Management of Malignant Solitary Fibrous Tumor of Pleura-A Diagnostic Conundrum and Literature Review
Download
Abstract
Introduction and Importance-Solitary fibrous tumors are rare neoplasms originating from CD34+ dendritic stromal cells with pleural cavity as the the most common site. Majority of them are benign and 10%−20% cases are malignant. This case report contributes to the sparse literature by detailing diagnostic and therapeutic approaches, emphasizing the role of surgical resection and adjuvant therapies. Case presentation-69-year-old gentleman presented right sided chest heaviness for last 3 months. Investigations-CT scan chest revealed 13.6×13.0 x15.0cm right sided pleural based mass. Interventions and Outcome-CT guided biopsy of pleural based mass revealed solitary fibrous tumor with IHC marker positive for STAT6 and CD34. He underwent en bloc excision of mass with right upper and middle lobectomy via posterolateral thoracotomy. Patient had air leak on postoperative day 5 which was managed successfully by bronchoscopic guided glue instillation over apical lobe bronchus stump. Final histopathology showed solitary fibrous tumor with high risk of metastasis based on nuclear atypia, tumor necrosis, mitosis. Patient received adjuvant radiotherapy with the total dose of 50 Gy in 25 fractions. He is now on regular follow up every 6 monthly and is now disease from last 1 year. Relevance and Impact-Malignant solitary fibrous tumor of the pleura is a rare mesenchymal neoplasm with diagnosis primarily based on immunohistochemical study. Complete surgical resection remained the first-line treatment of MSFTP with radiotherapy reserved for patients with positive resection margin and malignant solitary fibrous tumor. Future randomized control trials are required to better understand the therapeutic approaches of this entity. This case report also highlights the successful role of bronchoscopic instillation of glue over air leak site.
Introduction
The most common site of the solitary fibrous tumor is the pleural cavity.Most of the SFTs are benign but malignant in 10%−20% of cases [1]. Non-specific clinical symptoms and imaging findings lead to difficulty in diagnosing this entity. Solitary fibrous tumors are a rare mesenchymal neoplasm that originates from CD34+ dendritic stromal cells [2-4]. The diagnosis of Malignant SFTP (MSFTP) is based on rapid growth, local invasiveness, high rates of recurrence and metastasis [2-4]. We hereby present a rare case report of malignant SFT of the pleura and review the literature on this entity. This study includes narrative review of the case reports and retrospective studies on this rare entity providing insight into the current state of knowledge and valuable insights paving a path for future research required for this rare entity.
Patient Information
A 69-year-old gentleman presented to our clinic with heaviness of chest and weight loss for the last 4 months. On further evaluation,Chest X-ray revealed large opacity in right upper side of the chest. Contrast-enhanced computed tomography scan revealed a large well-defined hypervascular enhancing soft tissue lesion with areas of internal necrosis and specs of calcification measuring 13.6× 13.0 x15.0cm predominantly involving right upper lobe bronchus and abutting adjacent pleura and right pulmonary artery (Figure 1A). Routine blood investigations including serum tumor marker levels were within normal range. Whole body PET-CT scan was performed which revealed large mildly avid mass lesion in right upper lobe abutting horizontal and oblique fissure ,laterally abutting costal pleura and medially bulging into mediastinal fat, encasing right upper lobe bronchus and abutting right pulmonary vessels.There was presence of non avid small prevascular and paratracheal nodes. There was no evidence of active disease elsewhere seen in the rest of the body (Figure 1 B).
Figure 1. A, CT scan chest showing right sided large well-defined pleural based soft tissue lesion. B, Whole body PET-CT scan showing faint FDG avid right sided lesion encasing right bronchus and abutting right pulmonary artery.

Intervention
A CT- guided transthoracic core biopsy of the mediastinal mass was performed, which revealed oval to spindle tumor cells having hyperchromasia and high N:C ratio with focal areas of hyalinization (Figure 2A).
