Histological Harmony: A Distinct Case of Mixed Breast Carcinoma in an Elderly Female
Download
Abstract
Background: Breast cancer is classified morphologically into “Invasive Breast Carcinoma of No Special Type” (IBC-NST) and various special subtypes. Mixed breast carcinoma, characterized by the presence of two or more distinct histological types, poses unique diagnostic challenges and is relatively rare.
Case Presentation: A 74-year-old female presented with a six-month history of a lump in her left breast, with no significant family history. Clinical examination revealed an ill-defined lump, and imaging studies indicated a BIRADS score of IV-B. Fine Needle Aspiration Cytology (FNAC) suggested proliferative breast disease with atypia. Surgical excision uncovered two tumors: Tumor 1, an invasive papillary carcinoma, and Tumor 2, exhibiting features of IBC-NST and ductal carcinoma in situ (DCIS). A subsequent Left Modified Radical Mastectomy (MRM) confirmed no residual disease in the specimen or lymph nodes.
Immunohistochemistry Results: Both tumors tested positive for estrogen and progesterone receptors and negative for HER2-neu. Tumor 2 displayed a Ki67 index of 8%, indicating low proliferation.
Conclusion: This case exemplifies the complexity of mixed breast carcinoma involving IBC-NST and invasive papillary carcinoma. It underscores the importance of histopathological and immunohistochemical analysis in accurately diagnosing and managing such cases. As mixed breast cancers constitute a small percentage of diagnoses, ongoing vigilance and collaboration among oncologists and pathologists are essential for tailored treatment approaches.
Introduction
Breast cancer is a complex and diverse group of diseases, classified morphologically into two primary categories: “Invasive Breast Carcinoma of No Special Type” (IBC-NST) and various “special subtypes.” Among these classifications, certain tumors are designated as mixed-type carcinomas, exhibiting characteristics of both IBC-NST and a special subtype. This intriguing category arises when the special subtype constitutes between 10% to 90% of the tumor composition [1].
Mixed breast carcinomas are relatively rare, presenting unique challenges in diagnosis and treatment. The nuanced distinction between IBC-NST and its special subtypes necessitates a meticulous approach, where histopathological examination becomes paramount. In this report, we present a compelling case of mixed breast carcinoma featuring both IBC-NST and invasive papillary carcinoma in an elderly female patient.
The histological analysis revealed distinct features of both components, highlighting the complexity of the tumor’s architecture. Accompanying this morphological assessment, immunohistochemical profiling provided critical insights into the tumor’s biological behavior and potential therapeutic targets. By integrating detailed histopathological findings with IHC results, we enhance our understanding of this mixed entity, underscoring the importance of precise diagnosis in guiding effective treatment strategies. This case exemplifies the essential role of pathologists in unraveling the intricate tapestry of breast cancer, ultimately contributing to improved patient outcomes.
Case Report
A 74-year-old female presented to the outpatient surgical department, with a lump in her left breast that had developed over the past six months. Notably, her medical history revealed no family predisposition to breast cancer, and she reported no associated symptoms such as inverted nipples, discharge, or skin changes. No abnormalities in biochemical and hematological parameters were observed Upon physical examination, she had an ill-defined mass measuring 5.5 x 4 cm located in both the upper inner and outer quadrants of the left breast. To further evaluate this anomaly, an ultrasound was performed, revealing a well-defined hyperechoic lesion of 3.4 x 2.3 cm with spiculated margins, positioned between the 9 and 12 o’clock positions, earning a BIRADS score of IV-B. It was next proceeded with a Fine Needle Aspiration Cytology (FNAC) which exhibited features consistent with a proliferative breast disease with atypia (Figure 1A).
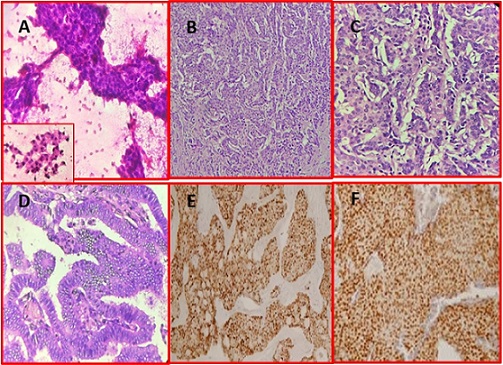
Figure 1. A – FNAC showing sheets of cohesive epithelial cells with mild to moderate nuclear atypia (H and E stain, 200x magnification), Inset showing dyscohesive cluster with mild nuclear atypia (H and E stain, 400x magnification), B – Invasive Breast Carcinoma - No special Type -Tumor cells arranged in ducts and tubules (H and E stain, 200x magnification), C –Invasive Breast Carcinoma-No special type - Tumor cells exhibiting pleomorphism and hyperchromasia (H and E stain, 400x magnification), D – Invasive Papillary Carcinoma- Tumor cells arranged in papillary structure with a central fibrovascular core (H and E stain, 200x magnification, E – IHC - PR positivity in Invasive Papillary Carcinoma component (magnification 200x), F – IHC - ER positivity in Invasive Ductal Carcinoma component (magnification 200x).
