Adrenal Myelolipoma with Synchronous Ipsilateral Clear Cell Type Renal Cell Carcinoma: A Case Report with Review of Literature
Download
Abstract
Adrenal myelolipomas, typically benign and nonfunctional, are uncommon tumors found incidentally in the adrenal gland, unlike the more prevalent renal cell carcinoma in the kidney. The occurrence of synchronous renal cell carcinoma with adrenal myelolipomas is exceptionally rare, with only a few sporadic case reports documented in the literature spanning over six decades. Here, we present a case of a 67-year-old obese male who complained of colicky left upper abdominal pain, accompanied by a significant medical history of type 2 diabetes and hypertension. Ultrasonography revealed a large space-occupying lesion in the middle pole of the left kidney. Subsequently, left radical nephrectomy and adrenalectomy were performed, and the specimens were sent for histopathological examination, confirming the diagnosis of adrenal myelolipoma with synchronous renal cell carcinoma
Introduction
Adrenal myelolipoma, a rare, benign tumor of the adrenal gland, is typically nonfunctioning and often detected incidentally. It tends to manifest between the fifth to seventh decades of life, with no significant gender predilection [1]. Associated comorbidities may include obesity, hypertension, and diabetes. In contrast, renal cell carcinoma accounts for a small yet significant portion of oncological diagnoses (5% and 3% in men and women respectively) [2], with clear cell RCC being the most prevalent subtype, known for its aggressive behavior. RCC primarily affects individuals aged between sixth and seventh decades, and has a slightly higher incidence in males (1.5:1). Established risk factors for RCC encompass several lifestyle and genetic factors, including obesity, hypertension, diabetes, smoking, analgesic use, and hereditary RCC syndromes. While both adrenal myelolipoma and renal cell carcinoma are rare entities on their own, the synchronous occurrence of both tumors is exceptionally rare, with only a handful of sporadic cases reported in the medical literature over the past six decades.
In this report, we present a case of adrenal myelolipoma with synchronous renal cell carcinoma and conduct a comprehensive literature review to compile and analyze existing sporadic case reports, aiming to enhance our understanding of the biological behavior of these lesions.
Case report
A 67-year-old male presented to the outpatient department with a one-month history of left upper abdominal pain, characterized by colicky episodes occasionally radiating to the back. Physical examination revealed no significant findings, although the patient was obese and had a known history of Type 2 diabetes and hypertension for the past decade. Routine investigations, including biochemical, hematological parameters, and urine analysis, were within normal limits, and there was no significant family history.
Ultrasonography revealed a space-occupying lesion in the middle pole of the left kidney, without evidence of hydronephrosis. Subsequent Contrast Enhanced Computed Tomography (CECT) scan of the abdomen provided further characterization of the mass, demonstrating an exophytic heterogeneous enhancing space occupying lesion (SOL) measuring 5x4x4 cm in the middle part of the kidney, as well as a well-defined, nodular lesion measuring 5x3x2 cm containing fat in the left adrenal gland. The location and characteristics of these masses on CECT were suggestive of Renal Cell Carcinoma of the left kidney and left adrenal myelolipoma.
After ruling out the possibility of adrenal metastasis from renal cell carcinoma (RCC), given the well-defined lesion with a fat component in the adrenal gland, the patient underwent thorough preoperative evaluation, including assessment for metastases. Subsequently, left radical nephrectomy and adrenalectomy were performed en bloc through a left subcostal incision. The specimen was subjected to histopathological evaluation.
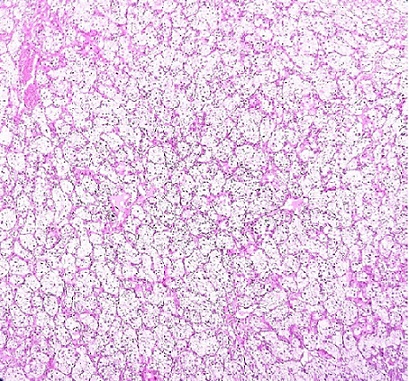
Gross examination revealed a large (5x3x3 cm), ill-defined growth with a variegated appearance in the middle part of the kidney near the capsule and adrenal gland, with yellowish hemorrhagic cut surface. Microscopic analysis identified a conventional clear cell type renal cell carcinoma of Fuhrman grade II, demonstrating capsular invasion without reaching Gerota’s fascia. The staging was determined as pT1b N0 M0 ( Figure 1).
