A Rare Occurrence: Osseous Metaplasia in Uterine Leiomyoma: Case Study and Observations
Download
Abstract
The most common tumor of female genital tract, leiomyoma demonstrate wide spectrum of variations. However, frank osseous metaplasia or bone formation is rare. A 39-year-old woman, presented with history of menorrhagia for 6 months associated with clots and dysmenorrhea. Her general examination and bimanual exploration were normal. Gross showed myometrium with intramural fibroid, Grey/white, firm to hard area in the myometrium of size 0.4 x 0.6 cms. Microscopic findings are myometrium showing bundles and fascicles of smooth muscle cells with area of hyaline degeneration, calcification, osseous metaplasia and mild stromal infiltration by chronic inflammatory cells.
Introduction
Uterine leiomyoma is the most prevalent benign tumor of the uterus, primarily affecting women of reproductive age, with an estimated prevalence of 68.8% [1]. Although uterine fibroids are often asymptomatic, they can sometimes cause heavy and prolonged menstrual bleeding, pelvic pain, bladder disturbances, and infertility [2]. Osseous metaplasia in leiomyomas is a rare phenomenon characterized by the conversion of fibroid tissue into osteoblasts, resulting in the formation of immature or mature bone. The most common secondary degenerative changes in leiomyomas include infection, necrosis, hyaline degeneration, calcification, and myxoid degeneration. Calcified and ossified leiomyoma are uncommon and is rarely reported in literature [3]. The exact causes of heterologous tissue formation in leiomyomas are not well understood. Their histopathological characteristics are highly variable, sometimes making it difficult to differentiate between benign and malignant tumors.
Case Report
A 39-year-old woman presented with history of abdominal pain and menorrhagia. Menstrual history was normal before the event. Obstetric history was notable for two spontaneous deliveries at term, last delivery was 14 years back and patient denied of any instrumentation of uterus in the past. Her general examination and bimanual exploration were normal. Standard hematological and biochemical tests showed normal results.
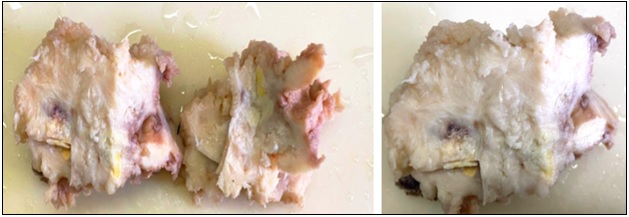
Histopathological evaluation of uterus with cervix done. Grossly we received a uterus with cervix measuring 13x6x4 cm with presence of intramural hard fibroid measuring 1x1 cm, which was gritty, hard and cut with extreme difficulty. The cut section of the mass showed yellowish hard areas (Figure 1).
Figure 1. The Gross Appearance Shows a well-defined, Gray-white Submucosal Mass with an Irregular, Cream-color- ed Area with Gritty Sensation.
Microscopic examination of Hematoxylin and Eosin stained sections, endometrium exhibits disordered proliferative endometrium with myometrium showing leiomyoma with bundles & fascicles of smooth muscle cells with areas of hyaline degeneration, calcification and osseous metaplasia with mild stromal infiltration by chronic inflammatory cells (Figure 2).
Figure 2. The H and E-stained Section of the Leiomyoma Displays Bony Trabeculae Surrounded by Hyalinized areas.
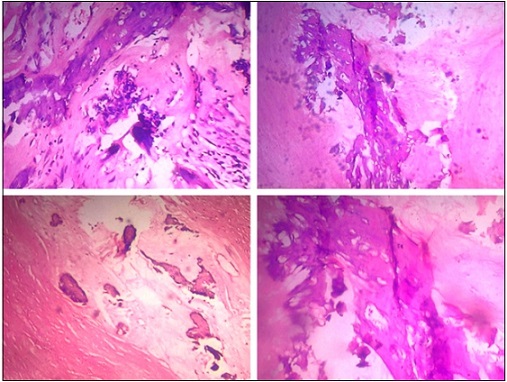
There is no evidence of granuloma/atypia /necrosis/ increased mitosis. The metaplastic nature of this condition is demonstrated morphologically through its continuity with stromal cells. Patient had no calcium disorder, her serum calcium and phosphate were in normal range, and so histopathological diagnosis of uterine leiomyoma with osseous metaplasia was made.