This led to the decision for a wide local excision.
Upon surgical exploration, the cut surface of the lumpectomy specimen unveiled two distinct tumors situated 0.5 cm apart. Tumor 1 was identified as a solid-cystic, grey-white mass measuring 4 x 3.5 x 2.5 cm, predominantly located in the upper inner quadrant. Histopathological examination revealed that this tumor exhibited an invasive growth pattern organized in a complex branching papillary structure with prominent fibrovascular cores (Figure 1 D). The tumor cells displayed significant pleomorphism, with round to oval nuclei.
Conversely, Tumor 2, a solid, grey-white lesion measuring 2 x 1.5 x 1.5 cm in the upper outer quadrant, presented a different profile. Microscopic assessment of this tumor revealed a ductal arrangement of neoplastic cells, demonstrating pronounced pleomorphism and hyperchromasia (Figure 1 B and C). Additionally, features of ductal carcinoma in situ (DCIS) and perineural invasion were noted, underscoring its malignancy.
Two weeks post-excision, the patient underwent a Left Modified Radical Mastectomy (MRM) coupled with axillary lymph node dissection. Examination of the MRM specimen indicated no residual tumor, with all lymph nodes appearing free of malignant deposits. Thus, a cumulative diagnosis of mpT2N0 Mixed Breast Carcinoma was established, characterized by the presence of both Invasive Breast Carcinoma of No Special Type (IBC-NST) and invasive papillary carcinoma (IPC).
Further elucidating the biological behavior of these tumors, immunohistochemical (IHC) analysis revealed that both tumors were positive for estrogen and progesterone receptors, while they tested negative for HER2-neu (Figure 1 E and F). Notably, Tumor 2 exhibited a low Ki67 proliferation index of 8%, suggesting a slower growth rate, while Tumor 1 showed additional negativity for synaptophysin and chromogranin.
This case not only highlights the complex nature of mixed breast carcinomas but also emphasizes the critical role of thorough histopathological examination and immunohistochemical profiling in guiding effective treatment strategies for patients. The patient’s journey through diagnosis and management underscores the necessity for personalized care in the realm of breast cancer, ultimately paving the way for improved patient outcomes.
Discussion
Invasive breast cancer (IBC) predominantly arises from the lining epithelium of the mammary ducts, accounting for approximately 85% of cases, with the remaining 15% stemming from the lobules, primarily the terminal duct lobular unit [2]. The World Health Organization (WHO) has established a comprehensive classification system, categorizing invasive breast carcinomas into 21 distinct histopathological types based on cellular morphology and architectural characteristics. Notably, a significant portion of breast cancer cases between 75% and 80% that were previously designated as “ductal” carcinomas have now been reclassified as “Invasive Breast Carcinoma - No Special Type” (IBC NST) [3].
Among the various histological types of breast cancer, mixed breast carcinoma presents a unique challenge. Defined by the presence of two or more distinct histologic variants, these tumors complicate both diagnosis and treatment due to their heterogeneous nature. The combination of IBC-NST with Invasive Papillary Carcinoma (IPC) in a single tumor is particularly rare, as mixed breast carcinomas featuring papillary and other histological types comprise less than 8% of all breast cancer diagnoses [4]. A study conducted by Rechsteiner et al. over a decade reported that the incidence of ductal carcinomas with papillary features is exceptionally low, estimated at only 1.31% [5]. This rarity poses significant challenges for researchers aiming to elucidate the etiopathology and clinical course of mixed breast cancers.
Given the infrequent occurrence of mixed breast carcinomas, oncological clinicians must remain vigilant for these atypical morphological combinations. Accurate diagnosis and tailored therapeutic strategies are crucial, emphasizing the importance of pathologists in analyzing and reporting histomorphological and immunohistochemical characteristics.
According to the WHO classification, IBC-NST is characterized by tumor cells organized into cords and trabeculae with varying degrees of glandular differentiation infiltrating the stroma. These tumors typically exhibit features such as nuclear pleomorphism, irregular nuclear contours, prominent nucleoli, and a variable mitotic index. The cellular architecture of IBC-NST can range from poorly differentiated tumors with significant heterogeneity to more differentiated forms that resemble normal breast tissue [6].
IPC is distinguished by its invasive growth pattern and comprises small cystic structures and papillary formations often seen in moderately dilated ducts. A key feature of IPC is the absence of myoepithelial cells at the periphery and within the papillary stalks. Although invasive papillary carcinomas are themselves rare, their prognosis is generally favorable when compared to IBC-NST [7]. Most IPCs are estrogen receptor (ER) and progesterone receptor (PR) positive and HER2 negative, classifying them within the luminal A subtype of breast cancer [8].
In this case, we present a patient diagnosed with a mixed breast carcinoma characterized by both IBC-NST and IPC. Immunohistochemical (IHC) analysis revealed positivity for estrogen and progesterone receptors and negativity for HER2, consistent with the typical profile of IPC. This profile reinforces the necessity for pathologists to carefully evaluate and report the unique characteristics of each component within mixed breast carcinomas.
