sustained disease control in patients with gynecological malignancies, who have OMC.
Materials and Methods
Case 1
A 66-year-old lady presented with a 3-month history of post-menopausal vaginal bleeding associated with foul-smelling vaginal discharge, abdominal swelling, and occasional dysuria. She was known to have hypertension. There was no known family history of cancer. On examination, the patient had an excellent performance status (ECOG 0). Gynecological examination revealed a normal vulva and a large circumferential mass in the cervix measuring 7 x 6 cm, hard in consistency with bleeding. There was obliteration of the left vaginal fornix and the left parametria was involved. Biopsy showed a moderately differentiated squamous cell carcinoma of the cervix, p16 positive. MRI of the pelvis showed a large cervical mass measuring 5x5x7 cm, invading the lower 2/3rd of the uterine body and upper 1/3rd of the vagina, and a 6.5 x 4 x 7 cm metastatic left external iliac lymph node, with thin septation, a solid component with a large cystic area, and a 3 x 3 cm lymph node at the level of left internal iliac artery bifurcation. PET-CT showed an FDG-avid lesion in the uterine cervix, bilateral obturator FDG-avid lesions, and an intensely FDG-avid lesion in the left side of the abdomen, inseparable from the anterior abdominal wall and bowel loops, suggestive of an omental deposit (Figure 1 (a,b)).
Figure 1. (a). PET-CT Axial Image of the Omental Deposit. (b) CT axial image of the omental deposit. (c): PET-CT axial image showing a partial response of the omental deposit. (d): CT axial image showing a partial response of the omental deposit..
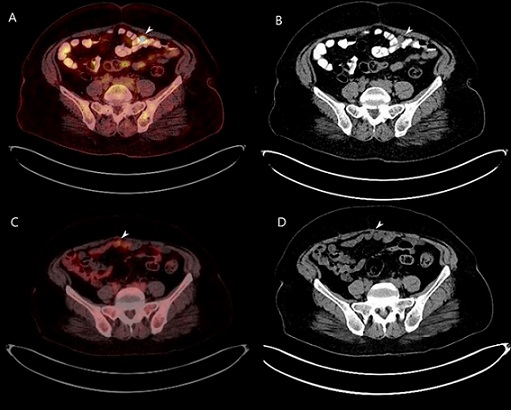
Given the low volume metastatic disease (one lesion in the omentum only) and excellent performance status, the multidisciplinary tumor board recommended 3 cycles of chemotherapy followed by a re-evaluation and in case of response, consideration of curative concurrent chemo-radiotherapy followed by excision of the metastases. The disease responded to 3 cycles of paclitaxel, carboplatin, and bevacizumab with minimal toxicity (grade II diarrhea, grade II nausea, and grade I oral mucositis). Re-staging PET-CT showed a partial response in omental disease with a significant reduction in metabolic volume and FDG intensity of the cervical mass and the lymph nodes (Figure 1(c,d)).
The patient was treated with concurrent chemo- radiotherapy (CCRT) in a curative setting, followed by laparoscopic omentectomy. Pathology from the omentum showed a complete pathological response. The patient remains well, free of disease, 2 years after diagnosis.
Case 2
A 53-year-old lady presented with a 1-month history of post-menopausal bleeding. She underwent laparoscopic total abdominal hysterectomy with bilateral salpingoophorectomy, omentectomy, and pelvic lymphadenectomy at another hospital. She had post- operative complications and underwent exploratory laparotomy with adhesiolysis and small bowel resection. A week later, she developed an enterocutaneous fistula and was explored again for intestinal obstruction. She had repeated infections treated with antibiotics, and 15 days later she developed a pulmonary embolism for which she started on anticoagulants. Two months after these events, she noticed vaginal spotting and on examination was found to have a mass occupying the vagina.
The patient came to our institution for a second opinion and further management. On examination, she had excellent performance status (ECOG 1), and her abdomen had a hypogastric midline scar, with enterocutaneous fistulae. On gynecologic examination, there was a bulky mass protruding from the posterior wall of the vagina with contiguous invasion of the right labia. Due to the mass which bled easily on touch, speculum examination was not possible. On palpation, there was a fixed mass occupying the posterior vagina wall that measured approximately 10cm. The anterior vagina also has a mass effect lesion that was fixed. The lateral walls of the vagina seemed nodular and infiltrated by disease. On rectal examination, the mucosa appeared to be intact.
