A Comparative Study of 3D Conformal Radiotherapy Versus Intensity Modulated Radiotherapy with Simultaneous Integrated Boost in Locally Advanced Head and Neck Cancer Patients
Download
Abstract
Introduction: Role of radiotherapy in comprehensive management of head and neck cancer for achieving tumor control and organ preservation is now well established and radiotherapy is routinely used as definitive or in the adjuvant setting after surgery, concurrently with chemotherapy or targeted agents. Development of linear accelerator with Multileaf Collimator (MLC) have revolutionized radiation delivery techniques, allowing conformal and Intensity Modulated Radiotherapy (IMRT) to deliver highly conformal sculpted radiation dose to a very complex structure with improved sparing of adjoining critical structures like salivary glands, spinal cord, eyes, and brainstem amounting to better therapeutic gain.
Aim and Objective: This prospective study is to compare toxicity profile of IMRT-SIB with Three Dimensional Conformal Radiotherapy (3D CRT) in head and neck cancer.
Materials and Methods: A total of 80 patients with proven head and neck cancer were included in the study. They underwent radiotherapy on Linac 2300 CD for 3D-CRT and TRUEBEAM SVC machine for the IMRT comprised of 40 patients in each arm. Patients received 66Gy/30 fractions, as radical treatment in the IMRT arm for 6 weeks and 66 Gy/33 fractions in the 3DCRT arm for 6.5 weeks from Monday to Friday.
Results: The 3D-CRT group demonstrated significantly more acute toxic effects compared with the IMRT group in our analysis. Acute Grade 3 or greater toxic effects to the skin occurred in 7 of 40 (17.5%), patients in the 3D-CRT group compared with 3 of 40 (7.5%) patients in the IMRT group. Acute Grade 3 or greater toxic effects to the mucous membranes occurred in 15 of 40 (37.5%) patients in the 3D-CRT group and only 9 of 40 (22.5%) patients in the IMRT group. Statistically significant grade III dysphagia developed in 8 of 40 (20%) patients in 3D-CRT group compared with 4 of 40 (10%) patients in IMRT group, while significant grade II xerostomia developed after 6 month of treatment; 20 of 40 patients in 3D-CRT group (50%), compared with 13 of 40 (32.5%) patients in IMRT group.
Conclusion: In our comparative study, IMRT was associated with a significantly lower incidence of Grade 3 or greater xerostomia, acute toxic effects to skin (dermatitis) and mucous membranes (mucositis) than 3DCRT. In addition, compared to 3D-CRT, IMRT had lower rates of feeding tube use during radiotherapy. Our analysis showed potentially less toxicity in patients treated with IMRT in comparison to 3D-CRT.
Introduction
Cancers are amongst one of the leading causes of morbidity and mortality worldwide, with approximately 19.97 million new cases, 9.74 million cancer related deaths in 2022 and 53.50 million prevalent cases in all age groups [1].
The International Agency for Research on Cancer estimated that one in 5 people worldwide develop cancer during their lifetime, where one in 8 men and one in 11 women die from the disease [2]. The ten most common cancer accounts for more than 60% of the newly diagnosed cancer cases and more than 70% of the cancer deaths [3]. In Indian scenario, 1.41 million new cases of cancer were estimated, indicating India as a single country (of the 185 countries) contributing to 10.43% of the global cancer burden; mortality figures were 9,16,827 contributing to 7.05% of global cancer deaths and 32,58,518 prevalent cases in 2022. Incidence rates of cancer were higher in females with 7, 22,138 and 6,91,178 in males in the same year [4].
The head and neck cancers accounts for almost 2,54,287 new cases annually, 60,922 in females and 1,93,364 in males in the country [4]. The ASIR (Age-Standard Incidence Rate) for HNC was 25.9 (95% CI25.7-26.1) and 8.0 (95% CI 79-8.1) per 100,000 population for males and females, respectively [5].
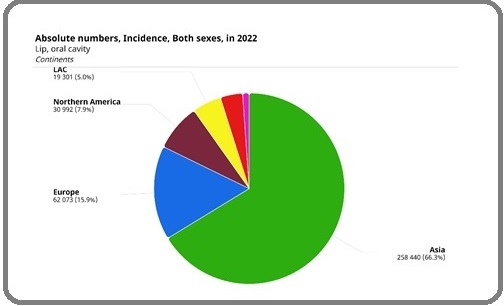
India has the highest burden of HNC in the world, accounting for about 30–35% of global cases. Over 100,000 new cases of head and neck cancers are registered every year in India, also expressed in Figure 1 [6].
Figure 1. Incidence of Oral Cavity Cancers Worldwide; Data, Cancer Today (GLOBOCON 2022).