Figure 2. A, Microscopic appearance showing oval spindle cells with hyperchromasia. B, Tumor cells positive for CD99 + marker. C, Post operative biopsy shows microscopic image with high Ki-67 index.

On subsequent IHC studies,the tumor cells were found to have strong positivity for STAT 6, CD34, CD 99,vimentin and negative for S100 and CK (Figure 2B). Final diagnosis favors the fibroblastic tumor with prominent staghorn vasculature consistent with solitary fibrous tumor. Case was discussed in multidisciplinary tumor board where plan for surgical excision of mass was taken.Patient was optimized for surgery and he subsequently underwent right posterolateral thoracotomy with excision of the mass along with right upper and middle lobectomy of lung as the large mass was densely adhered to right upper bronchus, superior pulmonary vein and upper lobe branches of right main pulmonary artery (Figure 3A, 3B).
Figure 3. A, Images showing intraoperative images of large right pleural based lesion adhered to right upper and middle lobe and parietal pleura. B, Resected mass with right bilobectomy.

Operative steps
After placing double lumen tube under general anaesthesia,patient was positioned in lateral position. After proper paint and draping, right posterolateral thoracotomy incision was made and pleural space was entered through 5th intercostal space. Operative findings were confirmed. The large pleural based mass was mobilized all around the parital pleura, apex and from inferior pulmonary ligament. It was a sessile mass adhering to right upper bronchus, superior pulmonary vein and upper lobe branches of right main pulmonary artery (Figure 3A). With the utilization of sharp dissection and after defining interlobar fissure,right upper and middle bilobectomy was performed as the upper and middle lobe bronchus were adhered to the tumor. Similarly, superior pulmonary vein was divided with vascular stapler. Finally, upper lobe branches from right pulmonary artery were divided. Intraoperative frozen section of bronchial cut margin was sent and was found negative for the tumor. Two intercostal drains were placed after achieving hemostasis and confirming adequate right lower lobe expansion.Wound was closed with ethibond sutures for rib approximation and skin staplers were applied.
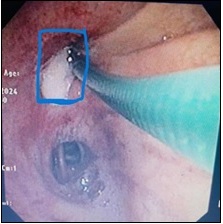
Patient was shifted to Intensive care unit and was monitored there for 2 days. He was allowed oral diet from POD1 (postoperative day) and was started on incentive spirometry. He was started on chest physiotherapy and was made ambulatory on POD2. Serial post operative chest x ray revealed adequate right lung expansion but on POD5 there was presence of air leak in the intercostal drain and chest X ray revealed small apical pneumothorax in right side of chest with partial collapse of right lower lobe. His vitals remained stable with SPO2 remained above 95%. Decision to convert intercostal drain to negative suction pleural drainage with pleur-evac was done with negative suction settings of -20 atmospheric pressure. There was slight reduction in the volume of air leak, Chest X ray showed reduction in pneumothorax but there was fall of SPO2 to 90% on POD7 for which pulmonology consultation was sought for. CT chest was performed which revealed partial right lung collapse with no septal thickening. Patient’s consent was taken for bronchoscopic guided glue instillation at the bronchial stump leak site as it has shown to be an effective method for managing bronchial stump air leaks. Bronchoscopy was performed which revealed air leak in apical segment stump of right upper bronchus.Bronchoscopic guided glue instillation over leak site was performed precisely by our pulmonology team (Figure 4).
Figure 4. Bronchoscopic Guided Glue Instillation Over Bronchial Leak Site.
The air leak resolved and chest X ray shows normally expanded lung in the post-procedure period. There was no evidence of air leak in intercostals drains. He was discharged on POD 10 after the removal of the intercostals drains. Final histopathological evaluation of tumor revealed well circumscribed mass of size 22x20x11cm with areas of tumor necrosis on cut section of tumor. Microscopically,it revealed proliferation of spindle shaped cells attached to pleural bands with staghorn vasculature. There was moderate nuclear atypia and tumor necrosis was seen. Mitotic activity was 4-5/10 HPF. Resection margins were negative for tumor.On Immunohistochemistry (IHC), the tumor cells were positive for CD34,STAT 6 and CD 99 (strongly and diffusely). The ki-67 index in the tumor cells was 10% in the final biopsy (Figure 2C). Hence, final diagnosis of solitary fibrous tumor with high risk of metastasis was made. Case was discussed in multidisciplinary tumor board and patient was advised adjuvant radiotherapy 50Gy in 25 fractions during subsequent follow up visit. He is on now on regular follow up and is now disease free from last 1 year.
