Rare Case Report of Primary Small Cell Carcinoma of the Bladder
Download
Abstract
Small cell bladder carcinoma (SCBC) is a very rare entity. Compared to urothelial carcinoma they are more aggressive and have higher probabilities for metastases. Due to the aggressive nature of small cell bladder cancer, early diagnosis and treatment is imperative for the greatest chance of survival. We had two cases of non metastatic Small cell bladder carcinoma presenting at our institute and both were treated with definitive radiotherapy. One patient on follow up developed skeletal metastases and succumbed to disease, while the other patient is alive and disease free after 6 years. Here we present the challenges in diagnosis and treatment, and outcome of two SCBC patients treated at our institute.
Introduction
Small cell bladder carcinoma (SCBC) is a rare type of bladder cancer with a frequency less than 1% [1, 2]. Presentation could be same as transitional cell carcinoma of bladder, but correct diagnosis is very important in view of therapeutic and prognostic implications. They tend to present more aggressively and at later stages than the more common urothelial carcinomas, with higher probabilities for metastases. Retrospective studies have reported good outcome with organ preservation approach in SCBC [3, 4]. Here we present two cases of primary small cell carcinoma of bladder challenges in diagnosis, and outcome of bladder conservation treatment approach.
Case Presentation
Case 1
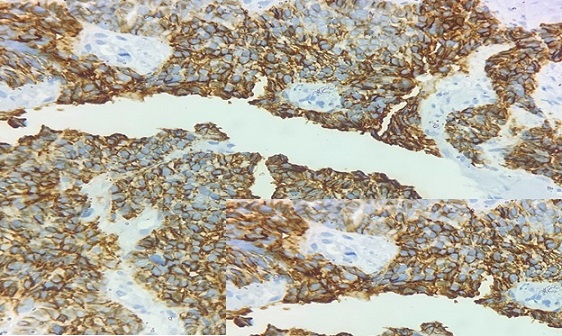
76 yearold male patient evaluated with complaints of dysuria, increased frequency of micturition and occasional hematuria. He was a chronic smoker. CT scan did showed bulky disease in urinary bladder with perivesical fat stranding. Patient underwent maximal TURBT. Histopathology examination of the TURBT specimen on microscopy showed infiltrative neoplasm arranged as sheets with scant intervening stroma. The cells had scant cytoplasm and hyperchromatic nucleus with inconspicuous nucleoli. Nuclear crowding and crush artifact were noted. Mitotic figures were brisk and areas of necrosis were noted. Perineural invasion was seen and neoplasm infiltrated muscularis propria. Immunohistochemistry showed CD56 and Synaptophysin positivity. Figure 1 shows Immunohistochemical study with diffuse CD 56 expression.
Figure 1. Shows CD 56 Expression.
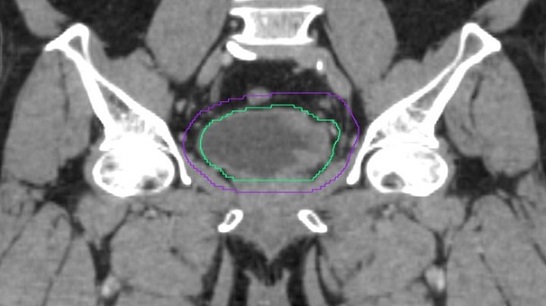
The final histopathology impression was Small cell neuroendocrine carcinoma. Patient had ECOG Performance status of 2 and had multiple comorbidities like Hypertension, Diabetes Mellitus, and Coronary artery disease. With CT imaging patient was staged as Carcinoma Urinary bladder c T3bN0M0. Case was discussed in Multispeciality tumor board and in view of old age multiple comorbidities it was decided to proceed with Definitive radiotherapy (RT). Planning CT scan showed tumor in superolateral wall of urinary bladder extending to distal ureter on left side with secondary hydroureteronephrosis. Patient was given definitive Radiotherapy with a dose of 60 Gy in 30 fractions. Figure 2 shows coronal CT image with clinical target volume (CTV) and planning target volume (PTV).
Figure 2. Coronal Planning CT Image with CTV (Green) and PTV (violet) .
Patient tolerated the planned course of Definitive RT well without any Grade III/IV toxicities. 3 months after completion of RT patient presented with paraparesis and MRI spine was suggestive of bone metastasis in multiple vertebral levels (D5, D6, D7 and L3). Patient was given palliative RT to the bone metastasis with a dose of 20 Gy in 5 fractions and patient succumbed to the disease one month later.