Figure 1. Showing Compact Nests and Sheets of Cells with Clear Cytoplasm and Distinct Membranes. Suggestive of Clear Cell Type Renal Cell Carcinoma – Fuhrman grade II (H and E, X400).
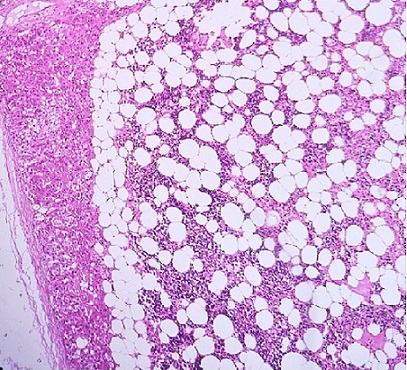
Furthermore, examination of the adrenal gland mass revealed the characteristic admixture of mature adipose tissue with all three hematopoietic elements, along with areas of hemorrhage, confirming the diagnosis of myelolipoma (Figure 2).
Figure 2. Showing Adrenal Myelolipoma Composed of Adipose Tissue Admixed with Tri-lineage Hematopoietic Cells. (H and E, X400).
Discussion
Myelolipoma of adrenal gland is a rare, benign tumor typically found unilaterally in the adrenal gland. It is often discovered incidentally and is composed of adipose tissue and hematopoietic elements. Myelolipoma was first described by Gierke [3], but the term “myelolipoma” was coined by Oberling in 1927 [4]. Most cases tend to be asymptomatic and are incidentally discovered through radiological imaging or autopsy, with a prevalence ranging from 0.1% to 0.2% [3]. Occasionally, they may present with acute retroperitoneal hemorrhage of acute onset [5]. Myelolipomas commonly occur in individuals between the fifth and seventh decades of life, with no specific sex predilection [1]. The majority of myelolipomas are non-functional.
Several conditions are often associated with adrenal myelolipoma, including Cushing’s disease, obesity, hypertension, and diabetes [5, 6]. It has been postulated that metaplastic changes within reticuloendothelial cells, triggered by factors such as necrosis, infection, or stress contribute to the development of myelolipomas [1, 7]. While asymptomatic small lesions typically do not require treatment, large myelolipomas or those causing hemorrhage may necessitate surgical excision with good prognosis.
In contrast, Renal cell carcinoma (RCC) represents a significant portion of oncological diagnoses worldwide, accounting for 5% and 3% of all cancer diagnoses in men and women, respectively, ranking as the sixth and tenth most frequently diagnosed cancer [2]. It is known for its aggressive nature and often fatal outcome. Among the various histological subtypes of RCC, the clear cell type is the most common, comprising 70-80% of all renal cancers [8, 9]. It is the most aggressive RCC subtype with the highest incidence noted in the sixth and seventh decade. Approximately 80% of RCC cases occur in individuals between 40 and 69 years, with a male-to-female ratio of 1.5:1 [10].
Various factors pose potential risks for renal cell carcinoma (RCC), including obesity, hypertension, type 2 diabetes, smoking, analgesic use, and urinary stones. Obesity exhibits a significant correlation with RCC [11], while a history of hypertension is linked to a 67% increase in RCC risk [12]. In women, the risk of RCC increases with the presence of multiple co-morbidities, such as obesity, hypertension, and type 2 diabetes, resulting in a four-fold increase compared to those without these conditions [13]. However, the association between RCC and type 2 diabetes remains uncertain, with the study conducted by Macleod et al. [14] unable to establish a definitive link. Furthermore, smoking emerges as an independent risk factor for RCC, as indicated by findings from the same study.Regular use of non-aspirin, non-steroidal anti-inflammatory drugs also poses an increased risk of RCC, as highlighted in a meta-analysis by Choueini et al. [15]. Additionally, a meta-analysis by Cheungpasitporn et al. [16] evaluated the association between history of kidney stone and RCC, suggesting a heightened RCC risk, particularly among males. Several hereditary RCC syndromes such as Von-Hippel-Lindau, constitutional translocation of chromosome 3, and tuberous sclerosis are associated with clear cell type of RCC [17].Despite considerable advancements in understanding and characterization of metastatic disease progression, especially in clear cell RCC, through microarray expression profile analysis [18, 19], there are currently no biomarkers suitable for daily clinical use in a diagnostic, prognostic and predictive individualized setting for RCC. Therefore, implementing a screening strategy in individuals at higher risk of RCC is an effective way of detection of asymptomatic disease, leading to earlier stage detection and better treatment outcomes.
