Stenotrophomonas Maltophilia Infection in Cancer Patients Undergoing Major Surgery in A Tertiary Cancer Centre
Download
Abstract
Background: We aim to study the impact of postoperative Stenotrophomonas maltophilia infections among cancer patients undergoing major surgery.
Methods: Ambispective, observational study. Study period from 1st November 2019 to 31st March 2024. The study population included patients with a definite diagnosis of cancer who underwent a major surgical procedure in a single, dedicated surgical unit and developed postoperative infection which showed a documented growth of Stenotrophomonas maltophilia. Clinical and laboratory parameters were collected and data represented as median values, percentages and range.
Results: Nine patients were identified to have Stenotrophomonas maltophilia infection in the postoperative period among a total of 2506 patients. Co-morbid illnesses were noted in 33.3% patients; all were nosocomial infections. Fever was a manifestation in 77.8% patients, 44.4% had leukocytosis. Of all samples, 33.3% were respiratory ones. Co-infection was noted in 44.4% patients. Sensitivity to trimethoprim-sulphamethoxazole was seen in 44.4% and to levofloxacin in 66.7% isolates. Mortality rate was 11.1%.
Conclusion: Stenotrophomonas maltophilia causes uncommon but clinically significant infections among cancer patients in the postoperative period.
Introduction
Stenotrophomonas maltophilia is a multi-drug resistant gram-negative bacillus and it acts as an opportunistic pathogen. Such infections are usually encountered in hospitalized patients and often result in high incidence of morbidity and mortality. The bacillus has inherent resistance to several antibiotics like carbapenems and the indiscriminate use of antibiotics may potentially make it a prominent nosocomial infection. The predisposing factors for S. maltophilia infection include in-dwelling central venous catheters, urinary catheters, mechanical ventilation, a post-surgical period, cancer, an intensive care unit (ICU) setting, use of immunosuppressive drugs and neutropenia. It can cause a wide array of manifestations ranging from pneumonia, bacteremia and sepsis, urinary tract infections, peritonitis, wound infections, cholangitis, arthritis, meningitis and endocarditis. The existing literature about this uncommon pathogen and its implication in patients undergoing major cancer surgery is limited world-wide and non-existent from our region. Our results will be a useful guide with respect to the clinical significance of this pathogen in the context described.
The aim of the study was to describe the impact of Stenotrophomonas maltophilia infection in the postoperative period of patients undergoing major cancer surgery. The primary objective was to estimate the clinical outcomes in terms of in-hospital morbidity and mortality associated with Stenotrophomonas maltophilia infection and the secondary objective was to report about the antibiotic sensitivity profile of these infections besides describing the clinical profile of the patients who had those infections.
Materials and Methods
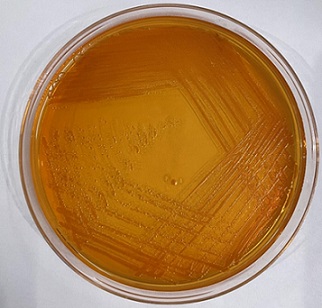
An ambispective, observational study was done in the surgical oncology unit of a tertiary care cancer centre in North-East India during the study period from 1st November 2019 to 31st March 2024. The study population included patients with a definite diagnosis of cancer who underwent a major surgical procedure in a single, dedicated surgical unit and developed postoperative infection which showed a documented growth of Stenotrophomonas maltophilia. All the microbiological samples were processed by standard procedures including inoculation in blood agar and MacConkey agar plates incubated overnight at 37 degrees centigrade and all the plates were examined for visible growth (Figure 1 and 2).
Figure 1. Stetenotrophomonas in Blood Agar.
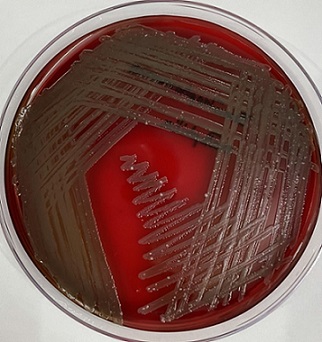
Figure 2. Stenotrophomonas in MacConkey.
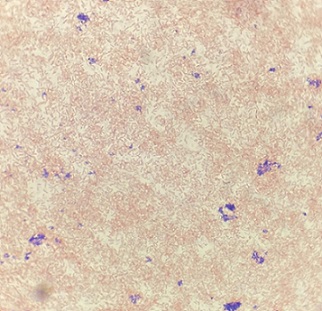
The colonies were identified as per standard microbiological procedures (Figure 3).