The tumor exhibited distinct areas of IBC-NST, characterized by its invasive growth pattern, and regions indicative of IPC, marked by papillary structures. The IBC-NST component displayed irregular architecture with significant nuclear pleomorphism and a high mitotic rate, while the IPC areas demonstrated well-defined papillary projections. The dual presence of these components posed significant challenges for grading and treatment planning. As per WHO guidelines, tumors displaying mixed characteristics should be reported with detailed grading and biomarker status for each component separately [9]. In our case, we performed comprehensive IHC staining, allowing for an in-depth evaluation of the tumor’s heterogeneous nature. Each component was graded according to its specific histological features and
corresponding biomarker expression.
The identification of mixed breast carcinoma necessitates a nuanced approach to treatment. Given the distinct biological behavior and prognostic outcomes associated with each subtype, clinicians must tailor therapeutic strategies accordingly. For instance, the favorable prognosis of IPC may influence the decision-making process regarding adjuvant therapy, while the more aggressive features of IBC-NST may require a more intensive treatment regimen [10].
Furthermore, the rarity of mixed breast carcinomas underscores the importance of collaborative efforts among oncologists, pathologists, and researchers. Continued documentation and analysis of such cases will enhance our understanding of the complexities involved in mixed breast cancer, potentially leading to the development of more effective treatment protocols.
In conclusion, mixed breast carcinoma, particularly cases involving IBC-NST and IPC, presents significant diagnostic and therapeutic challenges. The low incidence of these tumors complicates efforts to study their etiopathology, highlighting the necessity for heightened awareness among oncological practitioners. Comprehensive histomorphological and immunohistochemical analyses are essential for accurate diagnosis and effective treatment planning.
The rarity of these tumors calls for continued research and collaboration to deepen our understanding of their biological behavior. As we report on cases like this one, we not only contribute to the existing body of knowledge but also emphasize the critical role of pathologists in guiding the clinical management of breast cancer. Through precise characterization and tailored treatment strategies, we can improve patient outcomes in this complex disease landscape.
Acknowledgments
Statement of Transparency and Principals:
• Author declares no conflict of interest
• Study was approved by Research Ethic Committee of author affiliated Institute.
• Study’s data is available upon a reasonable request.
• All authors have contributed to implementation of this research.
References
- The "Forgotten" Subtypes of Breast Carcinoma: A Systematic Review of Selected Histological Variants Not Included or Not Recognized as Distinct Entities in the Current World Health Organization Classification of Breast Tumors Koufopoulos NI , Boutas I, Pouliakis A, Samaras MG , Kotanidis C, Kontogeorgi A, Dimas DT , et al . International Journal of Molecular Sciences.2024;25(15). CrossRef
- Breast cancer. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024 Menon G, Alkabban FM , Ferguson T. .
- Dhanalakshmi Srinivasan Institute of Medical Sciences and Hospital, Thuraiyur Road, Perambalur, 621 212, Tamil Nadu, India, Jayanthi C, Srivani S, Kumaran D. Spectrum of special variants of breast carcinoma and differentiated ductal carcinomas with their immunohistochemistry profile in a tertiary care centre Manjula N. Journal of Medical Sciences and Health.2024;10(1):16-25. CrossRef
- A rare mixed breast cancer of intraductal and solid papillary with tubular carcinoma histotypes in a young woman Zhang X, Shi J, Zhou Y, Mao F, Lin Y, Guan J, Liang Z, Sun Q. Journal of Thoracic Disease.2017;9(9). CrossRef
- Prognostic relevance of mixed histological subtypes in invasive breast carcinoma: a retrospective analysis Rechsteiner A, Dietrich D, Varga Z. Journal of Cancer Research and Clinical Oncology.2023;149(8). CrossRef
- Histological and molecular classification of breast cancer: what do we know? Nascimento RG do , Otoni KM . Mastology.2020;:30. Available from: https://www.mastology.org/wp-content/uploads/2020/09/MAS_2020024_AOP.pdf.
- Papillary carcinoma of the breast: an overview Pal SK , Lau SK , Kruper L, Nwoye U, Garberoglio C, Gupta RK , Paz B, et al . Breast Cancer Research and Treatment.2010;122(3). CrossRef
- Subtypes of Breast Cancer. In: Breast Cancer Orrantia-Borunda E, Anchondo-Nuñez P, Acuña-Aguilar LE , Gómez-Valles FO , Ramírez-Valdespino CA . Exon Publications.2022;:31-42.
- What's new in breast pathology 2022: WHO 5th edition and biomarker updates Muller K, Jorns JM , Tozbikian G. Journal of Pathology and Translational Medicine.2022;56(3). CrossRef
- Advanced Approaches to Breast Cancer Classification and Diagnosis Zubair M., Wang S., Ali N.. Frontiers in Pharmacology.2020;11. CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times