Small Cell Neuroendocrine Carcinoma of the Cervix with Past History of Uterine Fibroids: A Rare Case Report
Download
Abstract
Small cell neuroendocrine carcinoma of the cervix (SCNECC) is an aggressive uterine tumor, comprising less than 2% of all cases of invasive cervical cancer. This malignancy is frequently associated with high-risk human papillomavirus (HPV) type 18. Compared to squamous cell carcinoma or adenocarcinoma, SCNECC is characterized by a significantly higher risk of both nodal and distant metastases. The scarcity of clinical trials and evidence-based treatment protocols results in a reliance on case series and individual case reports for guidance. This case report delineates a successful management strategy for SCNECC utilizing a regimen of chemotherapy in conjunction with concomitant chemoradiation therapy (CCRT) and single-channel brachytherapy.
Introduction
Small cell neuroendocrine carcinoma of the cervix (SCNECC) represents a rare neoplasm, comprising less than 2% of all invasive cervical malignancies [1]. Among the various neuroendocrine tumor subtypes of the uterine cervix, SCNECC is classified as a poorly differentiated or high-grade neuroendocrine carcinoma (NEC), characterized by its aggressive nature and unfavorable prognosis. Patients diagnosed with SCNECC exhibit nearly double the mortality risk compared to those with cervical squamous cell carcinoma [2]. The disease course is frequently marked by the emergence of extensive hematogenous metastases and recurrent locoregional disease outside the irradiated areas. Due to its rare incidence, there are no established treatment protocols for SCNECC [1]. Our case report of post-menopausal woman details an uncommon presentation of SCNECC, diagnosed via biopsy and MRI, revealing a small enhancing lesion in the left half of vaginal stump and upper vagina.
Case Report
A 55-year-old female, married for 30 years, nulliparous, with no significant co-morbidities or family history of malignancy, was referred to the Atomic Energy Cancer Hospital NORI, with the primary complaint of fresh postcoital bleeding. The bleeding was minimal (about a teaspoon), with only 2 episodes reported in a week. This patient had a hysterectomy 10 years prior due to multiple fibroids. A gynecological examination revealed a cervical mass. USG Pelvis showed a tumor involving the cervical area. Biopsy of the lesion confirmed SCNECC with a high Ki67 (>90%) (Figure 1-2).
Figure 1. H and E Slide of small cell carcinoma cervix with histological section showing malignant neoplasm comprising of sheets and nests of atypical small cells with angulated, hyperchromatic nuclei stifled chromatic and demonstrate brisk mitoses with ki67 of more than 90%.
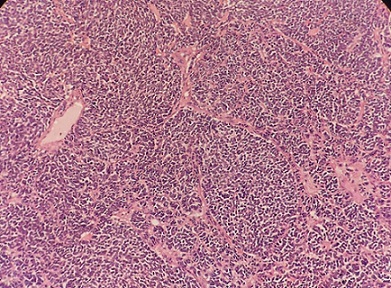
Figure 2. Ki67 proliferation index in small cell carcinoma cervix.

Immunohistochemistry showed the tumor to be synaptophysin positive and p40 negative. Following this, MRI pelvis was performed which revealed a small heterogeneously enhancing mass lesion involving the left half of the cervical/vaginal stump and upper vagina, measuring 2.9 x 2.2 cm, with parametrial extension (Figure 3) and no evidence of pelvic lymphadenopathy (FIGO stage IIB).
Figure 3. A (axial cut) and 3B (sgittal cut): Pre-treatment MRI Pelvis- An enhancing nodular lesion seen at the left side of operated vaginal stump measuring 2.9x2.2cm can be appreciated in the images.
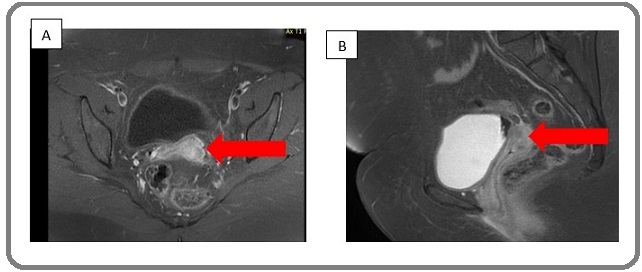
The lesion had well-defined planes with the bladder but indistinct planes with the rectum posteriorly, although the proctoscopy was normal. Metastatic workup including an MRI of the brain and contrast-enhanced computed tomography (CT) of chest, abdomen, and pelvis was negative.