Discussion
SFTP was originally considered as a rare tumor and had several nomenclature like solitary fibrous mesothelioma,localized mesothelioma, submesothelial fibroma, and pleural fibroma. Finally it was established that SFTP originates from CD34+ dendritic stromal cells [4]. SFTP accounts for less than 5% of all pleural tumors with 80% of them originating from the visceral pleura [5]. The peak incidence rate is 50-70 years with slight female predilection [6]. Majority of SFTPs are benign with generally good prognosis following surgery while about 10%−20% of SFTPs are malignant [1]. The etiology of MSFTP is still unclear with no association found with the smoking, radiation, asbestos or other toxic substances while a family cancer history may be a risk factor for MSFTP [7]. Clinical symptoms are more commonly seen in MSFTP patient compared to benign SFTP (58% vs. 23%) [5]. It has been stated that high-grade malignant SFT developed after transformation of benign or low-grade malignant SFT while another hypothesis stated malignant SFT arising de novo [8]. Studies have investigated the role of genetic polymorphisms in association with cancer risk and similarly future research should be performed to explore genetic factors association in MSFTP patients [9]. It has been shown in a study which highlighted the challenges faced in cancer detection in elderly populations especially in rare tumors [10]. Therefore,future studies should emphasize the need for improved screening and diagnostic strategies in this rare entity.At present,to screen MSFTP patients with high recurrence risk,various risk prediction models are used based on biological and histopathological characteristics [11]. According to World Health Organization classification for soft tissue tumors, SFT was classified as a fibroblastic/myofibroblastic tumor [12]. The diagnosis of MSFTP has been suggested if any one of the following criteria is met: (1) a high mitotic rate (at least 4 mitotic figure counts per 10 high-power fields), (2) increased cellularity, (3) necrosis or hemorrhage, and (4) cellular and nuclear pleomorphism [4, 13, 14]. In our case too, final diagnosis of malignant SFTP was made on these features of invasiveness, necrosis,mitosis and Ki-67 index of 10%.The nerve growth factor-induced gene A binding protein 2 (NAB2) - signal transducer and activator of transcription 6 (STAT6) fusion gene is considered as specific molecular marker for SFT and facilitate its diagnosis [15, 16]. Contrast enhanced Computed tomography (CT) is the preferred modality for preoperative workup of MSFTP to assess the size, location and relation of tumor with the adjacent structures as well as in identifying the feeding vessels of the tumor, which aids in management decision on MSFTP. MSFTP features heterogeneous density on non-enhanced CT. Cystic changes, myxoid degeneration, hemorrhage, and necrosis may be seen within the lesion,calcification may also be seen in sufficiently large MSFTP with pleural effusions in some cases. Distant metastasis has been reported in MSFTP commonly in lungs, bones, liver, pancreas, thyroid gland, urinary bladder, central nervous system, and reproductive system with a dismal prognosis similar to malignant mesothelioma with metastasis [17-20]. The site of distant metastasis may vary depending upon the primary site of MSFT [17]. The use of 18F-Fluorodeoxyglucose positron emission tomography (18F-FDG PET /CT) lies in its ability to obtain both functional and morphological information, which can further aid the diagnosis, staging, and predicting prognosis in SFTP patients. CT guided percutaneous fine needle aspiration biopsy is a commonly performed procedure for the diagnosis and grading these tumors. Histopathologically, MSFTP often presents with large mass with varying degrees of necrosis and hemorrhage with histological examination showing spindle-shaped, fibroblast-like tumor cells with staghorn-shaped