Figure 3. Stenotrophomonas under 100x Magnification Showing Gram Negative Bacilli Pattern .
The samples of blood culture were processed in BACT/ALERT 3D (bioMérieux). The final identification of the organisms was identified using a fully automated system, VITEK 2 (bioMérieux).The antibiotic sensitivity profile was done using the same system. For data collection, microbiological and clinical data variables obtained from review of EMR and physical case records. Variables to be studied include: age, sex, co-morbidity, primary malignancy, surgery performed, presence of fever, number of days of ICU and hospital stay, outcomes including whether recovered or succumbed, specimen types, presence of co-infection, blood parameters including total leucocytic count (TLC) and differential leucocytic count (DLC) and antibiotic sensitivity profile. The results were presented with the use of median values, percentages and range. The study was approved by the Institutional Ethical Committee (IEC).
Results
Atotal of 9 patients were found to have Stenotrophomonas maltophilia infection in the postoperative period among the 2506 patients undergoing major oncologic surgeries in the surgical unit concerned. The median age of the patients was 54 years (range 23 to 77 years). There were five male patients and four females. Three patients had co-morbid illnesses (33.3%), other than cancer. Seven patients (77.8%) were those who had major surgery for gastrointestinal and pancreatic cancers. All nine patients had the infection while they were hospitalized. Fever was a manifestation in 77.8% patients (Table 1).
| Characteristic category | Characteristics | No of patients/ Value |
| Median age | 54 years (range 23 to 77 years) | |
| Sex | Male | 5 |
| Female | 4 | |
| Co-morbidity | Diabetes mellitus | 1 |
| Hypertension | 1 | |
| Idiopathic thrombocytopenic purpura | 1 | |
| Others | 0 | |
| Primary malignancy | Esophageal cancer | 3 |
| Pancreatic cancer | 2 | |
| Colon cancer | 1 | |
| Rectal cancer | 1 | |
| Breast cancer | 2 | |
| Surgery performed | Esophagectomy | 3 |
| Whipple’s surgery | 1 | |
| Extended right hemicolectomy | 1 | |
| Low anterior resection | 1 | |
| Modified radical mastectomy | 2 | |
| Distal pancreaticosplenectomy and en bloc left nephrectomy and duodenojejunal flexure resection | 1 | |
| Hospitalized patient | Yes | 9 |
| No | 0 | |
| Fever | Yes | 7 |
| No | 2 | |
| Median ICU stay | 4 days (range 0 to 31 days) | |
| Median hospital stay | 15 days (range 0 to 42 days) | |
| Outcome | Recovered | 8 |
| Succumbed | 1 | |
| Risk factors | In-dwelling central venous catheter | 5 |
| Urinary catheter | 8 | |
| Mechanical ventilation | 5 | |
| ICU stay > 1 day | 5 |
We noted that 44.4% patients had leukocytosis and one patient (11.1%) had leucopenia. The specimens that yielded Stenotrophomonas maltophilia included wound swabs, blood samples, abdominal fluid (from drainage tube), pleural fluid (from pleural effusion) and tracheal swab and secretions. We found that 33.3% of positive samples were pertaining to the respiratory system (Table 2).
| Test | Test categories | Value/ number of patients/ Percentage |
| Total leucocytic count (TLC) | Median total count | 10,630 cells/mm 3 (range 1,850 to 33,710 cells/ mm 3 ) |
| Leukocytosis | 4 | |
| Leukopenia | 1 | |
| Differential leucocytic count (DLC) | Neutrophilia | 8 |
| Eosinophilia | 1 | |
| Specimen type | ||
| Wound swab | Wound swab | 2 |
| Blood | Blood | 2 |
| Abdominal fluid | Abdominal (drain) fluid | 2 |
| Pleural fluid | Pleural fluid | 1 |
| Tracheal swab/ secretion | Tracheal swab/ secretion | 2 |
| Antibiotic sensitivity | ||
| Levofloxacin | 66.70% | |
| Trimethoprim-sulphamethoxazole | 44.40% |
It was found that the bacillus was sensitive to the antibiotic levofloxacin in 66.7% samples and it was sensitive to the antibiotic trimethoprim and sulphamethoxazole in 44.4% samples. Co-infection was noted in 44.4% of patients and these included Pseudomonas aeruginosa, Acinetobacter baumannii, Klebsiella pneumoniae and Enterococcus faecalis VRE (Vancomycin Resistant Enterococcus) (Table 3).