Discussion
Uterine leiomyomas are frequently occurring benign tumors in women. Their histopathological diagnosis is generally simple when intersecting bundles of spindle cells with eosinophilic cytoplasm and cigar-shaped nuclei with blunt ends are identified. Leiomyomas can present in different histopathological variants, including the usual type, cellular, mitotically active, atypical or plexiform, epithelioid, and myxoid leiomyoma [4]. The precise cause of uterine fibroids is not fully understood; however, various factors contribute to their growth and development. These include age, genetic predisposition, hormonal influences (estrogen and progesterone), steroids, micro-RNAs (miRNAs), cytokines, and chemokines [5]. Calcification is rare and is seen only in 8% of the cases [4]. Metaplasia results from the reprogramming of stem cells or undifferentiated mesenchymal cells, causing them to develop along a different differentiation pathway [6]. This process of differentiation is influenced by signals from cytokines, growth factors, and extracellular matrix components in the surrounding cellular environment [6]. The underlying cause of osseous metaplasia in uterine fibroids remains uncertain; however, calcification and chronic inflammation are thought to play significant roles in its pathophysiology. Various hypotheses have been proposed regarding the mechanism of ossification, including hypercalcemia, hypervitaminosis D, hyperphosphatemia, chronic endometritis, pyometra, prolonged estrogen stimulation of the endometrium, and osteogenesis [7]. It is essential for pathologists to identify the non-neoplastic nature of this condition, as it can mimic calcified leiomyomas or malignant tumors with calcification, potentially leading to diagnostic errors.
In conclusion, Leiomyomas display a diverse range of histological variations, but osseous metaplasia is an uncommon finding. While the exact cause of osseous metaplasia in uterine leiomyomas remains uncertain, calcification and chronic inflammation are thought to play significant roles in its pathophysiology. Awareness of this condition is essential for accurate diagnosis and effective management.
Acknowledgments
Statement of Transparency and Principals
• Author declares no conflict of interest
• Study was approved by Research Ethic Committee of author affiliated Institute.
• Study’s data is available upon a reasonable request.
• All authors have contributed to implementation of this research.
References
- Epidemiology of uterine fibroids: a systematic review Stewart E. A., Cookson C. L., Gandolfo R. A., Schulze-Rath R.. BJOG: an international journal of obstetrics and gynaecology.2017;124(10). CrossRef
- Uterine fibroids - what's new? Williams AR. F1000Res. 2017;6:2109 .
- Extensively ossifying oral leiomyoma: a rare histologic finding Montague LJ , Fitzpatrick SG , Islam NM , Cohen DM , Bhattacharyya I. Head and Neck Pathology.2014;8(3). CrossRef
- Osseous metaplasia in leiomyoma: A first in a uterine leiomyoma Chander B, Shekhar S. Journal of Cancer Research and Therapeutics.2015;11(3). CrossRef
- Uterine fibroids: pathogenesis and interactions with endometrium and endomyometrial junction Ciavattini A, Di Giuseppe J, Stortoni P, Montik N, Giannubilo SR , Litta , Islam MS , et al . Obstetrics and Gynecology International.2013;2013. CrossRef
- Robbins and Cotran Pathologic Basis of Disease Kumar V, Abbas AK , Fausto N, Aster JC . Elsevier.2010.
- Osseous metaplasia of the endometrium: a rare cause of infertility and its hysteroscopic management Bahçeci M., Demirel L. C.. Human Reproduction (Oxford, England).1996;11(11). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times