Amongst these, nearly 60% have non-metastatic locally advanced disease. The cancer of the head and neck are found to be progressing at a Compound annual growth rate (CAGR) of 23 per cent [7].
Overall, 57.5% of global head and neck cancers occur in India. Head and neck cancers in India accounted for 30% of all cancers. In India, 60 to 80% of patients present with advanced disease as compared to 40% in developed countries [8].
Worldwide, head and neck cancer (HNC) is seventh most common cancer overall; fifth most common in men and the 12th most common in women [8]. Head and neck cancers originate from squamous cells located in the mucosal epithelium and are further classified by the anatomical area in which they arise. Head and neck squamous cell carcinoma (HNSCC) includes the lip, oral cavity, salivary glands, nasopharynx, oropharynx, hypopharynx, larynx, nasal and paranasal cavity, and ear [9].
The risk factors associated with HNSCC are environmental and lifestyle factors such as chewing tobacco, alcohol consumption and smoking. Some unknown factors play essential roles in tumorigenesis, tumor progression, and metastasis of HNC, such as alteration in microbial diversity and function, genetic polymorphisms in enzymes involved in alcohol and tobacco metabolism or, genetic predisposition as is in Li Fraumeni’s syndrome, Fanconi’s anemia and ataxia telangiectasia. [10] Recently, epidemiological studies have emerged a strong positive association with human papillomavirus (HPV) in subset of HNSCC. Other associated risk factors include poor dental hygiene, malnutrition, and immuno-suppression, pre malignant features like, sub-mucous fibrosis, leukoplakia, and erythroplakia, gastro-intestinal reflux, different inherited syndromes and chronic iron deficiency anemia [11]. Quality of life is poor, as they suffer from socially awkward conditions and are persistently suffer with pain, bleeding, mucositis, dysphagia, excessive salivating and the most disturbing is proliferative growth that disfigures the face. Radiotherapy is the main non-surgical treatment for squamous cell carcinoma of head and neck (HNSCC) [12].
High rates of local tumor control can be achieved with 5-year survival greater than 80% for stage 1 and 2 and 60-70% for stage 3 and 4 tumors. However, long-term sequelae of radiotherapy are highly prevalent and has severe adverse effects on quality of life (QOL) [13].
Standard of care for locally advanced squamous cell head and neck carcinoma is Chemo-radiation. The advent of Intensity Modulated Radiotherapy (IMRT) has facilitated high conformity in dose shaping, delivering of non-uniform fluence treatment beam and optimizing composite dose distribution, and thus, providing higher dose to the target volumes, and simultaneously limiting the dose to organ at risk and resulting in decreased toxicity to the normal structures.
It spares normal structures such as salivary glands, optic nerves, brain stem and spinal cord. It facilitates treatment dose delivery in a single treatment phase plan for the entire course of the treatment with different radiation doses and intensities, appropriate for gross tumor volume (GTV) and elective nodal region, including CTV, and is advantageous as matching of additional fields, tumor boosts and the need for electron fields to the posterior (level II, V) neck nodes are eliminated. It offers the possibility of simultaneously delivering higher radiation doses to the region of gross disease and lower doses to the areas of microscopic diseases, and is so called simultaneous integrated boost, SIB-IMRT.
The study is intended to compare and analyze the 3D conformal radiotherapy versus intensity modulated radiotherapy with simultaneous integrated boost radiation therapy for locally advanced head and neck cancer.
Aims and Objectives
To compare efficacy and adverse effects of 3D conformal radiotherapy (3D-CRT) with simultaneous integrated boost-IMRT (SIB-IMRT) with concurrent chemotherapy in locally advanced head and neck cancer patients.
Study Arm A (3D-CRT) Dose 2.0 Gy/#, 1#/day, 5 days a week, Total tumor dose: 66Gy. (Total number of fractions: 33)
Study Arm B (IMRT) Dose 2.2 Gy/#, 1#/day, 5days a week, Total tumor dose: 66Gy. (Total number of fractions: 30)
Materials and Methods
The present prospective analytical study was conducted in Acharya Tulsi Regional Cancer Treatment and Research Institute, Sardar Patel Medical College, Bikaner. It was done on 80 histologically proven new cases of locally advanced head and neck cancer with age 18-70 years with European Co-operative Oncology Group (ECOG) performance status 0-2. Patients with distant metastases, other concurrent malignancies and pregnant and lactating women were excluded from the study. Complete history with general physical and systemic examination was done. Local examination of larynx was done by direct and indirect laryngoscopy. Complete blood count, liver and renal function tests, X-ray soft tissue neck and chest, Ultrasonography of abdomen and pelvis and CE-CT scan of head and neck were done wherever required. Tissue diagnosis was done by biopsy.