| Surgery | Surgical complication | Specimen that yielded S. maltophilia | Co-infection | Sample yielding co-infection |
| Minimally invasive McKeown’s esophagectomy | Pneumonia | Tracheal swab | Pseudomonas aeruginosa | Pus from neck wound |
| Minimally invasive McKeown’s esophagectomy | Pleural effusion | Pleural fluid | Enterococcus faecalis VRE, Pseudomonas aeruginosa | Abdominal drain fluid |
| Whipple’s pancreaticoduodenectomy | Pancreatojejunostomy anastomosis leak | Blood | None | None |
| Distal pancreaticosplenectomy with en bloc resection of duodenojejunal flexure and left nephrectomy | Peripancreatic collection | Abdominal fluid | None | None |
| Extended right hemicolectomy | Surgical site infection (SSI) | Blood | None | None |
| Low anterior resection | Anastomotic leak | Abdominal fluid | Acinetobacter baumannii, Klebsiella oneumoniae | Pus from abdominal drain fluid |
| Modified radical mastectomy + thoraco-abdominal flap | Surgical site infection (SSI) | Wound swab | None | None |
| Modified radical mastectomy | Surgical site infection (SSI) | Wound swab | None | None |
| Minimally invasive McKeown’s esophagectomy | Anastomotic leak in the neck | Tracheal secretion | Acinetobacter baumannii | Chest drain fluid |
Out of the nine patients in the study, 88.9% of them recovered with appropriate antibiotics. The patients had a median period of intensive care unit (ICU) stay of 4 days (range 0 to 31 days) and a median period of hospital stay of 15 days (range 0 to 42 days). Every patient did have surgical morbidity and one patient succumbed to sepsis (11.1% mortality).
Discussion
Stenotrophomonas maltophilia is recognized as an emerging gram-negative multi-drug resistant organism (MDRO) and an opportunistic pathogen. It is mostly described in a hospital-acquired scenario, when the patient is immunocompromised. Even though it mostly causes respiratory infections, it has the ability to present with a wide spectrum of manifestations including pneumonia and acute exacerbations of chronic obstructive pulmonary disease (COPD), bacteremia and sepsis, urinary tract infections, peritonitis, wound infections, cholangitis, cellulitis and myositis, osteomyelitis and arthritis, eye infections, meningitis and endocarditis. The predisposing factors for S. maltophilia infection include in-dwelling central venous catheters, urinary catheters, mechanical ventilation, a post-surgical period, cancer, an intensive care unit (ICU) setting, use of immunosuppressive drugs and neutropenia [1-6]. We studied a population of patients who underwent major surgery for cancer and had several of such risk factors. Cancer itself has been described as a predisposing condition and the implications of infection by this organism has been described recently in the available literature. Cancer patients may be immunocompromised due to the debilitating disease per se or the use of chemotherapeutic agents. A major surgery also has its effect on the immune system, especially during the well-recognized phase of perioperative catabolism [7]. In our study, the median duration of ICU stay was 4 (range 0 to 31 days). Five patients had in-dwelling central venous catheters and a same number had mechanical ventilator support (55.6%).
Stenotrophomonas maltophilia was first isolated in 1943 as Bacterium bookeri and was subsequently named Pseudomonas maltophilia, then Xanthomonas maltophilia and eventually, the present nomenclature [8, 9]. The organism is often isolated from aqueous-associated sources like water-treatment and distribution sources, sinkholes, tap water, contaminated chlorhexidine-cetrimide antiseptic solutions, irrigating solutions, hand-washing soaps etc. It has a special ability to adhere to plastic and produce biofilms, such as in intravenous cannulae and catheters, nebulizers and prosthesis [5] [10-14].
Stenotrophomonas maltophilia has intrinsic resistance to carbapenems and prior history of use of these agents is implicated in selection pressure for this pathogen [15-20]. Trimethoprim-sulfamethoxazole has been often viewed as the antimicrobial agent of choice, but resistance has increasingly been reported [21-24]. In our study, only 44.4% of the isolates were sensitive to this antibiotic. The susceptibility to alternative antimicrobial agents is often explored [25-28]. Sensitivity to levofloxacin was seen in 66.7% of isolates in our study. In certain situations, combination therapy or alternative routes of drug administration such as in aerosol form for pulmonary infections may be considered [29].