vessels,atypical mitotic figures, necrosis. Complete surgical excision remains the standard treatment to treat these entities [7, 21]. Intraoperative frozen section has a definitive role in all SFTPs to determine the nature of the tumor and tumor margin assessment. Therefore, the gold standard for the surgical treatment of MSFTP is still with thoracotomy [21]. However,the surgical procedure of VATS remained feasible option for pedunculated tumors and well demarcated tumors with advantage of reduced postoperative pain and early recovery [7, 22]. While lobectomy remained the procedure of choice for large sessile tumors originating from the visceral pleura and extending into lung parenchyma. For malignant tumors that have invaded lung parenchyma, chest wall, pericardium, and diaphragm, extended resection when necessary would be a feasible option [7]. The post operative complication of air leaks can be managed by standard bronchoscopic guided glue instillation over bronchial stump leak site with good outcomes as we have utilized this technique in our case too with successful outcome.Adjuvant radiotherapy after complete tumor resection is not recommended in patients with benign SFTP. Adjuvant radiotherapy (50Gy in 25 fractions) can be considered in patients with a positive surgical margin, tumor recurrence, or MSFTP [23]. However, benefits of radiotherapy is still unclear given the small sample size and short follow up time in the studies and also due to lack of randomized clinical trials. Therefore, the application of radiotherapy in MSFTP patients should be decided on an individual basis following multidisciplinary discussion. In our case, after multidisciplinary tumor board discussion, we adjuvant radiotherapy with the dose of 50 Gy in 25 fractions was advised on the basis of the presence of features of high risk of metastasis in the final histopathology report of the tumor. The efficacy of chemotherapy in SFT treatment is undetermined [24-32]. Conventional chemotherapeutic drugs for soft tissue sarcoma may include anthracyclines and ifosfamide, but their efficacy for this entity is largely unknown. A retrospective study in Europe reported that anthracyclines may be effective in the adavanced SFT treatment [31]. Temozolomide combined with bevacizumab have shown some efficacy in retrospective studies. But most studies have found conventional chemotherapy to be ineffective in SFT treatment [30, 33]. Molecularly targeted therapy that inhibits vascular endothelial growth factor or other tyrosine kinase inhibitors pathways has shown some positive prospects for the treatment of advanced SFT (Table 1) [24, 25] [34, 35].
| Studies | Type of study | Tumor and number of patients | Type of therapy | ORR (number of patients) | mPFS (Months) | Year of study | Study limitations |
| Outani et al. [22] | Retrospective | Total -60 | Anthracycline- based (11) | 3 | 2021 | Retrospective study | |
| MSFT-35 | Gemcitabine− docetaxel (10) | 8 | |||||
| Ifosfamide- based (7) | - | 2 | |||||
| Trabectedin (6) | 3.5 | ||||||
| Eribulin (4) | 8 | ||||||
| Pazopanib (22) | 6.5 | ||||||
| Levard et al. [23] | Retrospective | Advanced SFT-23 | Doxorubicin- based (19) | 2 patients | 5.2 | 2013 | Retrospective study |
| Vinorelbine (1) | |||||||
| Paclitaxel (1) | |||||||
| Carboplatin and paclitaxel (1) | |||||||
| Brostallicin (1) | |||||||
| In 2 nd , 3 rd or 4 th line: | |||||||
| Pazopanib (6) | |||||||
| Sunitinib (4) | 5.1 | ||||||
| Stachiotti et al. [24] | Retrospective | MSFT -7 | Doxorubicin + Dacarbazine | 6 patients | 6 | 2017 | Low number of cases |
| DSFT-5 | 10 | ||||||
| Khalifa et al. [25] | Retrospective | All -11 | Trabectedin | 1 patient | 11.6 | 2015 | Low number of cases and retrospective study |
| MSFT-10 | |||||||
| Park et al. [26] | Retrospective | Advanced SFT-21 | Doxorubicin- based (15) | - | 4.6 | 2013 | Retrospective study with low case numbers |
| Gmcitabine- based (5) | |||||||