Case 2
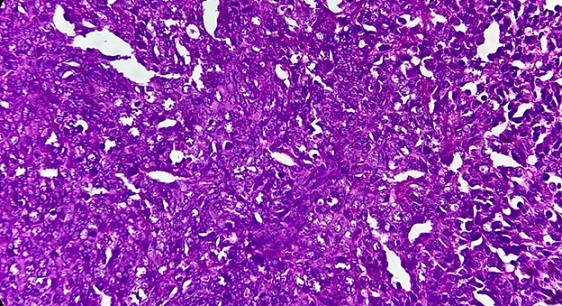
68 year old chronic smoker with complaints of difficulty in micturition and dysuria. Patient had ECOG Performance status of 1 with Diabetes Mellitus and Coronary artery disease as comorbidities. TURBT was done from an outside hospital and the slides and blocks of the same were reviewed in our hospital. Histopathology examination on microscopy showed invasive neoplasm with cells arranged in trabeculae, solid lobuled and nests. The cells were small with scant cytoplasm, hyperchromatic nuclei. Figure 3 shows High power view of individual tumor cells of small to Medium sized with scant cytoplasm, high N:C ratio, finely granular stippled chromatin and inconspicuous nucleoli (H and E, 40x).
Figure 3. Shows High Power View.
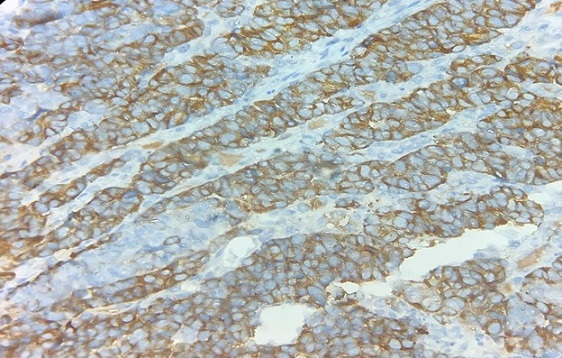
Nuclear debris were seen amidst tumor cells. Neoplastic cells were seen to invade deep muscle. Immunohistochemistry showed Ki 67 of 70-80% and Synaptophysin positivity. Figure 4 shows diffuse Synaptophysin expression on immunohistochemical staining.Final histopathology impression was small cell neuroendocrine carcinoma.
Figure 4. Shows Diffuse Synaptophysin Expression.
MRI pelvis done showed well defined heterogeneously enhancing polypoidal lesion with lobulated margins arising from right lateral wall of urinary bladder withfocal extension to perivesical regionand a suspicious right external iliac lymph node. PET CT scan was done for the patient and was reported as hypermetabolic primary malignancy of urinary bladder with no local or distant metastasis. After all investigations case was staged as Carcinoma Urinary Bladder cT3bN0M0. Case was discussed in Multispeciality board and the decision was to proceed with Neoadjuvant chemotherapy (NACT) followed by Definitive chemoradiation. Patient was given 2 cycles of neoadjuvant chemotherapy with Cisplatin & Etoposide combination. Post NACT patient treated with definitive chemoradiation. RT dose given was 60Gy in 30 fractions. During RT, patient was given one cycle of concurrent chemotherapy with Cisplatin & Etoposide combination. During Chemoradiation patient had Grade III hematological toxicity (thrombocytopenia), hence the fourth cycle chemotherapy was not given. Apart from that patient tolerated the planned course of chemoradiation well. After 75 months post treatment, patient is still disease free and coming for regular follow up.
Discussion
Among extrapulmonary small cell carcinoma (EPSCC), frequency of genitourinary location primary is much less compared to gastrointestinal location [5]. Most common presenting symptom is painlesshematuria and they can also present with dysuria, abdominal painand urinary obstruction and both of our patients presented with usual symptoms [6].
Investigations including cystoscopy and imaging are the same as for other bladder cancers. Diagnosis is based on histopathological examination as clinical andcystoscopic features are similar to urothelial carcinoma.Under light microscopy, small cell carcinoma is composed of small, round or oval cells, with prominenthyperchromatic nuclei, scant cytoplasm, granular chromatin. Extensive necrosis and high mitotic index are frequently seen.Immunohistochemical staining is positive for neuroendocrine markers, such as CD56, NSE, Synaptophysin, and Chromogranin-A [7, 8]. In both of our cases final histopathology impression was made only after immunohistochemical studies.
Both of our cases were treated with definitive radiotherapy with same radiotherapy dose of 60 Gy in 30 fractions. Several retrospective studies have used definitive RT dosage ranging from 56 Gy to 70 Gy [9-11]. In a published study on SCBC the median RT dose given was 60 Gy [12]. Organ preservation approach with concurrent chemotherapy and definitive RT have been reported in SCBC [3, 4]. One patient was given neoadjuvant as well as concurrent chemotherapy, but the other case was given only radical RT in view of multiple comorbidities, old age and poor performance status. In case of SCBC, there is no definite guideline to suggest either radical cystectomy or definitive radiotherapy as standard of care local treatment and in view of rarity of disease it is difficult to get a definitive conclusion regarding optimal local treatment through prospective studies. Some studies have reported improved survival outcome with addition of Neoadjuvant chemotherapy along with local treatment similar to small cell lung carcinoma [3, 13]. Among the two cases of SCBC treated at our centre, one patient who was treated with definitive RT alone, progressed at a distant site (bone) after 3 months period and the other patient who was treated with neoadjuvant chemotherapy followed by concurrent chemoradiation is still disease free after 75 months follow up period. Chemotherapy regimen used in our patient was Cisplatin & Etoposide combination as in similar study.Survival of patient who received chemotherapy was slightly higher and survival of patient who did not receive chemotherapy was comparable to a similar study [12]. Eventhough our experience of organ preservation approach in SCBC is only for two patients, our experience confirms the importance of adding systemic therapy as neoadjuvant and concurrent.