The crude mortality rate for patients with infection with this pathogen has been reported within the range of 14 to 69%. In our series, one patient succumbed to the infection (11.1%). A systematic review has highlighted that a significantly higher mortality occurs in patients treated with an initially inappropriate antibiotic, 61% as opposed to 30%. And, up to 37.5% of mortality was found to be attributable to Stenotrophomonas maltophilia infections. [30] From our series, we can note that outcomes of S. maltophilia infections have been varied, with two patients who had skin wound infections having a clinically non-significant course even with multi-drug resistance to the pathogen, whereas those with abdominal and thoracic cavity infections or bloodstream infections, especially in the presence of an adverse risk factor or an underlying serious surgical complication, having a significant clinical course. This re-iterates the fact that clinicians should not underestimate the clinical significance of these infections. In conclusion, Stenotrophomonas maltophilia infections, even though unusual, causes serious clinical manifestations with high morbidity and mortality rates and requires pinpoint antimicrobial therapy in view of several resistance patterns. These are opportunistic hospital-acquired infections which occur in patients with one or more adverse risk factors. Such risk factors become very prominent for patients being treated for cancer. The judicious use of currently available antimicrobial agents known as Antimicrobial Stewardship with pro-active hospital infection control policies will go a long way in curbing this menace.
Acknowledgments
Funding
None
Competing interests
None
Author contributions
Author contributions: Both authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Amrita Talukdar and Gaurav Das. The first draft of the manuscript was written by Amrita Talukdar and Gaurav Das. Both authors read and approved the final manuscript.
Data availability
The datasets generated during and analysed during the current study are available with the corresponding author on reasonable request and are not available publicly as per the permissions obtained from Institutional Ethics Committee (IEC).
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki and the Indian Good Clinical Practice. Approval was granted by the Institutional Ethics Committee.
Consent to participate
Waiver of consent was obtained from the Institutional Ethics Committee by virtue of this being a retrospective and observational study using de-identified patient information and variables already present in the hospital information system.
References
- Stenotrophomonas maltophilia: an emerging global opportunistic pathogen Brooke JS . Clinical Microbiology Reviews.2012;25(1). CrossRef
- Stenotrophomonas maltophilia: changing spectrum of a serious bacterial pathogen in patients with cancer Safdar A, Rolston KV . Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America.2007;45(12). CrossRef
- Microbiological and clinical aspects of infection associated with Stenotrophomonas maltophilia Denton M., Kerr K. G.. Clinical Microbiology Reviews.1998;11(1). CrossRef
- Risk factors associated with mortality of infections caused by Stenotrophomonas maltophilia: a systematic review Paez JJG , Costa S. F.. The Journal of Hospital Infection.2008;70(2). CrossRef
- Central venous catheter-related Stenotrophomonas maltophilia bacteraemia and associated relapsing bacteraemia in haematology and oncology patients Lai C.-H., Wong W.-W., Chin C., Huang C.-K., Lin H.-H., Chen W.-F., Yu K.-W., Liu C.-Y.. Clinical Microbiology and Infection: The Official Publication of the European Society of Clinical Microbiology and Infectious Diseases.2006;12(10). CrossRef
- Risk factors for mortality among patients with Stenotrophomonas maltophilia bacteremia in Tokyo, Japan, 1996-2009 Araoka H., Baba M., Yoneyama A.. European Journal of Clinical Microbiology & Infectious Diseases: Official Publication of the European Society of Clinical Microbiology.2010;29(5). CrossRef
- Risk factors for Stenotrophomonas maltophilia bacteremia in oncology patients: a case-control study Apisarnthanarak A, Mayfield JL , Garison T, McLendon PM , DiPersio JF , Fraser VJ , Polish LB . Infection Control and Hospital Epidemiology.2003;24(4). CrossRef
- A description of the type strain of Pseudomonas maltophilia. Int. Bull. Bacteriol Hugh R, Leifson E. Nomencl Taxon.1963;13:133-138.
- Stenotrophomonas, a new bacterial genus for Xanthomonas maltophilia (Hugh 1980) Swings et al. 1983 Palleroni N. J., Bradbury J. F.. International Journal of Systematic Bacteriology.1993;43(3). CrossRef
- Microbial contamination of suction tubes attached to suction instruments and preventive methods Yorioka K, Oie S, Kamiya A. Japanese Journal of Infectious Diseases.2010;63(2).