| Paclitaxel (5) | |||||||
| Stachiotti et al. [27] | Retrospective | MSFT -3 | Dacarbazine | 3 patients | 7 | 2013 | Retrospective study |
| DSFT-5 | |||||||
| DeVito et al. [28] | Retrospective | SFT -21 | Ifosfamide (10) | 2015 | No data on PFS | ||
| MSFT-16 | Taxane based (3) | - | - | ||||
| Multiple regimens (9) | |||||||
| Other (5) | |||||||
| Stachiotti et al. [29] | Retrospective | All -30 | Anthracyclines | -6 | 4 | 2013 | Retrospective study |
| MSFT -17 | -2 | 3.5 | |||||
| DSFT-12 | -4 | 5 | |||||
| Chaigneau et al. [30] | Case Report | MSFT-1 | Trabectedin | 1 | 8 | 2011 | Only case report-insufficient |
| Javier et al. [32] | Phase II trial | All -36 | Pazopanib | 2 | 5.6 | 2019 | Phase III trials required with large number of patients enrollment |
| MSFT -34 | |||||||
| DSFT-02 | |||||||
| Stacchiotti et al. [33] | Retrospective | MSFT -3 | Pazopanib | 0 | 3 | 2014 | Low number of cases and retrospective study |
MSFT-Malignant solitary fibrous Tumor, mPFS-Median progression free survival, ORR-overall response rate.
Also retrospective studies have found bevacizumab, sunitinib, and pazopanib to be effective in soft tissue sarcoma treatment. Pazopanib has been approved for the treatment of soft tissue sarcoma and it improved the prognosis of advanced SFT patients in an Europian multicenter, single-arm phase II trial [34]. Meanwhile, sunitinib and sorafenib are in phase II clinical trials for the treatment of soft tissue sarcoma. In addition, axitinib may also be effective in the treatment of non-dedifferentiated SFT [34, 36]. Future studies should be done to explore the novel therapeutic agents to improve better responses and survival rates in this rare entity [37]. In general, benign SFTP has a good prognosis. In a single-center, retrospective study by Zhou,the 5-year overall survival rate of 70 benign SFTP patients was 100% [38]. In another retrospective study, the 5-year survival rate was 88.9%, and the median survival time was 23.7 years for 84 benign SFTP patients [39]. However,the risk of local recurrence and malignant transformation is always present.Hence the long-term follow- up is required in these MSFTP cases to ascertain the quality of life in this rare entity [40].
Large-scale studies have found that the 10-year recurrence rate of SFTP is about 10%−25%, and incomplete tumor resection is the most important risk factor for recurrence [40]. As for MSFTP, the rates of disease-free survival (DFS) and overall survival (OS) were much lower. In Zhou’s study, rates of 5-year DFS and OS in MSFTP patients were 58.3% and 66.7%, respectively while another retrospective study among benign SFT patients, the 5-year survival rate was 88.9% [38-39].
The limitation of this study - It is a case report and further future studies in the form of randomized controlled trials are required to know appropriate adjuvant therapies and its sequencing for this rare entity.
In conclusion, MSFTP is a rare mesenchymal neoplasm with unclear etiology till date. Clinical manifestations of MSFTP include non-specific symptoms such as chest pain, hemoptysis and dyspnea with imaging findings of MSFTP being largely non-characteristic.This case report highlights the importance of immunohistochemical markers and multidisciplinary management with the role of surgery and radiotherapy in improving outcomes of this rare malignancy requiring future randomized control trials to better understand the therapeutic approaches of this entity.This case report also highlights the successful role of bronchoscopic instillation of glue at the air leak site in an otherwise stable patient.
Acknowledgments
Statement of Transparency and Principals:
• Author declares no conflict of interest
• Study was approved by Research Ethic Committee of author affiliated Institute.
• Study’s data is available upon a reasonable request.
• All authors have contributed to implementation of this research.