The combination of adrenal myelolipoma, a rare tumor, with clear cell renal cell carcinoma, a more common renal neoplasm is a very rare phenomena. Literature spanning the last six decades [20-30] reports only a handful of cases (Table 1).
| Case | Reference/ Year | Age/Sex | Presenting Symptoms | Obesity | Hypertensive | Hormonal Activity | Radiological Diagnosis | Diagnosis/Findings | Size of Adrenal Ml | Size of Rcc | RCC Grading, Typing And Staging | Management |
| 1 | Lopez et.al. 1967 [20] | 63/M | Hematuria with abdominal mass on right side | yes | * | * | Plain x-ray - RCC. Myelolipoma incidental on surgical specimen | Myelolipoma with ipsilateral RCC | * | * | Clear cell type | Radical nephrectomy |
| 2 | Matsumoto et.al. 1993 [21] | 41/M | Left flank mass | no (175/76kg) | no | nil | USG - both tumours | Myelolipoma with contralateral RCC | 6 cm | 11 cm | Clear cell type grade I | Left nephrectomy with right adrenalectomy |
| CT - both tumours | pT2b N0M0 | |||||||||||
| 3 | Hofmockel et.al. 1995 [22] | 59/M | Essential hypertension | yes | yes | nil | USG - both tumours | Myelolipoma with contralateral RCC | 11 cm | 5 cm | Clear cell type grade II | Left nephrectomy with right adrenalectomy 2 months later |
| CT - both tumours with IVP | pT2bN0M0 | |||||||||||
| 4 | El-Mekresh et.al. 1996 [23] | 46/F | Loin pain with mass | nil | nil | nil | X-ray – RCC USG - both tumours | Myelolipoma with ipsilateral RCC | * | * | RCC | Radical nephrectomy |
| CT - both tumours | ||||||||||||
| USG - both tumours | ||||||||||||
| 5 | Sharma et.al. 1997 [24] | 56/M | Hematuria | nil | nil | * | USG and CT – Myelolipoma | Myelolipoma with ipsilateral RCC | 2 cm | Not specified | Clear cell type | Radical nephrectomy |
| detected after nephrectomy during metastatic workup | ||||||||||||
| 6 | Campagnacci et.al. 2006 [25] | 71/M | * | * | * | * | USG - both tumours | Myelolipoma with ipsilateral RCC | Not specified | 3.5 cm | Clear cell type | Laparoscopic radiofrequency renal ablation |
| CT - both tumours | ||||||||||||
| 7 | Bahrami et.al. 2009 [26] | Not mentioned | * | * | * | * | Nil | Myelolipoma with ipsilateral RCC | 6.5 cm | 2.5 cm | Clear cell type | Radical nephrectomy |
| 8 | Mahe et.al. 2010 [27] | 50/F | Flank pain with hematuria | * | yes | * | USG - both tumours | Myelolipoma in a a drenocortical adenoma with ipsilateral RCC | 5 cm | 2.5 cm | Clear cell type grade III | Concurrent Surgical resection |
| CT - both tumours | pT1bN0M0 | |||||||||||
| 9 | Lewitowiez et.al. 2014 [28] | 69/F | Flank and abdominal pain | * | no | nil | USG – only kidney | Myelolipoma in an adrenal mature ganglioneuroma with ipsilateral RCC with sarcomatoid component | 6.5 cm | 3.5 cm | Clear cell type grade IV | Trans-abdominal nephrectomy |
| CT – both tumours | pT1bN0M0 | |||||||||||
| 10 | Senthil et.al. 2015 [29] | 60/M | No complains (asymptomatic) | nil | yes | nil | CT – both tumours | Myelolipoma with ipsilateral RCC | 4 cm | 4 cm | Clear cell type grade II | Laparoscopic right nephrectomy with adrenalectomy |
| pT1bN0M0 | ||||||||||||
| 11 | J. Padilla et al. 2015 [30] | 44/M | Gross hematuria and left flank pain | * | yes | nil | CT - Both tumors | Myelolipoma with contralateral renal clear cell carcinoma | 6 cm | 7 cm | Clear cell type | Left laparoscopic nephrectomy with right laparoscopic adrenalectomy |
| Grade II | ||||||||||||
| Pt3n0m0 | ||||||||||||
| 12 | Jindal et al. 2022 [31] | 54/M | Discomfort in the right hypochondria | * | yes | nil | USG - both tumors | Myelolipoma with contralateral renal clear cell carcinoma | 12 cm | 61 cm | Clear cell type | Left nephrectomy with right adrenalectomy |
| CT - both tumors | grade 2 | |||||||||||
| pT1bN0M0 | ||||||||||||
| 13 | Present case 2024 | 67/M | Abdominal and flank pain | yes | yes | nil | USG – only kidney | Myelolipoma with ipsilateral RCC | 5 cm | 5 cm | Clear cell type grade II | Left radical nephrectomy with adrenalectomy |
| CT – both tumors | pT1bN0M0 |
These cases are sporadic and consist of single case reports. The table includes all published cases from the past 57 years, including the present case.