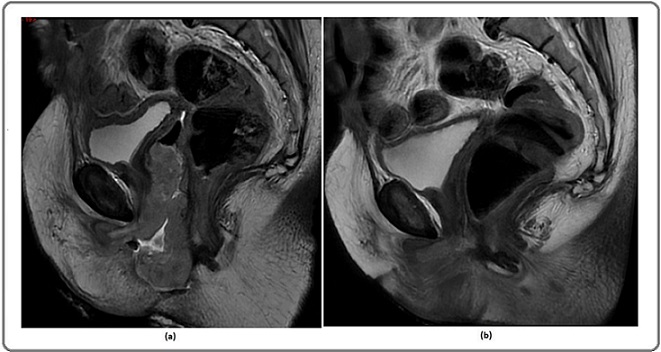
The vaginal lesion was biopsied, and pathology showed HPV-associated moderately differentiated squamous cell carcinoma. MRI of the pelvis showed a large soft tissue heterogeneous enhancing mass occupying the vaginal canal, measuring 4.5 x 5.9 x 10 cm. The mass extended anteriorly below the pubic symphysis involving the perineum, however, no cortical erosion of the pubic bones was noted. It involved the urethra and the rectum with the possibility of rectovaginal fistula posteriorly as well (Figure 2 (a)).
Figure 2. (a) MRI T2-weighted Sagittal Image of the Large Vaginal Mass. (b) Post-chemotherapy MRI T2-weighted sagittal image showing partial response..
Air fluid levels were noted within the vaginal stump superiorly. Multiple enlarged pathological appearing bilateral pelvic sidewall and inguinal recess lymph nodes were noted and a node in the left para-aortic region.
Her case was discussed in MDT, and she was commenced on chemotherapy, paclitaxel, and cisplatin (3 cycles). The follow-up scan showed a near-complete response (Figure 2 (b)).
The patient was treated with CCRT (EBRT with VMAT (volumetric modulated arc therapy) 45Gy in 25 fractions to the pelvis (including inguinal and paraaortic LN) with a simultaneous concomitant boost to the involved LN to a dose of 55Gy. As a boost, she received 21Gy/3 fractions of MRI-guided adaptive brachytherapy).
The patient remains in continuous complete remission for 2 years.
Case 3
A 48-year-old lady presented with a left-sided vulvar mass with clinically palpable left-sided inguinal lymph nodes. Staging investigations revealed a large exophytic cauliflower-shaped lesion involving bilateral labia majora extending into mons pubis and introitus, a few enlarged left inguinal lymph nodes, the largest measuring 27 x 21 mm. She underwent vulvectomy and bilateral inguinal node dissection in another institution. The pathology report described a moderately differentiated keratinizing squamous cell carcinoma – HPV associated - Stage IIIa, PDL-1 negative. She was referred to our institution for adjuvant chemoradiation. A re-staging PET-CT showed a metastatic lung nodule with a high SUV uptake (Figure 3(a,b)), in addition to uptake near the introitus and the left inguinal region.
Figure 3. (a) PET-CT Axial Image of the Solitary Lung Metastasis. (b) CT axial image of the solitary lung metastasis.(c) PET-CT axial image showing a complete metabolic response of the solitary lung metastasis. (d) CT axial image showing a complete metabolic response of the solitary lung metastasis..