Study Design
All 80 enrolled patients of III-IVB were treated by radiotherapy and randomized into either of the two arms Arm A (3D-CRT) and Arm B (IMRT). In the 3D conformal RT arm, patients were irradiated by 6 MV photon obtained by LINAC tele therapy machine CLINAC 2300CD, and Eclipse Treatment Planning System (T.P.S.) version 13.7. MLC shaped fields from three to five beams were placed to achieve homogeneity. The total dose of 66 Gy was delivered in 33 fractions, 2 Gy per fraction, one fraction per day, where PTV-high was given 66 Gy in 33 fractions. PTV-low risk was 44 Gy in 22 fractions. After 44 Gy, off cord dose reduction was done for spinal cord sparing, and posterior cervical nodes were treated with electron therapy, if needed. Patients were irradiated 5 days in a week from Monday to Friday. In the IMRT SIB arm, patients were irradiated by Inverse planning method performed in Eclipse Treatment Planning System (T.P.S.) version 15.6, by iso-centric technique where 6MV photon were obtained by TRUEBEAM SVC tele therapy machine. The aim was to reduce mean dose to 26 Gy or less for at least one parotid gland, or the lowest possible mean dose, whilst maintaining target coverage. Treatment set up consisted of five to seven beams.
Biological effective dose (BED)
The schedule of IMRT arm was planned by equating the Biological Effective Dose (BED) calculations, considering the conventional value of α/β = 10 for acute effects.
BED = D [1+ d/ (α/β)]; where D is the total dose, and d is dose per fraction.
BED Calculation for 3DCRT arm: BED for early effects For GTV = 2 x 33 (1+2/10)= 79.2 Gy
BED Calculation for IMRT arm: BED for early effects For PTV1 = 2.2 x 30 (1+2.2/10) = 80.52 Gy
Patients from both the arms received Cisplatin on a three weekly basis with a dose of 100mg/m2, as a part of the concurrent chemotherapy treatment, and were assessed weekly for local disease response.
The response evaluation were done at the completion of radiotherapy, and later at 3rd month and 6th month. Patients were categorized as per RECIST Criteria version 1.1 (Response Evaluation Criteria in Solid Tumors) and similarly, the toxicities were scored according to the CTCAE version 5.0 (Common Terminology Criteria for Adverse Events) for acute and late toxicities in both arms of treatment groups, and were monitored at the end of treatment, 3rd month and at 6th month. Symptoms were recorded as visible lesions in oral cavity and oropharynx, symptoms like, dysphagia, odynophagia, xerostomia, dermatitis, mucositis, and nasogastric feeding intubation. Data are coded and recorded in MS Excel spreadsheet program. SPSS v23 (IBM Corp.) is used for data analysis. Descriptive statistics are elaborated in the form of means/standard deviations and medians/IQRs for continuous variables, and frequencies and percentages for categorical variables. Data are presented in a graphical manner wherever appropriate for data visualization using histograms/box-and- whisker plots/column charts for continuous data and bar charts/pie charts for categorical data. P-value of <0.05 was considered significant. Data is presented in the form or tables and bar diagrams.
Results
In this study, majority of the patients were in their 4th decade of life with age in range of 18-70 years and median age was 48 years for 3DCRT arm and 52 years for the IMRT arm. Majority of the patients were male 82.5% in 3DCRT arm and 62.5% in the IMRT arm. ECOG Performance status ranged from 0-2. Majority of the population study had ECOG score 0. Histologically, throughout the study population, patients had Squamous Cell carcinoma (SCC). Well differentiated histology was present in 50% and 42.5% patients in 3D-CRT and IMRT arms, respectively, in Table 1.
| Demographic Characteristics | IMRT | 3D-CRT | |
| Age Groups | 21-30 Years | 4 | 2 |
| 31-40 Years | 6 | 10 | |
| 41-50 Years | 11 | 12 | |
| 51-60 Years | 13 | 9 | |
| 61-70 Years | 6 | 7 | |
| Sex | Male | 25 | 33 |
| Female | 15 | 7 | |
| ECOG | 0 | 30 | 28 |
| 1 | 6 | 10 | |
| 2 | 4 | 2 | |
| Histo-pathological Examination | WDSCC* | 17 | 20 |
| MDSCC# | 17 | 14 | |
| PDSCC@ | 6 | 6 | |
| Smoking/Tobacco | NO | 13 | 16 |
| YES | 27 | 24 |
* WDSCC - Moderately differentiated squamous cell carcinoma; # MDSCC - Well differentiated squamous cell carcinoma; @ PDSCC - Poorly differentiated squamous cell carcinoma
In this population, 10 and 16 patients of oral cavity disease, 20 and 16 patients of oropharynx lesion, 7 and 6 patients had hypo-pharyngeal disease and 3 and 2 patients had laryngeal carcinoma from 3D-CRT and IMRT study arms.