In conclusions, extrapulmonary small cell carcinoma (EPSCC) itself is rare and SCBC amounts for a very small proportion of EPSCC. Diagnosing SCBC needs detailed imaging and immunohistochemical studies and hence diagnosis is a challenge. In bladder carcinoma organ preservation approach is gaining popularity. In view of rarity of SCBC, there is paucity of definite treatment guidelines. Here we presented two cases of non metastatic SCBC treated with organ preservation approach. Though we cannot come to a definite conclusion from this case report, our experience suggest that organ preservation approach is a treatment option for SCBC. Addition of platinumbased chemotherapy as neoadjuvant and concurrent is essential to improve treatment outcome in terms of overall and disease free survival.
Acknowledgements
Conflict of interests
None to disclose.
We acknowledge the Pathology department, Malabar cancer center for providing us colour photography of the slides (H and E and IHC).
References
- Cancer statistics, 2008 Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ. CA: a cancer journal for clinicians.2008;58(2). CrossRef
- Primary small cell carcinoma of the urinary bladder Qayoom S, Chakrabarti D, Khan F, Goel MM . BMJ Case Reports.2019;12(9). CrossRef
- Treatment of Small Cell Carcinoma of the Bladder With Chemotherapy and Radiation after Transurethral Resection of a Bladder Tumor Bryant CM , Dang LH , Stechmiller BK , Gilbert SM , Morris SG , Zlotecki RA . American Journal of Clinical Oncology.2016;39(1). CrossRef
- Local control rate and prognosis after sequential chemoradiation for small cell carcinoma of the bladder Meijer RP , Meinhardt W, Poel HG , Rhijn BW , Kerst JM , Pos FJ , Horenblas S, Bex A. International Journal of Urology: Official Journal of the Japanese Urological Association.2013;20(8). CrossRef
- Clinical Overview of Extrapulmonary Small Cell Carcinoma Kim K, Lee H, Chun S, Shin S, Kim M, Lee K, Hyun M, Bae S, Ryoo H. Journal of Korean Medical Science.2006;21(5). CrossRef
- Small cell carcinoma of the urinary bladder. The Mayo Clinic experience Choong NWW , Quevedo JF , Kaur JS . Cancer.2005;103(6). CrossRef
- Collision Carcinoma Involving Small Cell Neuroendocrine Carcinoma and Squamous Cell Carcinoma of the Ureter: A Case Report and Review of the Literature Xu S, Xu L, Cao P, Yao S, Wu T, Hu X, Chen H, Gu J, Che X. Frontiers in Oncology.2021;11. CrossRef
- Clinicopathologic characteristics, therapy and outcomes of patients with primary ureteral small cell carcinoma: a case series and systematic review of the literature Zhong W, Lin R, Zhang L, Jin C, Li X, He Q, Gong K, He Z, Zhou L. OncoTargets and Therapy.2017;10. CrossRef
- Genitourinary small cell carcinoma: a retrospective review of treatment and survival patterns at The Ottawa Hospital Regional Cancer Center Asmis TR , Reaume MN , Dahrouge S, Malone S. BJU international.2006;97(4). CrossRef
- Small cell carcinoma of bladder: a single-center prospective study of 25 cases treated in analogy to small cell lung cancer Bex A, Nieuwenhuijzen JA , Kerst M, Pos F, Boven H, Meinhardt W, Horenblas S. Urology.2005;65(2). CrossRef
- Long-term survival after sequential chemoradiation for limited disease small cell carcinoma of the bladder Bex A, Vries R, Pos F, Kerst M, Horenblas S. World Journal of Urology.2009;27(1). CrossRef
- Organ-preserving approach via radiotherapy for small cell carcinoma of the bladder: an analysis based on the Japanese Radiation Oncology Study Group (JROSG) survey Akamatsu H, Nakamura K, Ebara T, Inaba K, Itasaka S, Jingu K, Kosaka Y, et al . Journal of Radiation Research.2019;60(4). CrossRef
- Phase II clinical trial of neoadjuvant alternating doublet chemotherapy with ifosfamide/doxorubicin and etoposide/cisplatin in small-cell urothelial cancer Siefker-Radtke AO , Kamat AM , Grossman HB , Williams DL , Qiao W, Thall PF , Dinney CP , Millikan RE . Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology.2009;27(16). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2024
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times