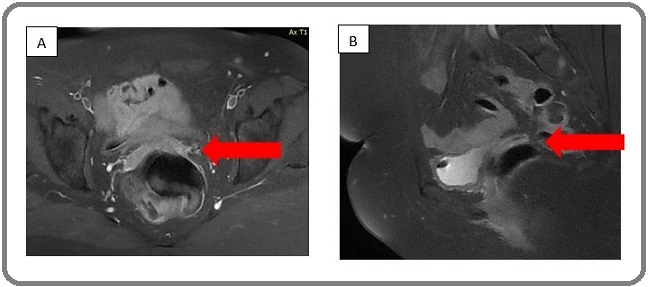
Since it was a high-grade NEC, the patient was started on a chemotherapy regimen of Intravenous (IV) etoposide (100mg/m2) and IV carboplatin with an AUC 5, both given on day 1. Each cycle was repeated after 21 days. Cisplatin was avoided due to mildly reduced renal function observed on baseline renal scan, though her eGFR was 90ml/min, allowing for safe administration of carboplatin. A total of six cycles were completed, followed by response assessment using MRI pelvis, which showed a marked reduction in the size of the lesion (Figure 4).
Figure 4. A (axial cut) and B (sgittal cut): Post 6 cycles of Carboplatin and Etoposide- the nodular lesion seen on the left side of vaginal stump had markedly regressed.
Subsequently, the patient underwent concurrent chemoradiation therapy (CCRT) to the pelvis, with a total dose of 50.4 Gy in 28 fractions (1.8 Gy per fraction). Concurrent carboplatin therapy with a weekly dose of 150mg was also administered. Prophylactic cranial irradiation (PCI) was not considered in this patient, due to lack of supporting literature regarding the added benefit of PCI and no evidence of regional or distant spread of disease. Post-CCRT, the patient was scheduled for single-channel brachytherapy, with 3 fractions of 5.5 Gy given one week post completion of CCRT on consecutive days. Following chemotherapy and radiotherapy, the patient has shown favorable progress and is under monthly follow-up. She is asymptomatic with no evidence of clinical or radiological disease.
Discussion
Cervical cancer is the fourth most prevalent cancer in women according to Globocan 2020 statistics. In Pakistan, it ranks as the third most common cancer, comprising 6.5% of all female cancers [3]. Neuroendocrine tumors of the cervix are rare, accounting for less than 5% of all cases [4]. About 80% of all cervical neuroendocrine tumors are associated with high-risk HPV [5]. In 2014, the World Health Organization categorized cervical neuroendocrine tumors into two categories: low-level (formerly known as carcinoid and atypical carcinoid) and high-level (formerly known as small cell cancer or large cell neuroendocrine cancer). Small cell neuroendocrine carcinoma cervix is classified as a high-grade carcinoma characterized by small to medium-sized cells with scant cytoplasm and neuroendocrine differentiation, which was similar in our patient as well [6]. Compared to other histological types such as adenocarcinoma and squamous cell carcinoma, small cell carcinoma exhibits a significantly higher risk of both nodal and distant metastases [7]. Common metastatic sites include the lung, liver, and bone. Approximately 75% of patients present at clinical stages I or II at diagnosis, yet metastases are frequently detected in lymph nodes even at these early stages which was contrary to our case where no regional lymphadenopathy was detected. Brain metastases mainly occur concurrently with lung metastases, but in our case MRI Brain and CT Scan Chest and Abdomen both showed no evidence of metastatic disease. The 5-year overall survival of small cell carcinoma cervix is significantly poorer, with around 30% compared to >65% for squamous cell carcinoma and adenocarcinoma of the cervix [8].
Vishwanathan et al. examined the sites of relapse and overall survival in women with neuroendocrine marker positive small cell carcinomas of the cervix. They concluded that patients with small cell neuroendocrine carcinomas of the cervix exhibit a poorer prognosis, frequently marked by the development of widespread hematogenous metastasis [9] but it was absent in our patient.