Patients’ ages ranged from 41 to 71 years, with the majority falling within their fifties and sixties, and a male predominance was noted. Presenting symptoms varied, ranging from asymptomatic to manifestations such as hematuria, abdominal pain, palpable mass or essential hypertension. Hormonal activity was absent in all cases, although observations of hypertension and obesity were noted. Diabetes was only reported in the present case.
Most of the cases were diagnosed based on imaging studies, using plain radiography, abdominal ultrasonography and CECT. Interestingly, adrenal myelolipoma was missed on ultrasonography in three cases, including the present one, but was detected on CECT. Ipsilateral involvement of the kidney was a predominant finding, with clear cell morphology observed in all cases. Fuhrman grade II was most commonly reported.
According to a comprehensive study conducted by Bahrami et al., [27] synchronous clear cell carcinomas of the kidney with adrenal masses of metastatic origin or non-functioning adenomas/hyperplasia are more prevalent than adrenal myelolipoma. Among 550 cases of radical nephrectomy with ipsilateral adrenalectomy specimens, they reported 80 cases of coexisting adrenal and renal masses. Most of the adrenal masses were adrenal adenoma / hyperplasia (56%) and metastatic tumors (43%) either through direct extension or by hematogenous spread of synchronous RCC. Only one case exhibited synchronous RCC of clear cell type and adrenal myelolipoma.
Lopex et.al., [21] documented the first case of concurrent RCC with myelolipoma of adrenal gland way back in 1967. The myelolipoma was incidentally discovered within the nephrectomy specimen undertaken for a sizable renal mass.
El-Mekrosh et. al., [24] reported a single case of myelolipoma originating from the adrenal gland, coexisting with ipsilateral RCC. The patient presented with symptoms of loin pain and a palpable mass. This case was part of a review focusing on the clinical, radiological, and histological characteristics of adrenal myelolipoma, encompassing eight cases out of a total of 72 cases of adrenal tumors.
Sharma et.al., [25] contributed seven additional cases of myelolipoma to the literature, providing insights into their clinical features, CT findings, and surgical therapeutic outcomes. Notably, one of these cases involved concurrent ipsilateral RCC.
Hofmockel et.al., [23] reported another case of myelolipoma of adrenal gland with contralateral RCC in 1995 and presented a review of well documented cases of adrenal myelolipoma reported during the last 10 years. No pathogenetic association was postulated between the two tumors.
Matsumoto et.al., [22] reported a case of adrenal myelolipoma associated with contralateral RCC of clear cell type keeping in mind the possibility of renal cell carcinoma metastasis to the contralateral adrenal.
Mahe et.al., [28] documented an exceptional case of tumor trifecta: a myelolipoma developing within an adrenocortical adenoma on the same side as a synchronous clear cell renal cell carcinoma. They conducted a comprehensive literature review focusing on the epidemiological, histological, and immunohistochemical characteristics of adrenal tumors. This review aids in discerning the origin and potential malignancy of adrenal lesions.
Lewitowicz et.al., [29] presented an unusual case report detailing the coexistence of clear cell renal cell carcinoma with a sarcomatoid component alongside adrenal mature ganglioneuromas containing myelolipoma. They conducted a thorough review of literature to analyze genetic abnormalities associated with both clear cell sarcomatoid RCC, adrenal myelolipoma, and ganglioneuromas.