60% vs 67.5% of the patients gave a history of smoking/tobacco chewing or both in the IMRT and 3D-CRT arms.
Figure 2 shows tumor stage of the patients. Among 3DCRT arm, 45% patients had stage IIIA, 37.5% had IVA and 17.5% were stage IVB disease.
Figure 2. Disease Stage of Study Patients.

In the IMRT arm 40% patients were of stage IIIA, 45% were of stage IVA and 15% were stage IVB disease as given in Table 2.
| Stage group | 3DCRT | IMRT |
| III A | 18 (45) | 16 (40) |
| IVA | 15 (37.5) | 18 (45) |
| IVB | 7 (17.5) | 6 (15) |
| Total | 40 | 40 |
Grade II skin toxicity in both the arms were significant (p=0.008). As given in Table 3, Grade 3 toxicity was seen in 6th week in both the arms; 7 patients (17.5%) in the 3D-CRT arm and 3 (7.5%) patients in the IMRT arm, (p=0.016), indicating a significant toxicity profile, while comparing both the arms. No cases of grade IV dermatitis was seen.
| Treatment Duration | 3D-CRT Grade- Dermatitis | IMRT Grade- Dermatitis | ||||||||
| 0 | I | II | III | IV | 0 | I | II | III | IV | |
| 2 nd week | 15 | 25 | 0 | 0 | 0 | 21 | 19 | 0 | 0 | 0 |
| 4 th week | 0 | 17 | 21 | 2 | 0 | 2 | 20 | 18 | 0 | 0 |
| 6 th week | 0 | 13 | 20 | 7 | 0 | 0 | 14 | 23 | 3 | 0 |
| 1 month after treatment | 6 | 22 | 12 | 0 | 0 | 8 | 24 | 8 | 0 | 0 |
| 3 months after treatment | 27 | 13 | 0 | 0 | 0 | 30 | 10 | 0 | 0 | 0 |
Xerostomia was reported by the patients at 4th week, end of the treatment, at 1 month, at 3 month, and 6 month follow up after treatment. At 1 month after the treatment, 11 (27.5%) patients had grade I and 29 (72.5%) patients had grade II xerostomia, while in the IMRT arm, 20 (50%) had grade I and 20 (50%) had grade II, making it significant with a p value of 0.05. 3 months after the treatment, 18 patients had grade I and 22 had grade II xerostomia in the 3D-CRT arm, where as in the IMRT arm 2 had grade 0, 8 had grade I and 31 had grade II of xerostomia (p=0.03). At 6 months after treatment, in the 3DCRT arm, 20 patients had grade I and 20 had grade II xerostomia, where in the Figure 3-4 IMRT arm, 4 had grade 0, 23 had grade I, and 13 had Grade II xerostomia.
Figure 3. Xerostomia in 3D-CRT arm.

Figure 4. Xerostomia in IMRT arm.
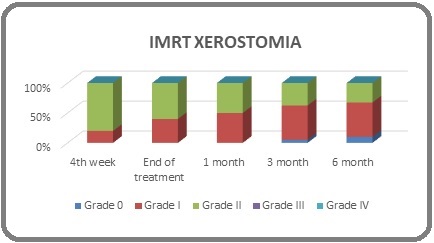
P=0.03. While comparing both the arms, throughout the duration of treatment the results were comparative in both the arms, but in the 6th month after the treatment completion, xerostomia was seen 12.5% higher incidence in the 3DCRT arm, shown in Table 4.
| Treatment Duration | 3D-CRT Grade- Xerostomia | IMRT Grade- Xerostomia | ||||||||
| 0 | I | II | III | IV | 0 | I | II | III | IV | |
| 4 th week | 0 | 3 | 37 | 0 | 0 | 0 | 8 | 32 | 0 | 0 |
| End of treatment | 0 | 6 | 34 | 0 | 0 | 0 | 16 | 24 | 0 | 0 |
| 1 month after treatment | 0 | 11 | 29 | 0 | 0 | 0 | 20 | 20 | 0 | 0 |
| 3 months after treatment | 0 | 18 | 22 | 0 | 0 | 2 | 23 | 15 | 0 | 0 |
| 6 months after treatment | 0 | 20 | 20 | 0 | 0 | 4 | 23 | 13 | 0 | 0 |
Grade 3 and above dysphagia were seen in the 4th to 6th week of treatment in the 3D-CRT arm in 2 and 6 patients respectively, where as in the IMRT arm, it was majorly seen in 6th week, in 4 patients (10%). Grade III, (p=0.029), suggested a significant difference in both the arms of the study group in favor of grade III dysphagia. Though no grade IV dysphagia was seen during or after treatment in any of the arms.