- Electronic ventilator temperature sensors as a potential source of respiratory tract colonization with Stenotrophomonas maltophilia Rogues A. M., Maugein J., Allery A., Fleureau C., Boulestreau H., Surcin S., Bebear C., Janvier G., Gachie J. P.. The Journal of Hospital Infection.2001;49(4). CrossRef
- Stenotrophomonas maltophilia contamination of nebulizers used to deliver aerosolized therapy to inpatients with cystic fibrosis Denton M., Rajgopal A., Mooney L., Qureshi A., Kerr K. G., Keer V., Pollard K., Peckham D. G., Conway S. P.. The Journal of Hospital Infection.2003;55(3). CrossRef
- Outbreak of Stenotrophomonas maltophilia bacteremia among patients undergoing bone marrow transplantation: association with faulty replacement of handwashing soap Klausner J. D., Zukerman C., Limaye A. P., Corey L.. Infection Control and Hospital Epidemiology.1999;20(11). CrossRef
- Nosocomial infections due to Xanthomonas maltophilia (Pseudomonas maltophilia) in patients with cancer Khardori N., Elting L., Wong E., Schable B., Bodey G. P.. Reviews of Infectious Diseases.1990;12(6). CrossRef
- Antibiotic susceptibility and outer membrane proteins of clinical Xanthomonas maltophilia isolates Cullmann W.. Chemotherapy.1991;37(4). CrossRef
- Susceptibility to beta-lactam antibiotics of mutant strains of Xanthomonas maltophilia with high- and low-level constitutive expression of L1 and L2 beta-lactamases Akova M., Bonfiglio G., Livermore D. M.. Journal of Medical Microbiology.1991;35(4). CrossRef
- Comparison of treatment with imipenem vs. ceftazidime as a predisposing factor for nosocomial acquisition of Stenotrophomonas maltophilia: a historical cohort study Carmeli Y., Samore M. H.. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America.1997;24(6). CrossRef
- Antimicrobial therapy for Stenotrophomonas maltophilia infections Nicodemo A. C., Paez JJG . European Journal of Clinical Microbiology & Infectious Diseases: Official Publication of the European Society of Clinical Microbiology.2007;26(4). CrossRef
- In vitro activities of antimicrobial combinations against clinical isolates of Stenotrophomonas maltophilia Liaw S, Teng L, Hsueh P, Ho S, Luh K. Journal of the Formosan Medical Association = Taiwan Yi Zhi.2002;101(7).
- Stenotrophomonas maltophilia drug resistance Sanchez MB , Hernandez A, Martinez JL . Future Microbiology.2009;4(6). CrossRef
- Therapeutic options for Stenotrophomonas maltophilia infections beyond co-trimoxazole: a systematic review Falagas ME , Valkimadi P, Huang Y, Matthaiou DK , Hsueh P. The Journal of Antimicrobial Chemotherapy.2008;62(5). CrossRef
- Multiple antibiotic resistance in Stenotrophomonas maltophilia Alonso A., Martínez J. L.. Antimicrobial Agents and Chemotherapy.1997;41(5). CrossRef
- Stenotrophomonas maltophilia resistant to trimethoprim-sulfamethoxazole: an increasing problem Al-Jasser AM . Annals of Clinical Microbiology and Antimicrobials.2006;5. CrossRef
- Global emergence of trimethoprim/sulfamethoxazole resistance in Stenotrophomonas maltophilia mediated by acquisition of sul genes Toleman MA , Bennett PM , Bennett DMC , Jones RN , Walsh TR . Emerging Infectious Diseases.2007;13(4). CrossRef
- Activities of ciprofloxacin and moxifloxacin against Stenotrophomonas maltophilia and emergence of resistant mutants in an in vitro pharmacokinetic-pharmacodynamic model Ba BB , Feghali H, Arpin C, Saux M, Quentin C. Antimicrobial Agents and Chemotherapy.2004;48(3). CrossRef
- Plasmid-mediated quinolone resistance: a multifaceted threat Strahilevitz J, Jacoby GA , Hooper DC , Robicsek A. Clinical Microbiology Reviews.2009;22(4). CrossRef
- Antimicrobial Treatment Strategies for Stenotrophomonas maltophilia: A Focus on Novel Therapies Gibb J, Wong DW . Antibiotics (Basel, Switzerland).2021;10(10). CrossRef
- Antibiotic combinations significantly more active than monotherapy in an in vitro infection model of Stenotrophomonas maltophilia Zelenitsky SA , Iacovides H, Ariano RE , Harding GKM . Diagnostic Microbiology and Infectious Disease.2005;51(1). CrossRef
- New antimicrobial agents for the treatment of bacterial infections in cancer patients Rolston KVI . Hematological Oncology.2009;27(3). CrossRef
- Attributable mortality of Stenotrophomonas maltophilia infections: a systematic review of the literature Falagas ME , Kastoris AC , Vouloumanou EK , Rafailidis PI , Kapaskelis AM , Dimopoulos G. Future Microbiology.2009;4(9). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2024
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times