Campagnacci et.al., [26] proposed laparoscopic radiofrequency renal ablation (RFA) as a potentially effective and less morbid procedure for small renal tumors, despite its higher surgical supply cost. They based this suggestion on their experience performing RFA on three cases of RCC, one of which involved an adrenal myelolipoma alongside ipsilateral RCC of clear cell type. Prior to RFA, laparoscopic adrenalectomy was conducted for the myelolipoma.
Senthil et.al., [30] reported laproscopic management of both adrenal and renal tumor through laproscopic adrenelectomy with nephrectomy for ipsilateral synchronous RCC and adrenal myelolipoma as a safe, minimally invasive and feasible procedure for surgical treatment.
In conclusion, the coexistence of adrenal myelolipoma and clear cell renal cell carcinoma, although individually rare, appears exceptionally uncommon based on an extensive 57-year literature review. This condition primarily affects individuals in their fifties and sixties, with a notable tendency for ipsilateral involvement of both organs. CT scan emerges as the most effective diagnostic tool for detecting these lesions and for excluding the possibility of metastatic disease in cases of ipsilateral gland involvement. While obesity and hypertension are significant risk factors for each lesion independently, their role in the occurrence of both tumors together is less clearly defined. Notably, no hormonal activity was observed in any of the reported cases.
Acknowledgments
Statement of Transparency and Principals:
• Author declares no conflict of interest
• Study was approved by Research Ethic Committee of author affiliated Institute.
• Study’s data is available upon a reasonable request.
• All authors have contributed to implementation of this research.
References
- Myelolipoma. www.pathologyoutlines.com Cevik L, Parwani A. 2022.
- Cancer statistics, 2023 Siegel RL , Miller KD , Wagle NS , Jemal A. CA: a cancer journal for clinicians.2023;73(1). CrossRef
- Uber knochenmarksgewebe in den nebenniene. Gierke E. Beitn Pathol Anat.1970;7:311-325.
- Les formations myelolipomatouses Obenling C. Bull Cancer.1929;18:234-46.
- Adrenal myelolipoma. Radiology Reference Article Weerakkody Y. Radiopaedia.org.2024.
- Computed Body Tomography with MRI Correlation Joseph , Sagel SS , Stanley RJ , Heiken JP . Lippincott Williams & Wilkins.2015.
- Presentation and therapy of myelolipoma Meyer A, Behrend M. International Journal of Urology: Official Journal of the Japanese Urological Association.2005;12(3). CrossRef
- Prognostic impact of histologic subtyping of adult renal epithelial neoplasms: an experience of 405 cases Amin MB , Tamboli P, Javidan J, Stricker H, Venturina M, Deshpande A, Menon M. The American Journal of Surgical Pathology.2002;26(3). CrossRef
- Prognostic utility of the recently recommended histologic classification and revised TNM staging system of renal cell carcinoma: a Swiss experience with 588 tumors Moch H., Gasser T., Amin M. B., Torhorst J., Sauter G., Mihatsch M. J.. Cancer.2000;89(3).
- Epidemiology of kidney cancer Pascual D., Borque A.. Advances in Urology.2008;2008. CrossRef
- Obesity and renal cell cancer--a quantitative review Bergström A., Hsieh C. C., Lindblad P., Lu C. M., Cook N. R., Wolk A.. British Journal of Cancer.2001;85(7). CrossRef
- Blood pressure and kidney cancer risk: meta-analysis of prospective studies Hidayat K, Du X, Zou S, Shi B. Journal of Hypertension.2017;35(7). CrossRef
- Type 2 diabetes and the risk of renal cell cancer in women Joh H, Willett WC , Cho E. Diabetes Care.2011;34(7). CrossRef
- Risk factors for renal cell carcinoma in the VITAL study Macleod LC , Hotaling JM , Wright JL , Davenport MT , Gore JL , Harper J, White E. The Journal of Urology.2013;190(5). CrossRef
- Analgesic use and the risk of kidney cancer: a meta-analysis of epidemiologic studies Choueiri TK , Je Y, Cho E. International Journal of Cancer.2014;134(2). CrossRef
- The risk of kidney cancer in patients with kidney stones: a systematic review and meta-analysis Cheungpasitporn W., Thongprayoon C., O'Corragain O. A., Edmonds P. J., Ungprasert P., Kittanamongkolchai W., Erickson S. B.. QJM: monthly journal of the Association of Physicians.2015;108(3). CrossRef
- Hereditary renal cancer syndromes: an update of a systematic review Verine J, Pluvinage A, Bousquet G, Lehmann-Che J, Bazelaire C, Soufir N, Mongiat-Artus P. European Urology.2010;58(5). CrossRef
- Gene signatures of progression and metastasis in renal cell cancer Jones J, Otu H, Spentzos D, Kolia S, Inan M, Beecken WD , Fellbaum C, et al . Clinical Cancer Research: An Official Journal of the American Association for Cancer Research.2005;11(16). CrossRef
- Gene expression in kidney cancer is associated with cytogenetic abnormalities, metastasis formation, and patient survival Sültmann H, Heydebreck A, Huber W, Kuner R, Buness A, Vogt M, Gunawan B, et al . Clinical Cancer Research: An Official Journal of the American Association for Cancer Research.2005;11(2 Pt 1).