Mucositis experienced by enrolled patients in the study groups. Grade 3 and above mucositis was seen in the 4th to 6th week in the 3D-CRT arm as 3 (7.5%) and 15 (37.5%) patients respectively. Grade II mucositis in 3D-CRT arm is higher than IMRT, and thus significant with a p value of 0.0016. In the IMRT arm, 8 (20%) patients had grade III mucositis seen in the 9 (22.5%) of the patients, (p= 0.0006). No grade IV mucositis were seen, as in Table 5.
| Treatment Duration | 3D-CRT Grade- Mucositis | IMRT Grade- Mucositis | ||||||||
| 0 | I | II | III | IV | 0 | I | II | III | IV | |
| 2 nd week | 30 | 10 | 0 | 0 | 0 | 31 | 9 | 0 | 0 | 0 |
| 4 th week | 2 | 21 | 14 | 3 | 0 | 5 | 22 | 13 | 0 | 0 |
| 6 th week | 0 | 2 | 23 | 15 | 0 | 0 | 5 | 26 | 9 | 0 |
| 1 month after treatment | 4 | 20 | 16 | 0 | 0 | 6 | 22 | 12 | 0 | 0 |
| 3 months after treatment | 11 | 17 | 12 | 0 | 0 | 13 | 18 | 9 | 0 | 0 |
| 6 months after treatment | 32 | 8 | 0 | 0 | 0 | 35 | 5 | 0 | 0 | 0 |
The incidence of patients who had to take support of Nasogastric tube for feeding during treatment due to symptoms like dysphagia and mucositis. In the 3D-CRT arm 13 patients were intubated with NG tube where most of them were in the 6th week i.e. 10 patients (25%) and 3 patients (7.5%) in the 4th week, in Table 6.
| Intubation of NG tube | 3D-CRT | IMRT |
| 2 nd week | 0 | 0 |
| 4 th week | 3 (7.5%) | 0 |
| 6 th week | 10 (25%) | 7 (17.5%) |
| 1 month | 0 | 0 |
| 3 months | 0 | 0 |
| 6 months | 0 | 0 |
| Total | 13 (32.5%) | 7 (17.5%) |
Similarly in the IMRT arm, 7 patients had to undergo nasogastric tube intubation, especially in the 6th week of treatment with 7 patients (17.5%) (p=0.003).
Interruptions in the treatment schedule in the patients of both the arms had multiple reasons, including patient’s toxicity profile, unexpected event in the family, or the breakdown of the system. Overall, 22 patients in the 3D-CRT arm and 25 patients in the IMRT arm completed their treatment without any disruptions or gaps; (p value = 0.065), suggesting the gaps in the treatment schedule of both arms are comparative and insignificant.
The patients enrolled in the study who had an upward trend towards weight loss during treatment phase. In the 3D-CRT arm 14 (35%) patient’s and in the IMRT arm, 8 (20%) patients had >10 % weight loss. Weight loss is higher in the 3DCRT arm by 15% when compared to IMRT, with a significant (p value = 0.032).
Treatment Response
The response evaluation for disease control according to the RECIST criteria at 3 months and 6 months follow up after completion of treatment. On follow up at 3 months after treatment, 35 patients showed CR, 5 patients showed PR, where, 3 were having nodal residue and 2 had disease at primary in 3DCRT arm. In IMRT arm also, 36 patients had CR, 3 patients had PR (2 with nodal disease and 1 with residual primary), and 1 had stable disease.
At 6 months after treatment completion, in the 3D-CRT arm, 34 patients had CR, 6 were in PR, where, 3 had disease at nodal region, 3 had at residual primary. In the IMRT arm, 33 patients achieved CR, 6 patients were in PR, where, 3 had nodal disease and 3 had residual primary disease, and 1 patient was in SD. The results of CR are similar, comparative and insignificant in both the arms with a p value of 0.357.
Discussion
Radiotherapy has played a significant role in the treatment of head and neck cancers. More than two-third of the head and neck carcinoma patients undergo either definitive or postoperative radiation therapy. Conventional radiotherapy is associated with significant acute as well as late toxicities, and to overcome these, newer technologies have evolved with the aim of delivering cytotoxic dose to tumor while delivering minimum dose to surrounding tissues, as shown in Figure 5 [14].
Figure 5. (A) Dose Plan of a Patient with a Laryngeal Tumor Treated with 3DCRT Using Two Opposing Fields; (B)Dose Plan of a Patient with a Laryngeal Tumor Treated with IMRT.

When compared to conventional radiotherapy, IMRT/3D-CRT techniques offer better sparing of normal tissues and thus minimizing toxicity. The IMRT technique gives the ability to create treatment fields with varying beam intensity by using inverse planning and optimization algorithms. The radiation beam can be adjusted to the irregularly shaped target volumes with extremely high precision while reducing the radiation to the surrounding healthy tissue and critical structures, like spinal cord, brain stem, optic nerve, lens, parotid glands in head and neck cancer [15].