References
- Predictors of behaviour in solitary fibrous tumours of the pleura surgically resected: Analysis of 107 patients Bellini A, Marulli G, Breda C, Ferrigno P, Terzi S, Lomangino I, Lo Giudice F, et al . Journal of Surgical Oncology.2019;120(4). CrossRef
- Atypical and malignant solitary fibrous tumors in extrathoracic locations: evidence of their comparability to intra-thoracic tumors Vallat-Decouvelaere A. V., Dry S. M., Fletcher C. D.. The American Journal of Surgical Pathology.1998;22(12). CrossRef
- Malignant giant solitary fibrous tumor of the pleura metastatic to the thyroid gland Ricciuti B, Metro G, Leonardi GC , Sordo RD , Colella R, Puma F, Ceccarelli S, et al . Tumori.2016;102(Suppl. 2). CrossRef
- Solitary Fibrous Tumor - Less Common Neoplasms of the Pleural Cavity Vejvodova S, Spidlen V, Mukensnabl P, Krakorova G, Molacek J, Vodicka J. Annals of Thoracic and Cardiovascular Surgery: Official Journal of the Association of Thoracic and Cardiovascular Surgeons of Asia.2017;23(1). CrossRef
- Solitary fibrous tumor of the pleura: outcomes of 157 complete resections in a single center Lahon B, Mercier O, Fadel E, Ghigna MR , Petkova B, Mussot S, Fabre D, Le Chevalier T, Dartevelle P. The Annals of Thoracic Surgery.2012;94(2). CrossRef
- Solitary fibrous tumour of pleura: CT differentiation of benign and malignant types Gupta A., Souza C. A., Sekhon H. S., Gomes M. M., Hare S. S., Agarwal P. P., Kanne J. P., Seely J. M.. Clinical Radiology.2017;72(9). CrossRef
- Solitary fibrous tumors of the pleura: A single center experience at National Cancer Center, China Tan F, Wang Y, Gao S, Xue Q, Mu J, Mao Y, Gao Y, et al . Thoracic Cancer.2018;9(12). CrossRef
- Solitary fibrous tumour: significance of p53 and CD34 immunoreactivity in its malignant transformation Yokoi T., Tsuzuki T., Yatabe Y., Suzuki M., Kurumaya H., Koshikawa T., et al . Histopathology.1998;32(5). CrossRef
- Alteration of the Risk of Oral Pre-Cancer and Cancer in North India Population by CYP1A1 Polymorphism Genotypes and Haplotype Nigam K, Sanyal S, Gupta S, Gupta OP , Mahdi AA , Bhatt M. L. B.. Asian Pacific journal of cancer prevention: APJCP.2019;20(2). CrossRef
- Utilization of Colorectal Cancer Screening among Saudi Elderly Population: A Study from the Saudi National Survey for Elderly Health Khoja A, Aljawadi M, Al-Shammari SA , Bokhari NN , Aldarwish AA , Mardini WK , Khoja TK . Asian Pacific journal of cancer prevention: APJCP.2018;19(12). CrossRef
- Comparison of Risk Stratification Models to Predict Recurrence and Survival in Pleuropulmonary Solitary Fibrous Tumor Reisenauer JS , Mneimneh , Jenkins , Mansfield AS , Aubry MC , Fritchie KJ , Allen MS , et al . Journal of Thoracic Oncology: Official Publication of the International Association for the Study of Lung Cancer.2018;13(9). CrossRef
- The new WHO classification and recent results in soft tissue tumor pathology Petersen I. Der Pathologe.2013;34(5). CrossRef
- Localized benign and malignant fibrous tumors of the pleura. A clinicopathologic review of 223 cases England D. M., Hochholzer L., McCarthy M. J.. The American Journal of Surgical Pathology.1989;13(8). CrossRef
- Prediction of local and metastatic recurrence in solitary fibrous tumor: construction of a risk calculator in a multicenter cohort from the French Sarcoma Group (FSG) database Salas S., Resseguier N., Blay J. Y., Le Cesne A., Italiano A., Chevreau C., Rosset P., et al . Annals of Oncology: Official Journal of the European Society for Medical Oncology.2017;28(8). CrossRef
- Research progress of NAB2-STAT6 fusion gene in solitary fibrous tumor/ hemangiopericytoma chin Zhu H. J Clin Neurosci .2014;22(3):335-339.