- Myelolipoma of the adrenal gland and kidney adenocarcinoma: clinical case López Engelking R., Ibarra Esparza X., Jiménez Velasco D., Maldonado E.. The Journal of Urology.1967;98(4). CrossRef
- [A case of adrenal myelolipoma associated with renal cell carcinoma] Matsumoto K., Takahashi O., Yajima H., Koya A., Kobayashi M., Yamanaka H.. Hinyokika Kiyo. Acta Urologica Japonica.1993;39(1).
- Myelolipoma of the adrenal gland associated with contralateral renal cell carcinoma: case report and review of the literature Hofmockel G., Dämmrich J., Manzanilla Garcia H., Frohmüller H.. The Journal of Urology.1995;153(1). CrossRef
- Clinical, radiological and histological features of adrenal myelolipoma: review and experience with a further eight cases El-Mekresh M. M., Abdel-Gawad M., El-Diasty T., El-Baz M., Ghoneim M. A.. British Journal of Urology.1996;78(3). CrossRef
- Symptomatic adrenal myelolipoma. Clinicopathological analysis of 7 cases and brief review of the literature Sharma M. C., Kashyap S., Sharma R., Chumber S., Sood R., Chahal R.. Urologia Internationalis.1997;59(2). CrossRef
- Laparoscopic radiofrequency renal ablation in patients with simultaneous visceral tumors: long-term follow-up Campagnacci R., Guerrieri M., De Sanctis A., Sarnari J., Lezoche E.. Journal of Endourology.2006;20(5). CrossRef
- Synchronous renal and adrenal masses: an analysis of 80 cases Bahrami A, Truong LD , Shen SS , Krishnan B. Annals of Diagnostic Pathology.2009;13(1). CrossRef
- A "tumour trifecta:" myelolipomata arising within an adrenocortical adenoma ipsilateral to a synchronous clear cell renal cell carcinoma Mahe E, El-Shinnawy I. The Malaysian Journal of Pathology.2010;32(2).
- Coexistence of renal cell carcinoma of clear cell type with sarcomatoid cell type component and adrenal mature ganglioneuroma with myelolipoma - a case of 69-year-old female patient Lewitowicz P, Wincewicz A, Horecka-Lewitowicz A, Matykiewicz J, Kozieł D, Głuszek S, Sulkowski S. Romanian Journal of Morphology and Embryology = Revue Roumaine De Morphologie Et Embryologie.2014;55(2). CrossRef
- Laparoscopic Nephrectomy with Adrenalectomy for Synchronous Adrenal Myelolipoma and Renal Cell Carcinoma Senthil K, Ramalingam M, Janardhan K, Murugesan A, Pai MG . Case Reports in Urology.2015;2015. CrossRef
- Tumor renal izquierdo y tumor suprarrenal derecho: abordaje laparoscópico en el mismo tiempo quirúrgico Padilla-Piña J., García-Vásquez R. A., Arriaga-Aguilar J., Vega-Castro R., Pérez-Manzanares V. M., Zárate-Morales A., Gerardo-Osuna I., Garcia-Díaz M.. Revista Mexicana de Urología.2015;75(3). CrossRef
- Concurrent laparoscopic management of giant adrenal myelolipoma and contralateral renal cell carcinoma Jindal T, Pawar P, Subedi N. Asian Journal of Urology.2022;9(1). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2024
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times