The ability of delivering lower doses of radiation to normal tissues while maintaining or increasing the dose in the target volume makes IMRT more appropriate treatment option compared to the conventional radiotherapy [16].
In this study, we analyzed acute toxicities such as skin reactions, mucositis, dysphagia, xerostomia, nasogastric tube intubation, weight loss, nausea and vomiting in patients during the treatment duration and at the end of it in both the arms of 3D-CRT and IMRT.
In our study, we observed, 37.5% patients versus 22.5% developed grade III mucositis in the 3DCRT and IMRT group respectively (p =0.006). Grade II mucositis in 3D-CRT arm is higher than IMRT, with a p value of 0.0016. No grade IV mucositis were seen during or after treatment in any of the arms.
The study results are comparable to the randomized controlled trial done by Gupta et al. [17]. In this randomized trial between 3DCRT and IMRT in 60 patients, grade 1 and 2 mucositis were similar between the two arms but incidence of grade 3 mucositis was reduced by IMRT. In the trial, 4 of 28 patients (14.5%) in 3DCRT compared with 2 of 32 patients (6%) in IMRT developed grade 3 mucositis. In my study, 37.5% patients versus 22.5% developed grade 3 mucositis in the 3DCRT and IMRT group respectively (p =0.006).
In a retrospective study of 80 patients, Ghosh et al. [18] compared toxicity profile of IMRT with 3DCT. They found grade 3 mucositis in 34 of 40 (85%), patients versus 23 of 40 (57.5%) patients in 3DCRT and IMRT arm respectively. In my study, grade 3 and above dysphagia are in seen in treatment in the 3D-CRT arm in 2 (5%) and 6 (15%) patients respectively, where as in the IMRT arm, it was majorly seen in 6th week, in 4 patients (10%) with a p value= 0.029, suggesting a significant difference in both the arms of the study group in favor of grade III dysphagia. No grade IV dysphagia was seen during or after treatment in any of the arms. In the Ghosh et al.
[18] study statistically significant dysphagia was seen in 34 of 40 (85%) versus 23 of 40 (57.5%) patients in 3DCRT and IMRT arm respectively. In our study also incidence of grade 3 dysphagia is reduced by IMRT and at three months post-radiotherapy treatment, 8 patients (20%) versus 4 patients (10%) had grade 3 dysphagia in 3DCRT and IMRT group respectively (p = 0.029).
Our results were different from the results of randomized trial of 59 patients by Sarbani Ghosh-Laskar et al. [19]. The authors found no significant differences between 3DCRT and IMRT in incidence of mucositis and dysphagia. The probable reason of the difference in the results may be more number patients in IMRT arm of trial by Sarbani Ghosh-Laskar et al.[19] had significant portion of oral cavity receiving higher radiation dose. IMRT may not always result in less mucositis and dysphagia compared to 3DCRT. The site and size of the primary tumor and nodal disease have a significant impact on radiotherapy induced acute mucositis and dysphagia. Severe mucositis and dysphagia is expected in patients if radiation Planning Target Volume (PTV) is involving a significant portion of the oral cavity.
In our study 14 (35%) patients in 3D-CRT group had ≥10% weight loss from baseline compared to 8 (20%) patients in IMRT group. Our results were similar to the randomized trial by Sarbani Ghosh-Laskar et al. [19]. In this trial, there was a trend toward substantial weight loss during radiotherapy among patients treated with 3DCRT (11 of 29 patients; 38%) as compared to IMRT (5 of 30 patients; 16.7%; p = 0.066). Higher weight-loss of the patients can explain the higher requirement of nasogastric tube for feeding in 3DCRT group.
In our study, nasogastric tube feeding was required in 15 patients (37.5%) in the 3DCRT group versus only in 7 patients (17.5%) in the IMRT group (p = 0.003). Similarly in the trial by Sarbani Ghosh-Laskar et al., [19] 7 of 29 patients (24%) in 3DCRT arm compared to 4 of 30 patients (13%) in IMRT arm required nasogastric intubation for feeding (p = 0.284). More patients in the 3DCRT group required nasogastric tube intubation for feeding compared to IMRT group.
In our study, 3DCRT group patients had more incidence of grade 3 dermatitis (17.5% versus 7.5%) compared to IMRT group versus (p = 0.01). Grade II skin reactions also were significant with a p value of 0.008. These results are comparable to the retrospective study by Ghosh et al. [18] In this retrospective study, acute grade 3 or worse dermatitis occurred in 5 of 40 (12.5%) patients in the 3DCRT group compared with 3 of 40 (7.5%) patients in the IMRT group.