- [Expression and significance of STAT6 in solitary fibrous tumor] Ding Z. Y., Wang Y. F., Wang X., Rao Q.. Zhonghua Bing Li Xue Za Zhi = Chinese Journal of Pathology.2017;46(4). CrossRef
- Malignant solitary fibrous tumor of the kidney with liver metastasis: A case report and literature review Zhang N, Zhou D, Chen K, Zhang H, Huang B. Journal of Cancer Research and Therapeutics.2018;14(Supplement). CrossRef
- Extrapleural solitary fibrous tumor: A distinct entity from pleural solitary fibrous tumor. An update on clinical, molecular and diagnostic features Ronchi A, Cozzolino I, Zito Marino F, Accardo M, Montella M, Panarese I, Roccuzzo G, et al . Annals of Diagnostic Pathology.2018;34. CrossRef
- Synchronous pancreatic and pulmonary metastases from solitary fibrous tumor of the pleura: report of a case Tamburini N, Fabbri N, Anania G, Maniscalco P, Quarantotto F, Rinaldi R, Cavallesco G. Tumori.2017;103(Suppl. 1). CrossRef
- Survival in Good Performance Malignant Pleural Mesothelioma Patients; Prognostic Factors and Predictors of Response Rahouma M, Aziz H, Ghaly G, Kamel M, Loai I, Mohamed A. Asian Pacific journal of cancer prevention: APJCP.2017;18(8). CrossRef
- Malignant solitary fibrous tumors of the pleura: retrospective review of a multicenter series Lococo F, Cesario A, Cardillo G, Filosso P, Galetta D, Carbone L, Oliaro A, et al . Journal of Thoracic Oncology: Official Publication of the International Association for the Study of Lung Cancer.2012;7(11). CrossRef
- Solitary fibrous tumors of the pleura: clinical characteristics, surgical treatment and outcome Magdeleinat P, Alifano M, Petino A, Le Rochais JP , Dulmet E, Galateau F, Icard P, Regnard JF . European Journal of Cardio-Thoracic Surgery: Official Journal of the European Association for Cardio-Thoracic Surgery.2002;21(6). CrossRef
- Thoracic malignant solitary fibrous tumors: A population-based study of survival Milano MT , Singh DP , Zhang H. Journal of Thoracic Disease.2011;3(2). CrossRef
- Clinical Outcomes of Patients with Metastatic Solitary Fibrous Tumors: A Japanese Musculoskeletal Oncology Group (JMOG) Multiinstitutional Study Outani H, Kobayashi E, Wasa J, Saito M, Takenaka S, Hayakawa K, Endo M, et al . Annals of Surgical Oncology.2021;28(7). CrossRef
- Outcome of patients with advanced solitary fibrous tumors: the Centre Léon Bérard experience Levard A, Derbel O, Méeus P, Ranchère D, Ray-Coquard I, Blay J, Cassier PA . BMC cancer.2013;13. CrossRef
- Patient-derived solitary fibrous tumour xenografts predict high sensitivity to doxorubicin/dacarbazine combination confirmed in the clinic and highlight the potential effectiveness of trabectedin or eribulin against this tumour Stacchiotti S., Saponara M., Frapolli R., Tortoreto M., Cominetti D., Provenzano S., Negri T., et al . European Journal of Cancer (Oxford, England: 1990).2017;76. CrossRef
- Efficacy of trabectedin in malignant solitary fibrous tumors: a retrospective analysis from the French Sarcoma Group Khalifa J., Ouali M., Chaltiel L., Le Guellec S., Le Cesne A., Blay J.-Y., Cousin P., et al . BMC cancer.2015;15. CrossRef
- The role of chemotherapy in advanced solitary fibrous tumors: a retrospective analysis Park MS , Ravi V, Conley A, Patel SR , Trent JC , Lev DC , Lazar AJ , et al . Clinical Sarcoma Research.2013;3(1). CrossRef