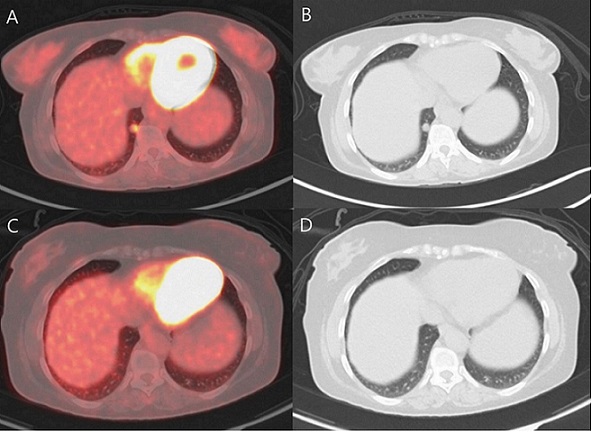
A biopsy from the left inguinal node was positive for SCC. After discussion in MDT, three cycles of chemotherapy (paclitaxel and carboplatin) were administered. A repeat PET-CT scan showed a very good partial response in the inguinal region and a complete metabolic response in the metastatic site in the lung (Figure 3(c,d)). She was then treated with CCRT (external beam radiotherapy 50.4Gy/28 fractions with 10Gy/5 fractions boost to active areas with concurrent cisplatin). The patient is currently on regular follow- up and is free of disease 10 months after diagnosis of metastatic disease.
Results and Discussion
We describe three patients with primary gynecological cancers with oligo-metastatic disease that were treated with curative intent modalities after discussions in the multidisciplinary team meetings. The first case is a patient with oligometastatic cervix cancer whose staging tests showed an omental deposit treated with chemotherapy, followed by radiotherapy and radical surgery. The second case is a patient with primary cancer of the vagina that was found to have a metastatic para-aortic lymph node after undergoing incomplete TAH and a BSO, that was treated with chemotherapy followed by concurrent chemo-radiotherapy with curative doses. The third case is a patient with primary cancer of the vulva with a metastatic lung nodule and was treated with chemotherapy followed by curative chemo-radiotherapy. All the patients responded to the combination chemotherapy and underwent radical procedures with curative intent to control the local disease. The patient with the cervical oligometastatic disease is currently at 33 months follow-up, the vaginal oligometastatic cancer patient is at 27 months follow-up, and the vulvar patient with oligometastatic disease is at 10 months follow-up. These outcomes suggest promising preliminary results for curative-intent treatment modalities in patients with oligo-metastatic gynecological cancers.
Different definitions of OMC have been suggested for various cancers, based mainly on expert opinions. Hendriks et al. [9] surveyed 33 experts involved in the management of non-small cell lung cancer (NSCLC) and reported concordance about the management plan in patients with single metastasis and node-negative disease. Dingemans et al. [10] suggested synchronous oligometastatic NSCLC as an entity if there were fewer than five metastases in three organs, seen on PET scan and after MRI and even thoracoscopic biopsy. 18F-FDG staging was the minimum requirement. It was proposed that this definition will help to standardize inclusion criteria for future clinical trials. Bamias et al. [11] used a modified Delphi method and suggested a maximum of three metastatic sites, all resectable, or amenable to stereotactic therapy, as the definition of OMC of the urinary bladder. Kroese et al. [12] used two Delphi surveys to suggest the definition of OMC in esophagogastric cancer if there were ≤3 metastases or 1 extra-regional lymph node station, or no progression at restaging after systemic therapy.
Oligometastatic gynecological cancer together with most cancer sites is a growing subfield of oncology. It is considered a unique circumstance with potential curative- intent treatments in highly selected patients, one that requires a careful therapeutic strategy with integrated care. A consensus for indication of curative intent radiotherapy was published by the ESTRO-ASTRO document [13] and defined OMC as 1 to 5 metastasis lesions, with optional controlled primary tumor, and all metastatic sites safely treatable. Our patients’ oligometastatic status was defined accordingly and was individually discussed site-specific tumor board. This empowered attending physicians and patients to proceed with curative intent treatments in an oligometastatic setting.
Previously considered incurable, the traditional view of metastatic cancers is giving way to the emergence of oligo-metastatic cancer (OMC), where new systemic therapies combined with local interventions offer hope for longer survival in patients with low-volume metastatic disease. Treatment options like SBRT, minimally invasive surgeries, systemic treatments, and thermal ablations are all available and often employed, alone or in combination, with the intent of eradicating visible disease [14]. However, optimal treatment decisions hinge on a multifaceted discussion based on a comprehensive analysis of patient-tumor-specific characteristics: disease kinetics, age, performance status, psychosocial support, financial considerations, tolerability of side effects, and desired quality of life. A tailored treatment plan crafted with meticulous attention to these factors maximizes clinical benefit in each case.