In our study at 1 month after the treatment, 11 patients had grade I and 29 patients had grade II xerostomia, while in the IMRT arm, 20 had grade I and 20 had grade II, making it significant with a p value of 0.05. At 3 months after treatment, 18 had grade I and 22 had grade II xerostomia in the 3D-CRT arm, where as in the IMRT arm 2 had grade 0, 8 had grade I and 31 had grade II of xerostomia. P=0.03. At 6 months after treatment, in the 3DCRT arm, 20 patients had grade I and 20 had grade II xerostomia, where in the IMRT arm, 4 had grade 0, 23 had grade I, and 13 had Grade II xerostomia. P=0.03.
The results are similar with results of a non-randomized, retrospective study, performed on prospectively collected data by Vergeer et al. [20] between IMRT (91 patients) and 3DCRT (150 patients). The authors found a significant difference in xerostomia in favor of IMRT in 3rd and 6th months after treatment (p-value ranging from 0.002 to 0.005).
The use of IMRT resulted in a significant reduction of the mean dose of the parotid glands (27 Gy vs. 44 Gy (p < 0.001). During radiation, grade 2 RTOG xerostomia was significantly less with IMRT than with 3D-CRT. At 6 months, the prevalence of patient-rated moderate to severe xerostomia and Grade 2 or higher RTOG xerostomia was significantly lower after IMRT versus 3D-CRT. Treatment with IMRT also had a positive effect on several general and head and neck cancer-specific QoL dimensions.
These results are similar to trial by Gupta et al., [17] where the authors concluded that the proportion of patients with grade 2 or worse acute xerostomia was significantly smaller after IMRT (19 of 32 patients, 59%) compared with 3DCRT (25 of 28 patients, 89%) (p = 0.009). Sarbani Ghosh-Laskar et al.[19] also evaluated the incidence of grade 2 or worse acute xerostomia 8 weeks after parotid- sparing radiotherapy and they found significantly lower proportion of patients with grade 2 or worse xerostomia after IMRT than after 3DCRT.
On follow up at 3 months after treatment, 35 patients showed CR, 5 patients showed PR, (3 with nodal residue and 2 with disease at primary) in 3DCRT arm. In IMRT arm also, 36 patients had CR, 3 patients had PR (2 with nodal disease and 1 with residual primary), and 1 had stable disease.
At 6 months after treatment completion, in the 3D-CRT arm, 34 patients had CR, 6 were in PR, where, 3 had disease at nodal region, 3 had at residual primary. In the IMRT arm, 33 patients achieved CR, 6 patients were in PR, where, 3 had nodal disease and 3 had residual primary disease, and 1 patient was in SD. The results of CR (p=0.357) are similar, comparative and insignificant in both the arms. In 3D-CRT arm as well as IMRT arms; Nodal site residual disease were more than the primary site, (p=0.365) indicating insignificant Partial response of both the study arms.
In summary, IMRT significantly reduced the incidence of severe mucositis, dysphagia, xerostomia, weight-loss of the patients and the requirements for nasogastric tube for feeding and it improved the treatment-compliance compared to 3DCRT in locally advanced head neck cancer patients treated by concurrent chemo-radiotherapy.
In conclusion, this prospective study was undertaken at ATRCTRI, Bikaner to estimate and compare acute toxicities like dysphagia, mucositis, dermatitis, xerostomia and hematological toxicity between the two study arms as 3D conformal radiotherapy and SIB-IMRT. It also intended to evaluate loco-regional disease response and compliance between both the arms of treatment in head and neck cancer at the end of treatment and following up to 6 months after the treatment completion. A total of 80 patients of squamous cell carcinoma of locally advanced head and neck region were taken and randomized.
The patients received radiotherapy by IMRT and 3D-CRT treatment modalities, where; 66 Gy in 30 fractions (2.2Gy/# for High risk; 1.8Gy/# for the Low-risk PTV) in the IMRT arm and 66 Gy in 33 fractions (2Gy/#) in the 3D-CRT arm. The patients in both the arms had concurrent three weekly Cisplatin administration with a dose of 100mg/m2.
The toxicity profile were noted in patients according to CTCAE v.5.0 guidelines. Observations like grade III mucositis (p =0.006), grade 3 and above dysphagia (p= 0.029), incidence of grade 3 dermatitis (p = 0.01), substantial weight loss during radiotherapy (p = 0.066) were higher in the 3D-CRT arm. Nasogastric tube feeding were more required in the 3D-CRT arm (p = 0.003).
At 1 month (p=0.05), 3 months (p=0.03) and 6 months after the treatment (p=0.03); more patients of the 3D-CRT arm had grade I and II xerostomia. The results of disease response (complete response) (p=0.357) were similar, comparative and insignificant in both the arms.