- Dacarbazine in solitary fibrous tumor: a case series analysis and preclinical evidence vis-a-vis temozolomide and antiangiogenics Stacchiotti S., Tortoreto M., Bozzi F., Tamborini E., Morosi C., Messina A., Libertini M., et al . Clinical Cancer Research: An Official Journal of the American Association for Cancer Research.2013;19(18). CrossRef
- Clinical Characteristics and Outcomes for Solitary Fibrous Tumor (SFT): A Single Center Experience DeVito N, Henderson E, Han G, Reed D, Bui MM , Lavey R, Robinson L, et al . PloS One.2015;10(10). CrossRef
- Response to chemotherapy of solitary fibrous tumour: a retrospective study Stacchiotti S., Libertini M., Negri T., Palassini E., Gronchi A., Fatigoni S., Poletti P., et al . European Journal of Cancer (Oxford, England: 1990).2013;49(10). CrossRef
- Efficacy of trabectedin in metastatic solitary fibrous tumor Chaigneau L, Kalbacher E, Thiery-Vuillemin A, Fagnoni-Legat C, Isambert N, Aherfi L, Pauchot J, et al . Rare Tumors.2011;3(3). CrossRef
- Conventional anthracycline-based chemotherapy has limited efficacy in solitary fibrous tumour Constantinidou A, Jones RL , Olmos D, Thway K, Fisher C, Al-Muderis O, Judson I. Acta Oncologica (Stockholm, Sweden).2012;51(4). CrossRef
- Pazopanib for treatment of advanced malignant and dedifferentiated solitary fibrous tumour: a multicentre, single-arm, phase 2 trial Martin-Broto J, Stacchiotti S, Lopez-Pousa A, Redondo A, Bernabeu D, Alava E, Casali PG , et al . The Lancet. Oncology.2019;20(1). CrossRef
- Preclinical and clinical evidence of activity of pazopanib in solitary fibrous tumour Stacchiotti S., Tortoreto M., Baldi G. G., Grignani G., Toss A., Badalamenti G., Cominetti D., et al . European Journal of Cancer (Oxford, England: 1990).2014;50(17). CrossRef
- Activity of temozolomide and bevacizumab in the treatment of locally advanced, recurrent, and metastatic hemangiopericytoma and malignant solitary fibrous tumor Park MS , Patel SR , Ludwig JA , Trent JC , Conrad CA , Lazar AJ , Wang W, et al . Cancer.2011;117(21). CrossRef
- Cytotoxic and Antiproliferative Activity of Polyisoprenoids in Seventeen Mangroves Species Against WiDr Colon Cancer Cells Sari DP , Basyuni M, Hasibuan PA , Sumardi S, Nuryawan A, Wati R. Asian Pacific journal of cancer prevention: APJCP.2018;19(12). CrossRef
- Thoracic solitary fibrous tumors: an analysis of 70 patients who underwent surgical resection in a single institution Zhou C, Li W, Shao Ji, Zhao J. Journal of Cancer Research and Clinical Oncology.2020;146(5). CrossRef
- Solitary fibrous tumors of the pleura: results of surgical treatment and long-term prognosis Harrison-Phipps KM , Nichols FC , Schleck CD , Deschamps C, Cassivi SD , Schipper PH , Allen MS , Wigle DA , Pairolero PC . The Journal of Thoracic and Cardiovascular Surgery.2009;138(1). CrossRef
- A Critical Review of Instruments Measuring the Quality of Life of Cancer Patients in Iranian Studies and Their Psychometrics Properties Hasanvand S, Rassouli M, Mandegari Z, Salmani N, Moghimkhan F. Asian Pacific journal of cancer prevention: APJCP.2019;20(2). CrossRef
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright
© Asian Pacific Journal of Cancer Care , 2025
Author Details
How to Cite
- Abstract viewed - 0 times
- PDF (FULL TEXT) downloaded - 0 times
- XML downloaded - 0 times