Due to the rarity of this malignancy, there is a lack of standardized treatment protocols for managing neuroendocrine tumors of the cervical region. The Society of Gynecologic Oncology published a clinical document in 2011 reviewing neuroendocrine tumors of the gynecological tract [10]. According to it, surgery is suggested as a preferred treatment for early- stage squamous cell cervical carcinoma (SCCC), followed by subsequent adjuvant chemotherapy. For patients with advanced disease or those unfit for surgical intervention, chemotherapy is recommended [8], with etoposide/ cisplatin (EP) being the preferred chemotherapy regimen. Similar treatment was employed for our patient.
A variety of studies have demonstrated that pelvic control by radical hysterectomy is not beneficial for patients with SCNECC and should be reserved for those with early invasive lesions without obvious lymph node metastasis. Conversely, non-radical hysterectomy followed by adjuvant chemotherapy is recommended [11]. In the presented case, hysterectomy was performed ten years ago due to uterine fibroids, however no tissue diagnosis was available. The nodular lesion located on the left side of vaginal stump which was surgically inoperable due to its proximity to adjacent structures; thus, systematic therapy was initiated. Radiotherapy was given to consolidate tumor control.
In conclusion, given the rarity and aggressiveness of SCNECC, it is important to treat the disease using a combination of chemotherapy and radiation. Surgical intervention should be confined to early-stage disease. SCNECC generally has a poor prognosis. Disease stage and lymph node involvement significantly impact survival outcomes, and these factors should be considered when tailoring treatment strategies.
Acknowledgments
Statement of Transparency and Principals:
• Author declares no conflict of interest
• Study was approved by Research Ethic Committee of author affiliated Institute.
• Study’s data is available upon a reasonable request.
• All authors have contributed to implementation of this research.
References
- Recent Advances in the Management of Small Cell Carcinoma of the Uterine Cervix Miyoshi A. I., Ueda Y, Kurita T, Kimura T, Yoshino K. Anticancer Research.2023;43(4). CrossRef
- Small cell neuroendocrine carcinoma of the cervix: From molecular basis to therapeutic advances Chao A, Wu R, Lin C, Chang T, Lai C. Biomedical Journal.2023;46(5). CrossRef
- Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries Sung H, Ferlay J, Siegel RL , Laversanne M, Soerjomataram I, Jemal A, Bray F. CA: a cancer journal for clinicians.2021;71(3). CrossRef
- The importance of choosing the right strategy to treat small cell carcinoma of the cervix: a comparative analysis of treatments Kawamura M, Koide Y, Murai T, Ishihara S, Takase Y, Murao T, Okazaki D, et al . BMC cancer.2021;21(1). CrossRef
- Cervical small cell carcinoma frequently presented in multiple high risk HPV infection and often associated with other type of epithelial tumors Li P, Ma J, Zhang X, Guo Y, Liu Y, Li X, Zhao D, Wang Z. Diagnostic Pathology.2018;13(1). CrossRef
- Small Cell (Neuroendocrine) Carcinoma of the Cervix: An Analysis for 19 Cases and Literature Review Lu J, Li Y, Wang J. Frontiers in Cellular and Infection Microbiology.2022;12. CrossRef
- Neoplastic Lesions of the Cervix. In: Nucci MR, Parra-Herran C, editors. Gynecologic Pathology (Second Edition) [Internet] Park KJ , Soslow RA . Philadelphia: Elsevier.2020;:227-293.
- Small cell neuroendocrine carcinoma of the cervix: a rare entity Pavithra V, Shalini C. N. S, Priya S, Rani U, Rajendiran S., Joseph LD . Journal of clinical and diagnostic research: JCDR.2014;8(2). CrossRef
- Small cell neuroendocrine carcinoma of the cervix: outcome and patterns of recurrence Viswanathan AN , Deavers MT , Jhingran A, Ramirez PT , Levenback C, Eifel PJ . Gynecologic Oncology.2004;93(1). CrossRef
- Neuroendocrine tumors of the gynecologic tract: A Society of Gynecologic Oncology (SGO) clinical document Gardner GJ , Reidy-Lagunes D, Gehrig PA . Gynecologic Oncology.2011;122(1). CrossRef
- Surgical treatment for neuroendocrine carcinoma of the uterine cervix Kasamatsu T., Sasajima Y., Onda T., Sawada M., Kato T., Tanikawa M.. International Journal of Gynaecology and Obstetrics: The Official Organ of the International Federation of Gynaecology and Obstetrics.2007;99(3). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times