In summary, IMRT significantly reduced the incidence of severe mucositis, dysphagia, xerostomia, weight-loss in patients and the requirements for nasogastric tube for feeding as it improved the treatment-compliance compared to 3DCRT.
Our study is one of the few available prospective studies which compared the acute toxicity and compliance of 3DCRT and IMRT in locally advanced head neck cancer. We accept that our study has certain limitations also. The study lacks objective data of saliva flow rate to assess the xerostomia. Cost effectiveness and difference in quality of life between IMRT and 3DCRT were not done. It was a single institution based non-randomized study with a small number of patients. A large scale, multi-centric, randomized trial is recommended to validate the results.
References
- WHO, International Agency for Research on Cancer, Factsheet by The Global Cancer Observatory March 2023.
- WHO, International Agency for Research on Cancer/cancer topic/cancer type/head and neck cancers/global cancer observatory/infographics. .
- Freddie Bray, Mathieu Laversanne, Hyuna Sung, Jacques Farley; Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries CA Cancer Journal of Clinicians.Feb 2024;74(3).
- WHO, International Agency for Research on Cancer, GLOBOCON India 2022, Factsheet by The Global Cancer Observatory March, 2023..
- Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020 Cao W, Chen H, Yu Y, Li N, Chen W. Chinese Medical Journal.2021;134(7). CrossRef
- WHO, International Agency for Research on Cancer, GLOBOCON 2020- New Global Cancer Data 2020.
- Head and Neck Cancer Burden in India Kulkarni M. International Journal of Head and Neck Surgery.2013;4. CrossRef
- A Study of Head and Neck Cancer Patients with Reference to Tobacco Use, Gender, and Subsite Distribution Chauhan R, Trivedi V, Rani R, Singh U. South Asian Journal of Cancer.2022;11(1). CrossRef
- Major Risk Factors in Head and Neck Cancer: A Retrospective Analysis of 12-Year Experiences Dhull AK , Atri R, Dhankhar R, Chauhan AK , Kaushal V. World Journal of Oncology.2018;9(3). CrossRef
- Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium Hashibe M, Brennan P, Benhamou S, Castellsague X, Chen C, Curado MP , Dal Maso L, et al . Journal of the National Cancer Institute.2007;99(10). CrossRef
- Head and neck squamous cell carcinoma Johnson DE , Burtness B, Leemans CR , Lui VWY , Bauman JE , Grandis JR . Nature Reviews. Disease Primers.2020;6(1). CrossRef
- Cancers of the Major Salivary Gland Son E, Panwar A, Mosher CH , Lydiatt D. Journal of Oncology Practice.2018;14(2). CrossRef
- An Updated Review on Head and Neck Cancer Treatment with Radiation Therapy Anderson G, Ebadi M, Vo K, Novak J, Govindarajan A, Amini A. Cancers.2021;13(19). CrossRef
- Intensity modulated radiotherapy for head-and-neck cancer: discussing safety of modern radiation techniques Veen J, Nuyts S. Translational Cancer Research.2017;6(Suppl 6). CrossRef
- Intensity-modulated radiation therapy for head and neck cancer: systematic review and meta-analysis Marta GN , Silva V, Andrade Carvalho H, Arruda FF , Hanna SA , Gadia R, Silva JLF , et al . Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2014;110(1). CrossRef
- Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): a phase 3 multicentre randomised controlled trial Nutting CM , Morden JP , Harrington KJ , Urbano TG , Bhide SA , Clark C, Miles EA , et al . The Lancet. Oncology.2011;12(2). CrossRef
- Three-dimensional conformal radiotherapy (3D-CRT) versus intensity modulated radiation therapy (IMRT) in squamous cell carcinoma of the head and neck: a randomized controlled trial Gupta T, Agarwal J, Jain S, Phurailatpam R, Kannan S, Ghosh-Laskar S, Murthy V, et al . Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology.2012;104(3). CrossRef
- Toxicity Profile of IMRT Vs. 3D-CRT in Head and Neck Cancer: A Retrospective Study Ghosh G, Tallari R, Malviya A. Journal of clinical and diagnostic research: JCDR.2016;10(9). CrossRef
- Prospective randomized controlled trial to compare 3-dimensional conformal radiotherapy to intensity-modulated radiotherapy in head and neck squamous cell carcinoma: Long-term results Ghosh-Laskar S, Yathiraj PH , Dutta D, Rangarajan V, Purandare N, Gupta T, Budrukkar A, et al . Head & Neck.2016;38 Suppl 1. CrossRef
- Intensity-modulated radiotherapy reduces radiation-induced morbidity and improves health-related quality of life: results of a nonrandomized prospective study using a standardized follow-up program Vergeer MR , Doornaert PAH , Rietveld DHF , Leemans CR , Slotman BN , Langendijk JA . International Journal of Radiation Oncology, Biology, Physics.2009;74(1). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times