A study by the EMBRACE research network shed light on the current management of synchronous or metachronous metastatic cervical cancer. The survey focused on evaluating clinical practices across participating sites when managing oligometastatic or oligo-recurrent disease. The results revealed that despite limited high-level evidence for OMC treatment, most oncologists consider using curative intent CCRT for oligometastatic cervical cancer. This finding underscores the reality that oncologists face daily, navigating complex treatment decisions within an evolving therapeutic landscape. It also highlights the crucial role of ongoing research and personalized approaches in maximizing outcomes for each OMC patient [15].
Ning et al. [16] demonstrated promising outcomes with definitive radiotherapy for oligometastatic cervical cancer, with median overall survival exceeding 50 months and a 2-year survival rate above 70%. Their study included patients with two or fewer extra-pelvic/paraaortic metastases, diagnosed at initial diagnosis or follow-up. Standard radiotherapy doses for cervical cancer were used for the primary site, while metastases were targeted with either stereotactic ablative radiotherapy (SBRT) or surgery. Notably, minimal toxicity was observed despite the higher ablative doses.
Despite the established role of surgery in predicting survival for metastatic ovarian cancer patients, the value of resecting metastatic sites as part of the curative treatment for other gynecological cancers such as cervical and uterine malignancies remains an area of active investigation [17]. The existing literature supporting aggressive surgical resection for metastatic gynecological cancer largely consists of retrospective studies and case reports, lacking the robust methodologies of randomized controlled trials. The complexity of such procedures can be substantial, potentially involving non-gynecological organ resection (such as liver and lung) and adding significant surgical risk [18]. The decision to surgically manage metastatic cancer requires careful consideration of potential benefits versus risks, particularly in the absence of definitive evidence demonstrating improved survival or local control.
Mesko et al. [19] found that SABR for oligometastatic gynecological cancer patients was safe and effective, and resulted in 32% partial response, and 17% complete response. While rigorous evidence for specific sequencing is lacking, individualizing treatment approaches within a multimodality framework seems feasible and suggests promising outcomes, considering cost-effectiveness, compliance, and managing toxicity [20].
In conclusion, our case series showcases several oligometastatic gynecological cancer patients treated with multimodal therapies (chemotherapy, radiotherapy, and surgery) following MDT discussions. The sequencing of local and systemic therapies remains an open question, yet it offers exciting possibilities for selecting patients for curative interventions. Although challenges persist in defining the ideal OMC treatment approach, our review highlights the crucial role of systemic chemotherapy in identifying patients and the multidisciplinary collaboration in managing these complex patients.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors.
The authors declare no conflict of interest.
References
- Characterisation and classification of oligometastatic disease: a European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus recommendation Guckenberger M, Lievens Y, Bouma AB , Collette L, Dekker A, deSouza NM , Dingemans AC , et al . The Lancet. Oncology.2020;21(1). CrossRef
- Oligometastases revisited Weichselbaum RR , Hellman S. Nature Reviews. Clinical Oncology.2011;8(6). CrossRef
- Metastases-directed stereotactic body radiotherapy in combination with targeted therapy or immunotherapy: systematic review and consensus recommendations by the EORTC-ESTRO OligoCare consortium Kroeze S.G.C., Pavic M, Jereczek-Fossa A, Westhoff P, Kroeze S, Pavic M, Stellamans K, et al . 2023.
- The biology and treatment of oligometastatic cancer Reyes DK , Pienta KJ . Oncotarget.2015;6(11). CrossRef
- Stereotactic Ablative Radiotherapy for the Comprehensive Treatment of Oligometastatic Cancers: Long-Term Results of the SABR-COMET Phase II Randomized Trial Palma DA , Olson R, Harrow S, Gaede S, Louie AV , Haasbeek C, Mulroy L, et al . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2020;38(25). CrossRef
- Stereotactic radiotherapy in the management of oligometastatic and recurrent head and neck cancer: a single-center experience Mohamed AA , Goncalves M, Singh BP , Tometten M, Rashad A, Hölzle F, Hackenberg S, Eble M. Strahlentherapie Und Onkologie: Organ Der Deutschen Rontgengesellschaft ... [et Al].2024;200(5). CrossRef
- Survival benefit of local consolidative therapy for patients with single-organ metastatic pancreatic cancer: a propensity score-matched cross-sectional study based on 17 registries Hu X, Hu D, Fu B, Li H, Ren G, Liu H, Song J, et al . Frontiers in Endocrinology.2023;14. CrossRef
- Stereotactic body radiation therapy for oligometastatic gynecologic malignancies: A systematic review Yegya-Raman N, Cao CD , Hathout L, Girda E, Richard SD , Rosenblum NG , Taunk NK , Jabbour SK . Gynecologic Oncology.2020;159(2). CrossRef
- Defining oligometastatic non-small cell lung cancer: A simulated multidisciplinary expert opinion Hendriks LEL , Dooms C, Berghmans T, Novello S, Levy A, De Ruysscher D, Hasan B, et al . European Journal of Cancer (Oxford, England: 1990).2019;123. CrossRef
- Definition of Synchronous Oligometastatic Non-Small Cell Lung Cancer-A Consensus Report Dingemans AC , Hendriks LEL , Berghmans T, Levy A, Hasan B, Faivre-Finn C, Giaj-Levra M, et al . Journal of Thoracic Oncology: Official Publication of the International Association for the Study of Lung Cancer.2019;14(12). CrossRef
- Definition and Diagnosis of Oligometastatic Bladder Cancer: A Delphi Consensus Study Endorsed by the European Association of Urology, European Society for Radiotherapy and Oncology, and European Society of Medical Oncology Genitourinary Faculty Bamias A, Stenzl A, Brown SL , Albiges L, Babjuk M, Birtle A, Briganti A, et al . European Urology.2023;84(4). CrossRef
- Definition, diagnosis and treatment of oligometastatic oesophagogastric cancer: A Delphi consensus study in Europe Kroese TE , Laarhoven HWM , Schoppman SF , Deseyne PRAJ , Cutsem E, Haustermans K, Nafteux P, et al . European Journal of Cancer (Oxford, England: 1990).2023;185. CrossRef
- Defining oligometastatic disease from a radiation oncology perspective: An ESTRO-ASTRO consensus document Lievens Y, Guckenberger M, Gomez D, Hoyer M, Iyengar P, Kindts I, Méndez Romero A, et al . Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2020;148. CrossRef
- ESTRO/ESGO/SIOPe guidelines for the management of patients with vaginal cancer Nout R, Calaminus G, Planchamp F, Chargari C, Lax SF , Martelli H, McCluggage WG , et al . Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2023;186. CrossRef
- Management of oligo-metastatic and oligo-recurrent cervical cancer: A pattern of care survey within the EMBRACE research network Chopra S, Mangaj A, Sharma A, Tan LT , Sturdza A, Jürgenliemk-Schulz I, Han K, et al . Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2021;155. CrossRef
- Outcomes and patterns of relapse after definitive radiation therapy for oligometastatic cervical cancer Ning MS , Ahobila V, Jhingran A, Stecklein SR , Frumovitz M, Schmeler KM , Eifel PJ , Klopp AH . Gynecologic Oncology.2018;148(1). CrossRef
- Patients with stage IV epithelial ovarian cancer: understanding the determinants of survival Dabi Y, Huchon C, Ouldamer L, Bendifallah S, Collinet P, Bricou A, Daraï E, et al . Journal of Translational Medicine.2020;18(1). CrossRef
- Role of surgical resection for lung, liver, and central nervous system metastases in patients with gynecological cancer: a literature review Tangjitgamol S., Levenback C. F., Beller U., Kavanagh J. J.. International Journal of Gynecological Cancer: Official Journal of the International Gynecological Cancer Society.2004;14(3). CrossRef
- Clinical Outcomes for Stereotactic Ablative Radiotherapy in Oligometastatic and Oligoprogressive Gynecological Malignancies Mesko S, Sandler K, Cohen J, Konecny G, Steinberg M, Kamrava M. International Journal of Gynecological Cancer: Official Journal of the International Gynecological Cancer Society.2017;27(2). CrossRef
- Oligometastatic Cancer: Key Concepts and Research Opportunities for 2021 and Beyond Szturz P, Vermorken JB . Cancers.2021;13(11). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times